Playlist
Show Playlist
Hide Playlist
Sulfonamides, Trimethoprim and Fluoroquinolones – Antimetabolites
-
Slides Sulfonamides Trimethoprim Fluoroquinolones.pdf
-
Reference List Pharmacology.pdf
-
Download Lecture Overview
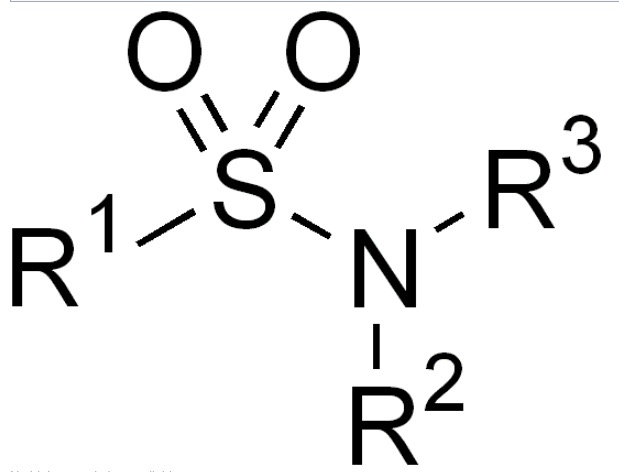
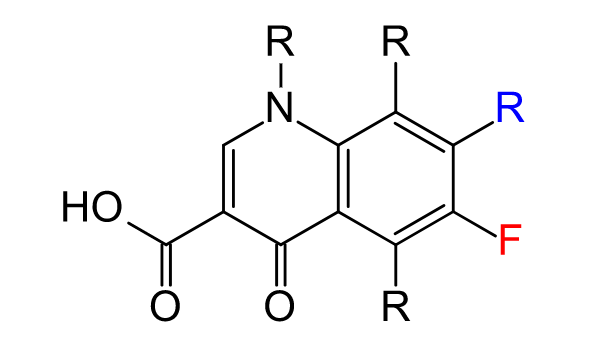
00:01 Let's talk about the sulfonamides. 00:04 Now sulfonamides, are weak acids and their congeners or structurally similar to a chemical called Para-aminobenzoic acid (PABA). 00:14 Which, is actually shown in illustration right here. 00:17 Now, these are bacteriostatic inhibitors of folic acid synthesis. 00:22 So, mammals obtain their folic acid from the diet, whereas bacteria have to manufacture it. 00:30 Now, most of this particular drug is going to be excreted in the urine. 00:34 So, trimethoprim is often added to the sulfonamides, these are selective inhibitors of dihydrofolate acid reductase. 00:42 It inhibits the bacterial form, it prevents formation of tetrahydrofolate. 00:48 Now, bacterial dihydrofolate reductase is five times more sensitive to trimethoprim than the human version of the same enzyme. 00:56 So, from a trimethoprim point of view, it's really a non-issue. 01:02 We combine sulfamethoxazole with trimethoprim, to create an agent called Septra which is sold commercially are also called SMP/TMP. 01:12 Now, bacterial synergy is obtained because we're acting on two different levels of the folic acid production pathway. 01:21 Now, the sulfonamides work on this particular enzyme at the top of this structure and trimethoprim works on dihydrofolic acid reductase at the middle of this structural pathway. 01:34 These drugs are concentrated in the bladder, so, they're particularly effective in bladder infections. 01:40 Now, we also use this agent in, pneumocystis jirovecii infections and toxoplasmosis infections in HIV-positive patients. 01:47 So, it's not just used in urinary tract infections alone. 01:52 Now, Septra toxicity includes hypersensitivity reactions, which, are actually surprisingly common a lot of patients are allergic to sulfa and they will have a cross allergy to this agent. 02:05 There are also cross allergies with other agents as well. 02:08 So, an example for this is if patients are allergic to Septr for example, they may also be allergic to ACE inhibitors and even rarer but but seen is ARB’s. 02:19 Now, another side effect with this medication is, nausea vomiting and diarrhea and very rarely you may get episodes of granuloycytopenia, thrombocytopenia. 02:30 Hemolysis is often seen too, in patients who have G6PD deficiency, so that's an important consideration in some patients. 02:41 Let's move on to fluoroquinolones. 02:43 Now, we have several generations of fluoroquinolones out there. 02:47 Let's talk at the them one at a time. 02:49 The first generation was norfloxacin. 02:52 It's not really clinically used anymore because of toxicity issues and lack of efficacy issues. 02:57 So, this was replaced with the second-generation fluoroquinolones. 03:01 Ciprofloxacin being the prototypical one and probably the best known of the fluoroquinolones. 03:08 It has more gram-negative activity, especially against gonococcus. 03:14 The third-generation agents include levofloxacin and these are less active against gram-negative bacteria, but they, have a much greater activity against gram-positive cocci and MRSA and anaerobes. 03:31 And they’re actually quite effective against atypical bacteria like, M. pneumoniae and C. pneumoniae. 03:37 So, levofloxacin which is called Levaquin commercially is often used in pneumonia. 03:47 Now, the fluoroquinolones in general have very good oral bioavailability and they are eliminated through the kidney, so, we have to be aware of renal function. 03:57 The other issue that we have to be aware of is that this drug, is actually blocked by probenecid the excretion of it. 04:03 So, in patients who are also on probenecid you may have toxic levels. 04:07 An agent called moxifloxacin has hepatic clearance and may be used in renal failure. 04:13 These agents have half-lives of three to nine hours, so, they're most often given twice a day. 04:19 Some formulations though are actually given once a day and a good example is, a formulation called “Cipro XL,” which is, ciprofloxacin, a special kind of pill, that allows it to be given once a day and that's used most commonly in epididymitis for example. 04:37 So, how do these agents work? The mechanism of action of fluoroquinolones is actually quite interesting. 04:44 They interfere with DNA topoisomerase II. 04:49 So DNA topoisomerase is the enzyme that's responsible for taking that helical twisted three-dimensional structure and untwisting it, so that, we can get access to the genetic information inside it. 05:01 So, by interfering with it, you actually interfere with the first step of DNA transcription. 05:10 Topoisomerase II is inhibited in the gram-negative organisms and type IV is inhibited in the gram-positive organisms. 05:20 Now, I want to make sure that you know this because this is a great exam question. 05:24 One of those useless pieces of information that we love to put on exams for you. 05:29 So, make sure you remember this and then once you pass your exams you can forget it. 05:33 Now, these agents are bactericidal. 05:37 These agents also have a post antibiotic effect, which is quite nice when you give them short term, you know that there's going to be a long-term beneficial effect with these agents. 05:48 In terms of how bacteria develop a resistance to fluoroquinolones, it's kind of an interesting phenomenon. 05:54 What they do is they change their porins, so that, they actually reduce the intracellular concentration or accumulation of this drug. 06:04 The efflux mechanisms in M. tuberculosis, S. aureus and S. pneumoniae are also in play here. 06:13 The other thing that will happen too, is that we'll see changes in the sensitivity of the target enzymes. 06:19 So, sometimes that DNA topoisomerase, will have, a point mutation that prevents the fluoroquinolone from doing its job. 06:27 Now, these are interesting in the sense that they are actually, drug and bug specific. 06:32 So, gyrA is actually a gene that codes for the resistance to certain fluoroquinolones in the gonococcus bacteria. 06:44 In terms of toxicity, gastrointestinal distress, skin rash, headache and insomnia are quite commonly seen. 06:52 More rarely you will see phototoxicity, now tendinitis and tendon rupture has been reported, in terms of fluoroquinolone toxicity. 07:01 It's important to note that we do not recommend these agents in pregnant women or in children who are growing and the reason is, because it may damage their cartilage and they may develop arthropathy, especially in patients who are in their teenage years, I find that a lot of physicians forget this and they prescribe it to their teen kids, who haven't finished growing. 07:22 So, do not do that, only in fully grown mature adults. 07:27 Now, the newer agents in this drug class may also prolong the QT interval, so we have to be aware of that potential problem as well.
About the Lecture
The lecture Sulfonamides, Trimethoprim and Fluoroquinolones – Antimetabolites by Pravin Shukle, MD is from the course Antimicrobial Pharmacology. It contains the following chapters:
- Sulfonamides
- Trimethoprim
- Sulfamethoxazole/Trimethoprim
- Flouroquinolones
Included Quiz Questions
Sulfamethoxazole/trimethoprim is useful against bladder infections. What pharmacological property of the drug allows it to be effective in this situation?
- It concentrates in the bladder.
- It requires a low pH environment to become activated.
- It concentrates in the urethra where infectious organisms typically dwell.
- It is a weak acid that must be deprotonated to exert its effect.
- Cells of the bladder do not require folate, so there is less organ damage compared to other drugs.
What is one toxicity of fluoroquinolones?
- Tendon rupture
- Shortened QT interval
- Ototoxicity
- CML
- Acromegaly
Which fluoroquinolone undergoes hepatic clearance?
- Moxifloxacin
- Ciprofloxacin
- Levofloxacin
- Norfloxacin
- Oflaxacin
What statement about fluoroquinolones is INCORRECT?
- These agents are bacteriostatic.
- They have good oral bioavailability.
- They work by interfering with DNA topoisomerase II in gram negative organisms.
- They are usually administered twice daily.
- Kidney excretion of fluroquinolones is blocked by probenecid which may lead to toxic accumulation.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |