Playlist
Show Playlist
Hide Playlist
Ventricular (VT) & Supraventricular (SVT) Tachycardia
-
Emergency Medicine Tachyarrhythmia.pdf
-
Download Lecture Overview
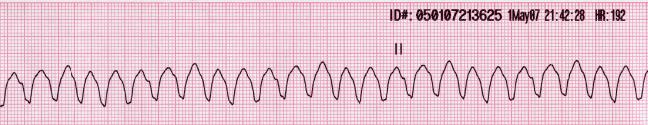
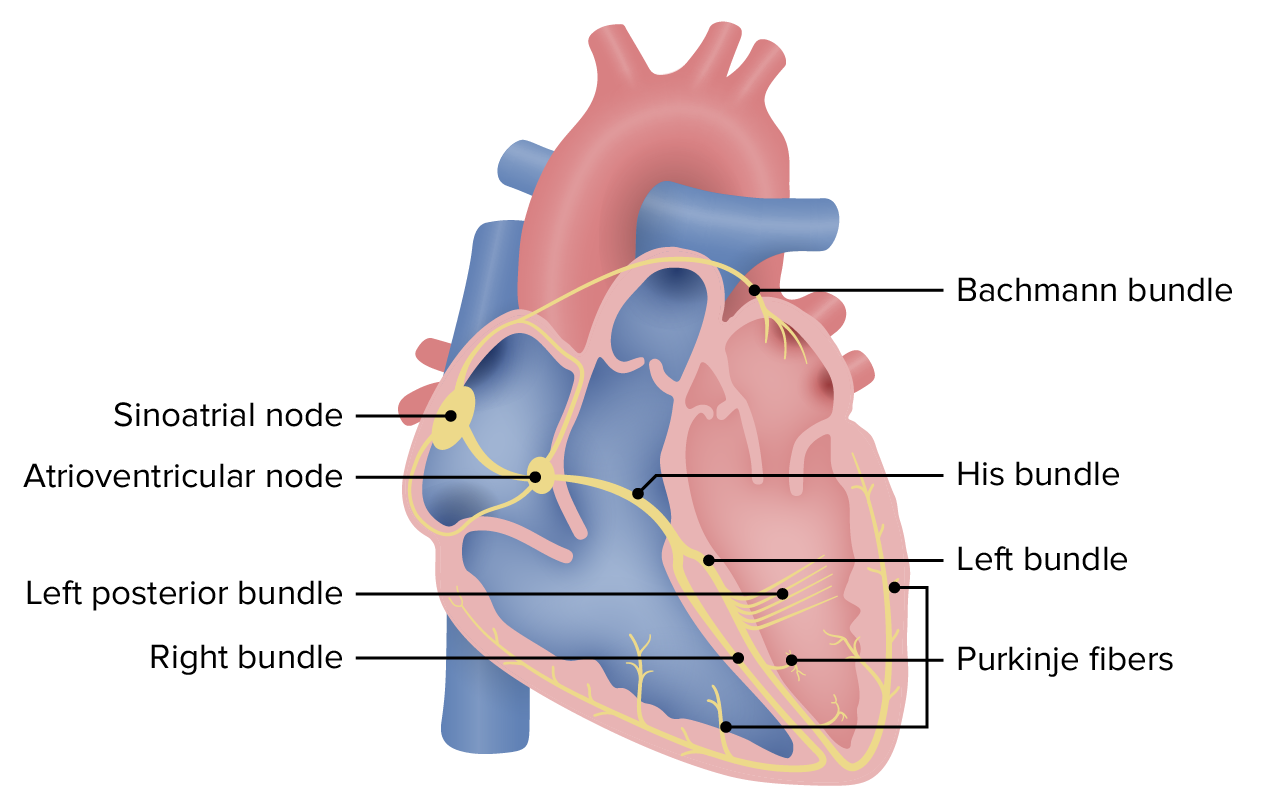
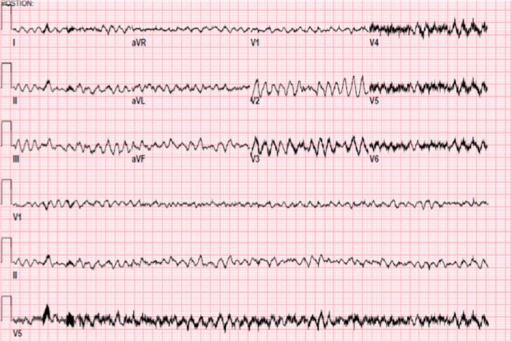
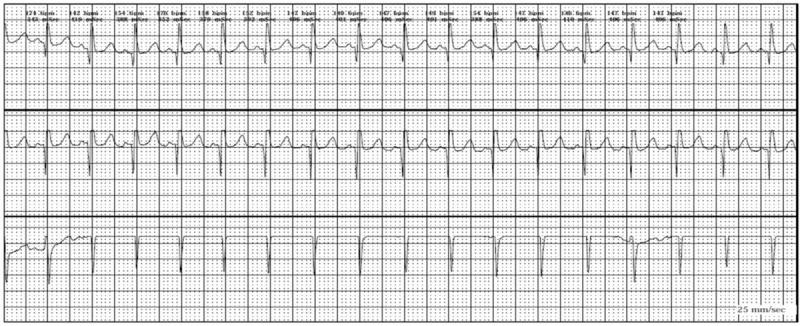
00:01 So really, when we think about wide complex rhythms, we wanna think about whether the patient is in ventricular tachycardia or supraventricular tachycardia with aberrant conduction. 00:13 And there are some clinical features that will help us distinguish between the two. 00:18 So, older patients are much more likely to be in V-tach compared to younger patients. 00:24 Patients with a history of heart disease, either ischemic heart disease, heart failure, cardiomyopathy, again, more likely to be having a ventricular dysrhythmia and definitely patients who have a family history for ventricular rhythm disturbance, again, are more likely to be in V-tach. 00:41 On the ECG, there are a number of different features that you can look for and we’re not gonna cover them in a lot of detail here but you can look for AV dissociation, fusion or capture beats, extreme axis deviation, QRS concordance, or Brugada’s sign which is defined as a hundred milliseconds from the QRS complex to the bottom of the S wave. 01:05 In other words, prolongation of that latter part of the QRS complex. 01:10 The bottom-line is that these things are really interesting to think about and talk about, and they make for good conversation on rounds, but ultimately, it’s very, very difficult to reliably differentiate between V-tach and supraventricular tachycardia with aberrancy. 01:27 There are a lot of different criteria that people use for this. 01:30 There’s the Brugada criteria, the modified Brugada criteria, there’s a whole bunch of different ones. 01:36 But none of them has been shown to be completely reliable in clinical practice and therefore, they’re not completely safe to use in clinical practice. 01:44 So, this is a pearl for you, pay attention. 01:47 The bottom-line is that all wide-complex tachycardia should be assumed to be V-tach until proven otherwise. 01:56 It’s very difficult to differentiate between V-tach, and supraventricular tachycardia with aberrant conduction on clinical grounds, so when in doubt, assume that it’s V-tach, and you’ll be safe. 02:09 Now, why is this so important? Well, very simply, V-tach is a life-threatening rhythm disturbance and you have to treat it aggressively where supraventricular tachycardia is more benign and you don’t have to be quite as assertive with your management. 02:25 More importantly, ventricular tachycardia’s not gonna respond to the kinds of treatments that we use for supraventricular rhythms. 02:33 So you’re not gonna be effective in treating V-tach if you’re trying to treat it like a supraventricular rhythm. 02:40 But the most important thing is that in some situations, use of medications that are designed for supraventricular rhythms can actually be harmful in certain situations in wide-complex tachycardia. 02:55 You can actually kill patients by treating their wide-complex tachycardia as though it is supraventricular in origin, and let’s talk about an example of that. 03:06 So, Wolff-Parkinson-White is one condition where it’s very, very dangerous to use AV nodal blocking agents which are used for supraventricular rhythms to try to terminate wide-complex tachycardia. 03:19 So, in patients with WPW, there are two conduction pathways. 03:24 There’s a normal conduction pathway and there’s an accessory pathway. 03:27 Now, if you use an AV-nodal blocker to try to slow down a heart rate in a patient with WPW, it’s gonna work on the normal pathway, that runs through the AV node. 03:39 However, these patients have a second pathway, an accessory pathway, and your AV-nodal blocker is not gonna work on that accessory pathway. 03:47 So what’s gonna happen? You’ve got all kinds of electricity whizzing around the heart. 03:51 You block one pathway, so you’re gonna end up forcing the electricity down the other pathway which can actually accelerate conduction through the accessory pathway and cause the heart rate to further increase or you can precipitate ventricular fibrillation. 04:09 So, this is a potentially lethal error in these patients. 04:13 Now, very simply, if you treat the patient as though they have ventricular tachycardia and you don’t use AV-nodal blockers, you use the types of medicines that we’re gonna talk about for V-tach, you don’t have this problem because you’re gonna block both the normal and the accessory pathway simultaneously and you won’t set your patient up for this type of risk. 04:35 So, how do you diagnose ventricular tachycardia? Like we said, you have to have tachycardia so the rate has to be greater than 100. 04:45 It’s usually much higher than that though, it’s usually in the 150 to 200 range, about 180 is pretty average for V-tach. 04:53 You have to have a wide QRS complex which we already said is greater than 120 milliseconds, and you have to have a regular rate. 05:00 Now, there might be some minimal beat to beat variability, you certainly can see that but in general, you should see the QRS complex is coming along at a regular rate. 05:12 Anytime you have unstable v-tach, you need to cardiovert your patient. 05:18 So you're gonna perform synchronized cardioversion and get them out of v-tach. 05:22 If they're stable, you might choose to manage them medically. 05:26 And medical management of v-tach is gonna be the antiarrhythmic drugs. 05:30 The most commonly used one is probably amiodarone, at least in the US. 05:34 Although procainamide is a very safe and effective drug, and sotalol can also be used. 05:39 Now, the reason that we use these antiarrhythmics, is that they are non-selective, so they don't just act on the AV-node, like your beta-blockers and your calcium channel blockers do, they act on the entire myocardium, and decrease automaticity sort of decrease the willingness of the heart to generate an action potential. 05:59 So they're gonna work on rhythms that are originating outside of the normal conduction system. 06:06 Basically, they're gonna work on ventricular rhythms. 06:09 Now, if you have a patient who has regular monomorphic ventricular tachycardia, you might think, "Hey, maybe this is actually a supraventricular rhythm." And you can consider adenosine. 06:24 It's the one AV-nodal blocking agent that’s reasonable to attempt in wide complex rhythms because it is so short acting, it's unlikely to cause any major problems, like a beta-blocker or a calcium channel blocker would. 06:38 But really the mainstay of treatment for v-tach is gonna be cardioversion for unstable patients, and antiarrhythmic medication specifically amiodarone or procainamide for patients who are stable.
About the Lecture
The lecture Ventricular (VT) & Supraventricular (SVT) Tachycardia by Julianna Jung, MD, FACEP is from the course Cardiovascular Emergencies and Shock.
Included Quiz Questions
Which of the following statements regarding ventricular tachycardia is INCORRECT?
- It is easy to differentiate SVT with aberrancy and ventricular tachycardia.
- All wide-complex tachycardia should be assumed to be ventricular tachycardia until proven otherwise.
- Positive family history for ventricular rhythm disturbance makes ventricular tachycardia more likely.
- AV dissociation can be seen in the ECG of ventricular tachycardia.
Which of the following findings makes ventricular tachycardia less likely?
- QRS duration of 100 ms
- Rate of 180 bpm
- Minimal beat-to-beat variability
- QRS width of 3 mm
- Regular rate
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |