Playlist
Show Playlist
Hide Playlist
Urology Surgery: Testicular Pain
-
Slides TesticularPain Surgery.pdf
-
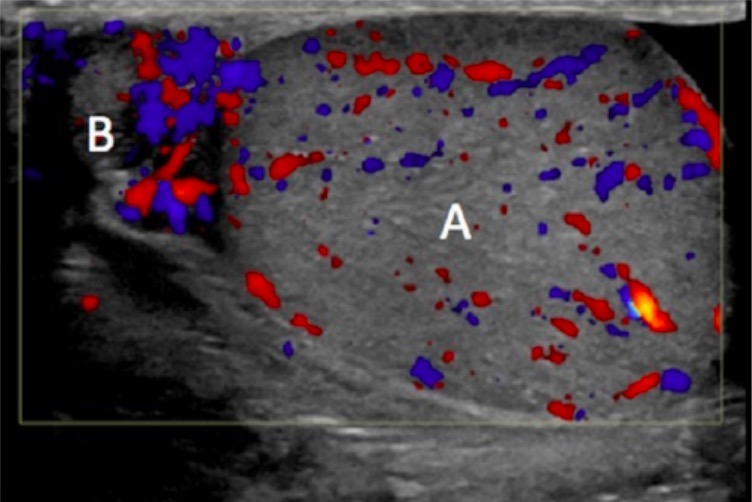
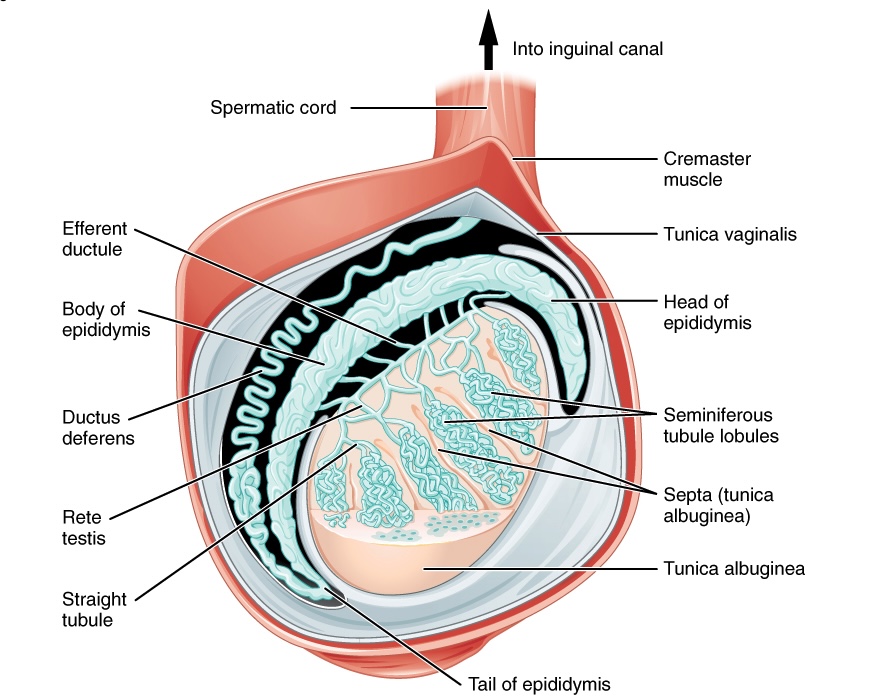
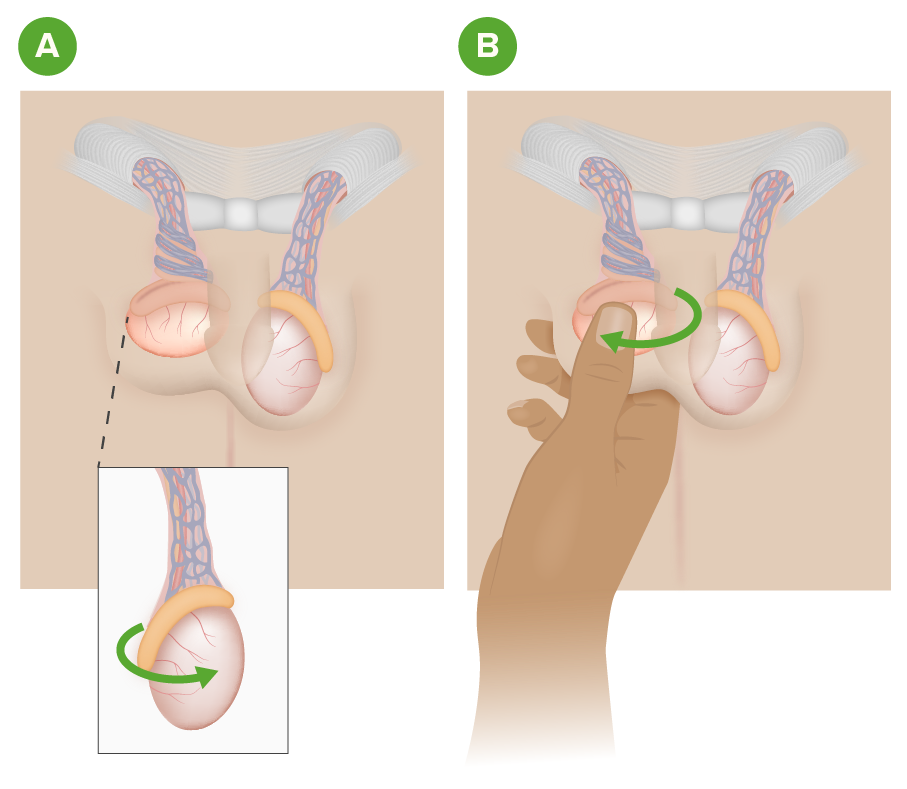
Download Lecture Overview
00:01 Thank you for joining me on this discussion of testicular pain in the section of urology. 00:09 Let's go over the anatomy of a testicle briefly. 00:13 On the center of the screen is a typical schematic of a testicle. 00:17 Note, highlighted in a green box is a tunica vaginalis. 00:21 It’s particularly important when we discuss torsion of the testicle. 00:26 Squiggly line about the left upper quadrant of that picture is the vas deferens. 00:30 And, of course, dead center is the testicle itself. 00:34 Now, let's move on to a discussion of testicular torsion. 00:38 Testicular torsion involves torsion of the spermatic cord structures. 00:43 As the picture demonstrates, normal on the left, twisted or torsed testicle on the right. 00:50 As the torsion happens, the spermatic cord, which produces the blood supply to the testicle, is all also compromised. 00:58 As a result, there's a risk of ischemia to the testicle. 01:02 This can cause a lot of pain. 01:04 The pathophysiology behind testicular torsion is important. 01:08 We recognize that the tunica vaginalis is not securely attached to the posterior lateral aspect of the testicle. 01:14 Recall another disease process where the attach – anatomic attachments are important? That's right. Colonic volvulus. 01:22 If the attachment of the tunica vaginalis is too high or insufficient, the spermatic cord is to freely floating and, as a result, can twist. 01:32 What are some physical findings? As you can imagine, there can be severe unilateral testicular pain associated with scrotal swelling and a reflexive nausea or vomiting. 01:42 Additionally, during testicular torsion, patient may lose their cremasteric reflex. 01:48 As a reminder, the cremasteric muscles are extensions of the internal oblique muscle fibers. 01:54 The cremasteric reflex is normally elicited by touching the inner thigh and watching if the testicle rises. 02:01 With testicular torsion, this reflex is lost. 02:04 Additionally, as a major differentiating point between testicular torsion and epididymitis, there's usually no relief of pain with the elevation of the testicle in torsion. 02:16 Routine laboratory values are of little consequence and are not indicative of testicular torsion. 02:22 Frankly, not necessary. 02:26 But ultrasounds are useful, specifically duplexes. 02:31 Ultrasound duplex assesses your flow of the spermatic vessels. 02:35 And, of course, the lack of spermatic vessel flow is indicative of torsion and indicative of high risk for ischemia. 02:42 Remember, only obtain an ultrasound if low suspicion of torsion. 02:46 Otherwise, you should rush to the operating room for surgical exploration. 02:50 Every minute counts! Now, let’s discuss the surgery. 02:54 Remember, very importantly, a delay in the de-torsion may lead to testicular ischemia. 03:00 Therefore, don't proceed to a duplex unless you have some question or a suspicion that it's actually not a torsion. 03:06 Scrotal fixation is necessary after the de-torsion. 03:10 As you can remember, the tunica vaginalis is inappropriately seated. 03:14 And if the testicle is not viable, you may actually have to remove it. 03:19 Now, let's move on to epididymitis. 03:22 Epididymitis is also a common cause for testicular pain. 03:26 Remember that the epididymitis, as the name implies, is an inflammation of the epididymis. 03:32 Retrograde passage of urine can occur from the prostatic urethra to the epididymis via the ejaculatory ducts and vas deferens. 03:42 As a result, epididymitis can occur. 03:45 There is some association with chlamydia and urine organisms and you should just be aware of this association. 03:53 Physical findings are very similar to testicular torsion. 03:57 Unilateral testicular pain, scrotal swelling and a reflexive nausea/vomiting. 04:02 Therefore, it's important to have differentiating factors between torsion and epididymitis. 04:08 As you can imagine, when the testicular – when the testicle is involved, it’s pretty difficult to examine the patient. 04:15 With epididymitis, there can also be a loss of cremasteric reflex. 04:20 However, there's generally some modicum of relief of pain on elevation. 04:24 This is called the Prehn’s Sign. 04:26 Again, laboratories may not be helpful, although as a sign of increased inflammation, there may be elevated white blood cell count. 04:33 But don't count on that. 04:35 How do we treat epididymitis? Unlike torsion, which is a surgical emergency, epididymitis can be treated medically. 04:42 Especially if an STD or sexual transmitted disease is related, particularly in chlamydia or gonorrhea, you should offer the patient ceftriaxone and doxycycline. 04:51 Otherwise, it's largely supportive care with non-steroidals, analgesics and sometimes ice packs can help. 04:58 Now, it's time to remind you of some important clinical pearls and high-yield information. 05:03 Remember, elevation of the testicle relieves pain in epididymitis, whereas does not in torsion. 05:09 Although this is classic teaching, frankly, it’s impractical in clinical care. 05:13 When a patient has testicular pain, it generally hurts no matter what you do. 05:17 And remember, testicular torsion is a urologic emergency. 05:22 Don't wait for additional diagnostic studies unless you suspect, in fact, that it's not testicular torsion. 05:30 Thank you very much for joining me on this discussion of testicular pain.
About the Lecture
The lecture Urology Surgery: Testicular Pain by Kevin Pei, MD is from the course Special Surgery. It contains the following chapters:
- Urology Surgery – Testicular Pain
- Epididymitis
Included Quiz Questions
Testicular torsion can occur in which of the following conditions?
- Tunica vaginalis is not securely attached to the posterolateral aspect of testicle
- Tunica albuginea not securely attached to the anterolateral aspect of the testicle
- Tunica vaginalis is not securely attached to the lateral aspect of the testicle
- Tunica albuginea not securely attached to the posterolateral aspect of the testicle
- The spermatic cord is not securely attached to the anteroposterior aspect of testicle
A patient presents to you with testicular pain. He is diagnosed with epididymitis and STD testing was negative. Which of the following is the best treatment option?
- NSAIDs
- Ceftriaxone
- Cefepime
- Doxycycline
- Levofloxacin
Customer reviews
3,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
1 |
| 2 Stars |
|
2 |
| 1 Star |
|
0 |
Though brief, it covered the main points, the dx and treatment. The differentiation was lacking.
Few details, not sufficient explanation. Please make the breaks between the slides longer
It isnt clear the difference between torsion and epidymitis and i would like more images
1 customer review without text
1 user review without text