Playlist
Show Playlist
Hide Playlist
Treatment Regimens for Mycobacterium Tuberculosis – Antimycobacterial Agents
-
Slides Treatment Regimens for Mycobacterium Tuberculosis Antimycobacterial Agents.pdf
-
Reference List Pharmacology.pdf
-
Download Lecture Overview
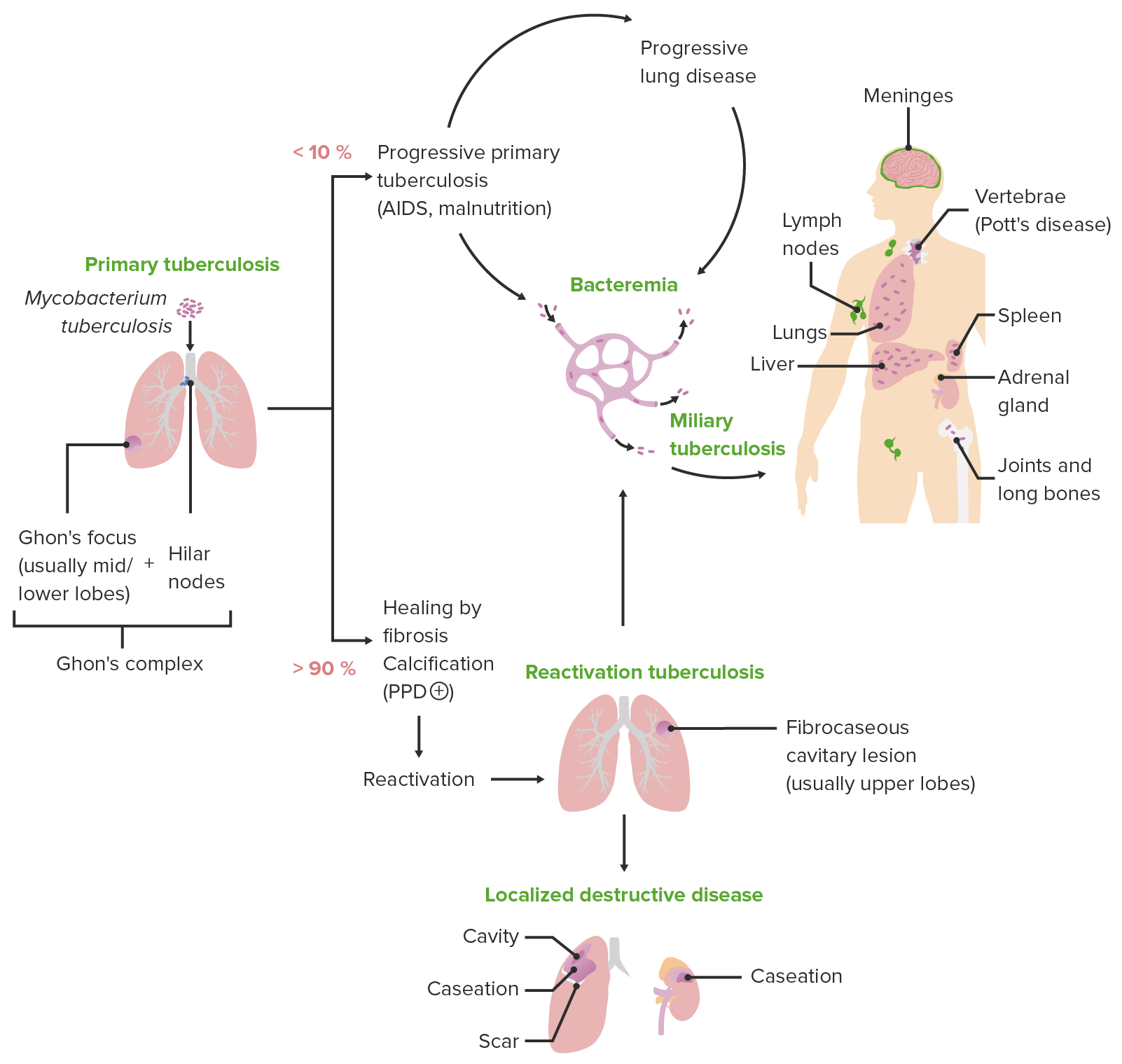
00:00 Before I discuss the treatment of symptomatic tuberculosis, I will outline the proper clinical terminology of asymptomatic and symptomatic TB and explain why it is important to distinguish between them. Tuberculosis infection, TI, is the newer term for what is still known also as latent tuberculosis infection, represents an asymptomatic and non-communicable state of TB. 00:23 Individuals with TI have been exposed to mycobacterium tuberculosis and have developed a specific cell-mediated immunologic response. 00:33 This response can be detected through a positive tuberculin skin test, TST, and/or an interferon gamma release assay, IGRA. Despite being asymptomatic, TI carries a risk of progressing to active TB disease. In otherwise healthy individuals, this lifetime risk is estimated to be between 5 to 10 percent. However, the risk may exceed 10 percent in those with compromised immune systems, such as individuals infected with HIV or those on immunosuppressive treatments. A higher risk is also seen in people living in high TB prevalence areas, young children, and the elderly. The risk of progression is highest within the first two years following the initial infection. Treatment for TI typically involves one or two drugs. Rifampin, 10 mRg per kg orally daily for four months, is the preferred choice. 01:32 This treatment regimen aims to reduce the risk of developing active TB in the future and is generally effective with a lower toxicity profile compared to the more extensive drug combinations used for treating active TB disease. 01:46 Tuberculosis disease, TD, is also known by older, but still used terms, such as active tuberculosis, active tuberculosis disease, or active tuberculosis infection, is characterized by an infection that is both symptomatic and communicable, unlike TI. Management of drug susceptible TD involves a two-phase treatment regimen. 02:08 The initial intensive phase includes four drugs, isoniazid, rifampin, pyrazinamide, and ethambutol, administered for eight weeks. This is followed by a continuation phase consisting of isoniazid and rifampin for at least another 18 weeks. 02:28 Let's take a look at the guidelines in the drugs used to treat mycobacterial infections in TB. 02:34 Make sure you look up TB treatment regimens in your own region of the world. 02:38 They will vary based on where you live. 02:41 Remember that pregnant and breastfeeding women need some vitamin B such as pyridoxine supplementation and that's because some of these drugs interfere with the vitamin B6 pathway. 02:55 These are the drugs that I'm going to address right now and these are the three letter designations that I'll use in this particular slide set. 03:02 Now let's look at our tuberculosis treatment regimens. 03:06 We have two main options, the standard six-month regimen, which remains our primary choice due to its proven safety and broad applicability, and the newer four-month regimen. 03:18 Let's start with our standard regimen. 03:20 For adults with TB who don't have HIV, we treat the first two months with isonia zid, rifampin, pyrazinamide, and ethambutol. 03:30 In the following four months, they'll get just isoniazid and rifampin. 03:35 Here's a helpful mnemonic: For TB treatment, remember the ripe fruits for the intensive phase and just the RI for the continuation phase. 03:45 For adults who have both TB and HIV, we add ART, that's antiretroviral therapy, to this regimen. 03:54 So they'll receive ART plus INH, that's isoniazid, rifampin, pyrazinamide, and ethambutol for the first two months. 04:03 Then for the next four months, they'll continue with ART plus isoniazid and rifampin. 04:10 Pregnant women with active TB have a special regimen. 04:13 They'll receive isoniazid, rifampin, and ethambutol. 04:18 Notice we don't give them PZA. 04:20 This treatment extends to nine months total. 04:23 Two months intensive phase and seven months continuation phase. 04:27 Now let's talk about our newer four month regimen. 04:30 These patients receive rifampin, isoniazid, pyrazinamide, and moxifloxacine for two months, followed by rifampin, isoniazid, and moxifloxacine for nine more weeks. 04:42 However, we need to be careful with patient selection here. 04:46 This shorter regimen isn't for everyone. 04:49 We can't use it in pregnant or breastfeeding patients, cases involving bones and joints, the central nervous system, the heart lining, or widespread TB. 04:58 For HIV positive patients, we need to see CD4 counts above 100 cells per cubic millimeter before considering this option. 05:08 Now, we have different guidelines in different parts of the world. 05:12 For my American students, here is the website from the Centers for Disease Control. 05:19 For my countrymen in Canada, this is the website through Health Canada. 05:25 My friends in the United Kingdom can look at the very excellent Nice guidelines, N-I-C-E. 05:31 For my friends in India, you can look at this website. 05:35 For my friends in other parts of Europe and for my friends in Africa, we have all of these different guidelines that are relatively specific for your region of the world. 05:44 Now, if you go to the CDC website, they will actually give you guidelines for different parts of the world as well but please look up your own region's guidelines so that you can have a really good idea of which ones to learn for your particular part of the world. 05:59 If you're studying for the USMLE, please look at the CDC guidelines. 06:04 These guidelines can change every single year and one year, I remember, it actually changed in six months. 06:11 So, keep up to date with the guidelines. 06:13 There's no way that I can keep up with the lectures and the guidelines, so, look them up yourself before you go and write your exam. 06:20 Thank you very much. It was great having you listen to me. Go write your exam. 06:25 I know you're gonna do well. Good luck.
About the Lecture
The lecture Treatment Regimens for Mycobacterium Tuberculosis – Antimycobacterial Agents by Pravin Shukle, MD is from the course Antimicrobial Pharmacology. It contains the following chapters:
- Drugs Regimens - Mycobacterium Tuberculosis
- Drugs Regimens - Mycrobacterium Leprae
- Drugs Regimens - Atypical Mycrobacterium Infections
Included Quiz Questions
In the standard regimen for tuberculosis disease treatment, which drugs are stopped after 2 months in non-HIV patients?
- Pyrazinamide and ethambutol
- Rifampin and isoniazid
- Dapsone and isoniazid
- Ethambutol and azithromycin
What is the estimated lifetime risk of progression from tuberculosis infection (TI) to tuberculosis disease (TD) in otherwise healthy individuals?
- 5-10%
- 1-2%
- 10-20%
- 20--30%
- 30--40%
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |