Playlist
Show Playlist
Hide Playlist
Type 2 Diabetes Mellitus – Hyperglycemia
-
Slides HyperglycemiaDiabetesMellitus EndocrinePathology.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
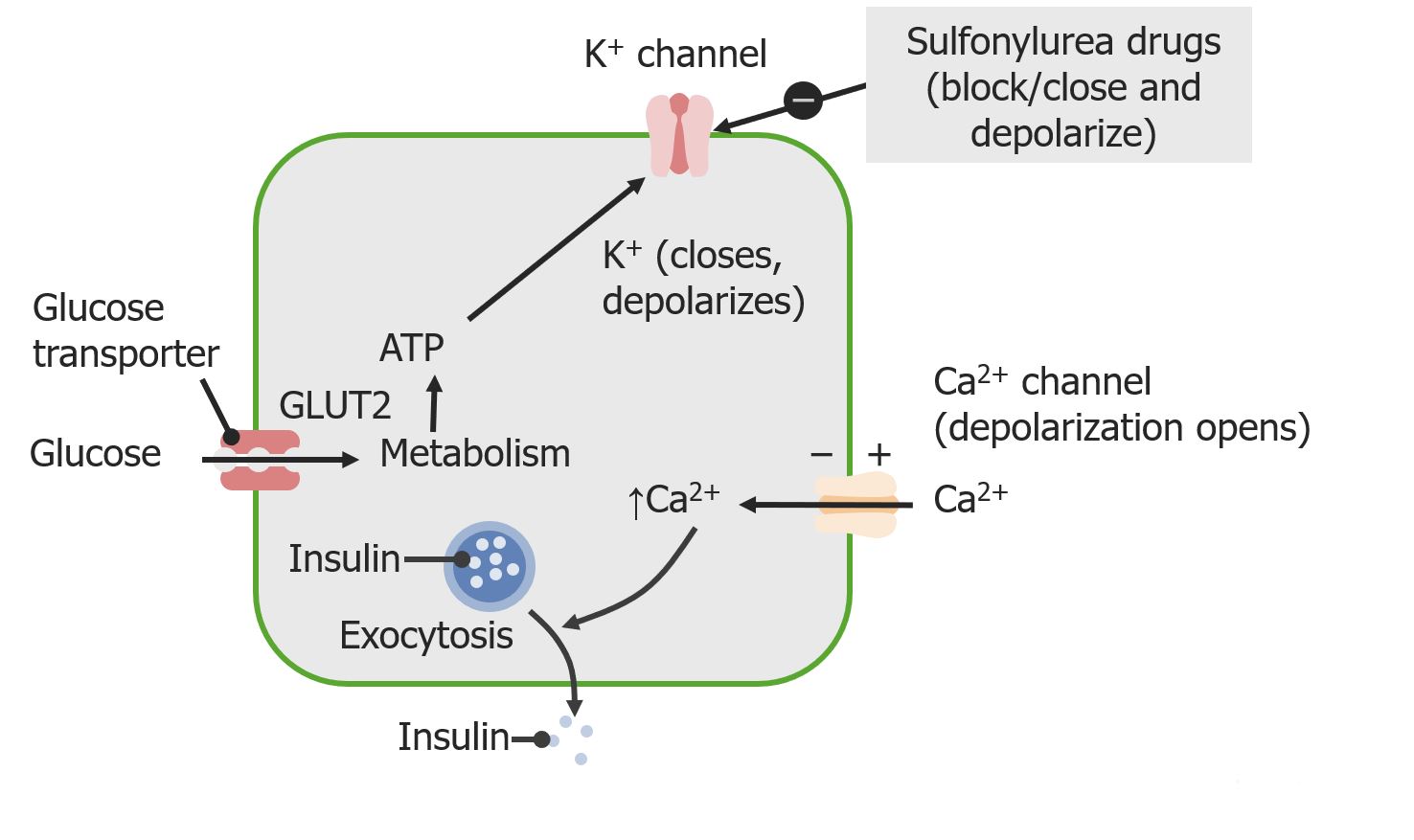
00:01 Let’s talk about type II. 00:03 The type II diabetes, the basic characteristics, epidemiology: usually later in life, greater than 30. 00:09 These patients will be obese as far as you’re concerned and a major, major genetic family history component. 00:17 Here, the patho-physio that you want to know for sure, priority would be the fact that the insulin receptors are resistant. 00:23 Do you remember those insulin receptors with two beta sub-units, with autophosphorylation in tyrosine kinase? Somewhere in that apparatus of the membrane, the insulin receptor isn’t working. 00:37 Where’s my glucose? Decreased peripheral glucose uptake resulting in hyperglycemia. 00:45 The beta cell dysfunction is quite interesting, we’ll walk you through this. 00:49 So, initially, the patient becomes obese. 00:53 Okay, gradually; you don’t become obese overnight. 00:57 As it goes on to become obese, the insulin receptors are working less and less and less which means that now the patient is increasing their glucose step by step by step overtime. 01:13 In type II diabetes, it’s still possible that you have insulin in your pancreas, correct? Yes, therefore, with that hyperglycemia early on, do you think that your patient with type II diabetes might have hyperinsulinemia? Yeah, lot of research mind you with this because that hyperinsulinemia can actually wreak havoc up and down the body. 01:42 For example, take a look at the armpits of a patient with type II diabetes or the back of the neck of type II diabetes and you’ll notice there’s darkening of the skin. 01:55 Nigra means dark; acanthosis means thickening… thickening of the keratinocytes, therefore giving you the presentation of dark skin underneath the armpits and maybe the back of the neck. 02:09 Maybe the insulin in fact, there’s a lot of evidence out there that that increased insulin early on in type II diabetes may then cause this. 02:20 Perhaps even the atherosclerosis, maybe even hypertension. 02:24 Insulin level increased… now, you understand this. 02:28 If you do not follow my discussion just now, this becomes rather difficult. 02:34 Early on, you can have increased levels of insulin, but at some point in time what happens? Well, with the pancreas, you might exhaust all levels of insulin. 02:43 What’s your first step of management? Discipline, lifestyle modification, exercise, watch your diet. 02:51 If that doesn’t work, patient’s non-compliant, then you start thinking about oral hypoglycemic drugs. 02:58 Worst case scenario… insulin. 03:02 Complications… ketoacidosis is rare, but can occur after stress such as surgery… type II diabetes. The more common hyperglycemic emergency in type II diabetes is a hyperosmolar hyperglycemic state, which can develop more insidiously. 03:21 Pathology, couple of important things here. 03:25 Fibrosis and hyalinization… fibrosis and hyalinization. 03:31 Fibrosis might be found in the pancreas, you can have an amyloid and we’ll talk about it in a little bit called amylin and if you’re thinking about type II diabetes and you’re referring to what’s known as arteriolosclerosis… arteriolosclerosis, there are two kinds remember? You’re putting things together? Hyaline, arteriolosclerosis; hyperplastic, arteriolosclerosis. 04:00 Which one is it that you find in type II diabetes and hypertension? Hyaline, arteriolosclerosis. 04:11 Non-conventional type II diabetes… similar to type II, occurs in the young. 04:16 Increasing in frequency, meaning to say as we gain better understanding of diabetes mellitus, we actually find this as being increasing type of diagnosis, genetically inherited, this is important. 04:30 It’s one thing that you want to take out of the symptoms referred to as being MODY. 04:33 MODY, stands for Maturity Onset of Diabetes in the Young, M-O-D-Y. 04:41 Usually genetic proponent, may usually develop type II diabetes. 04:45 However, this is a heterogeneous disorder, and depending on the underlying genetic cause, patients may present similar to type I. 04:54 So, therefore, do not confuse this with type I diabetes. 05:01 Type I diabetes, young patient, autoimmune destruction of the pancreatic islet cells. 05:06 Type I diabetic, insulin is not going to be present. 05:09 You’re worried about hyperglycemia. 05:10 The only method of treatment would be to give insulin. 05:14 Here, however, glucokinase could be a problem. 05:19 Remember glucokinase? One of the first enzymes in the glycolytic pathway… not the rate-limiting enzyme, but the first stanza. 05:26 So, if glucokinase is not present, then what happens? May result in hyperglycemia not conventional and may then go on to develop type II diabetes. 05:35 This is not present at all in type I. 05:38 Could be insulin molecule production or secretion issues, but the big one that you want to take out of this is the first bullet point of glucokinase… non-conventional.
About the Lecture
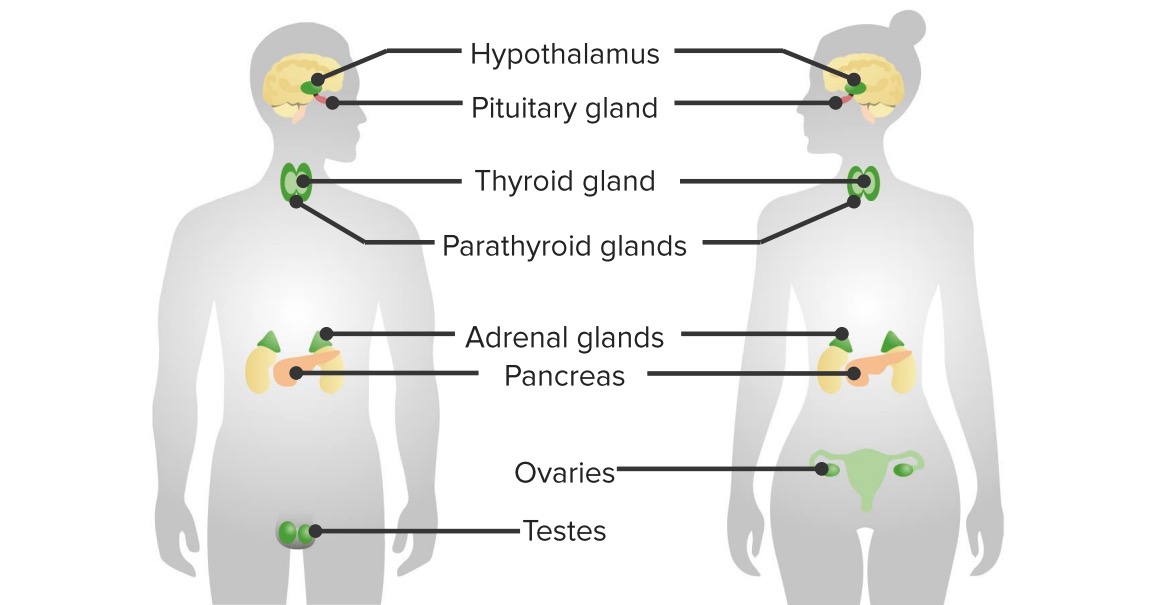
The lecture Type 2 Diabetes Mellitus – Hyperglycemia by Carlo Raj, MD is from the course Pancreatic Disease and Diabetes.
Included Quiz Questions
What is FALSE about type 2 diabetes mellitus?
- DKA is the most common initial presentation.
- The disease process most often occurs later in life.
- It has a stronger genetic predisposition than type 1 DM.
- The disease is associated with a higher BMI.
- The presence of prediabetes is a strong indicator of the development of disease.
What is the consequence of decreased peripheral glucose uptake and increased hepatic glucose production on pancreatic beta-cell function and insulin secretion?
- β cell dysfunction and impaired insulin secretion
- DKA
- Hypoglycemia
- Decreased response to exogenous insulin
- Increased release of glucagon
What material is deposited within the pancreatic islets in advanced type 2 diabetes mellitus?
- Amyloid
- Lymphocytes
- Phospholipase A
- Mutated glucagon
- Tau
What is NOT potentially affected by a genetic mutation in cases of maturity-onset diabetes of the young (MODY)?
- Glucagon secretion
- Glucokinase
- Insulin production
- Insulin secretion
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
love your lectures especially your calm way of standing,speaking,teaching and sometime smiling among one of best teachersof mine