Playlist
Show Playlist
Hide Playlist
Sexually Transmitted Infections: Drips/Discharges, Pelvic Inflammatory Disease, and Trichomonas Vaginalis
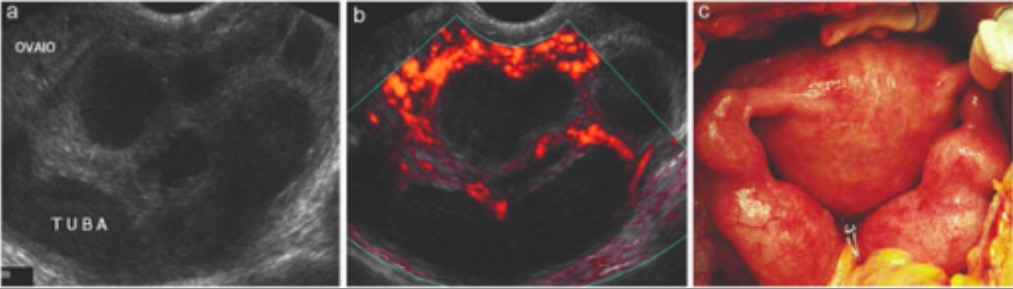
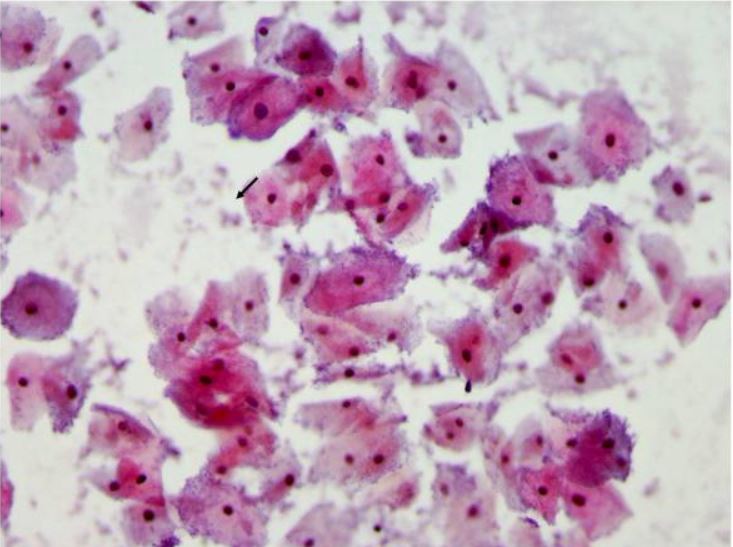
00:01 Let's now review another case. 00:03 A 35 year old woman who is HIV-positive presents with a one week history of yellow vaginal discharge and mild dysuria. 00:11 What about her HIV status concerns you? I'll let you think about that. 00:25 Well, what's in your differential diagnosis? What would you do next? If you're taught to ask the patient, "is she using condoms during sex?" That's a good question. 00:38 You want to ask every patient, "Do you use barrier contraception to avoid STIs?" But especially in HIV-positive patient as she can transmit the virus to her partner. 00:49 Offer the patient testing for her partner in case she does have a partner. 00:55 Could she possibly have an STI? Well, she does have an abnormal discharge. 01:01 You also wanna ask the patient, is she taking her HIV meds? this is important as it keeps the virus titers low. 01:09 Typically, patients are treated with anti-retrovirals. 01:13 What else should she be screened for? Let's go on as you think about that. 01:20 Well, let's now talk about the second criteria for the CDC's diagnosis of clinical drips. 01:27 So, gonorrhea is a very common cause of a discharge in a woman. 01:33 You can also have nongonococcal urethritis, chlamydia, mucopurulent cervicitis and trichomonas vaginalis that causes vaginitis and urethritis and of course, bacterial vaginosis. 01:48 Remember that bacterial vaginosis is not an STI but it is sexually associated and let's not discuss that now. 01:56 The vagina typically has an acidic ph but with intercourse, the sperm increases the ph of the vagina and actually causes an overgrowth of certain bacteria. 02:07 This leads to a fishy, vaginal discharge that these patients can suffer from recurrently. 02:16 Let's now talk about gonorrhea. 02:18 Gonorrhea is a urogenital infection in the female and can cause infection specifically in the endocervical canal. 02:26 70 to 90% also colonize the urethra. 02:30 The incubation period is unclear but usually signs and symptoms occur within ten days of an infection. 02:37 Most patients complain of a vaginal discharge, painful urination or dysuria and labial pain, swelling or abdominal pain. 02:45 There are other forms of urethritis besides those caused by gonorrhea. 02:50 They can be nongonococcal urethritis. 02:53 20 to 40% actually is caused by chlamydia. 02:57 Another 20 to 30% is caused by mycoplasma, another half is actually unknown. 03:05 And occassionally, trichomonas vaginalis and HSV can cause urethritis. 03:11 You can have mild dysuria or pain upon urination and sometimes a vaginal discharge that is mucoid. 03:19 You can see polymorphonuclear cells on a urethral smear. 03:24 but that's typically very painful and hard to tolerate. 03:28 You can see on microscopy in the urine that there would be the presence of white blood cells and you may see the presence of leukocyte esterase. 03:38 Let's now talk about chlamydia. 03:40 Chlamydia can mostly be asymptomatic. 03:43 It's actually asymptomatic but causes a lot of morbidity especially to the female GYN tract. 03:50 Clinical manifestations of chlamydia include cervicitis, urethritis and PID. 03:56 PID can be very devastating to a woman's fertility. 04:00 Complications include potential transmission to a newborn during delivery. 04:05 This can cause conjunctivitis and pneumonia in a newborn and the pediatricians need to be alerted to the status of mom if she has chlamydia. 04:16 Let's now look at what a normal cervix looks like. 04:19 Here you can see the cervix is pink and looks to have no discharge or lesion. 04:24 However, this cervix appears intensely red and angry and has a discharge. 04:31 So typically, when you wanna test for chlamydia, you would insert a Q-tip that allows us to obtain some of the mucus and send that off for PCR or nucleic acid testing. 04:46 You can also do a gram stain to look for gonorrhea. 04:52 You can do a non-culture, non-amplified test or you can do a nucleic acid amplification test and you can use urine, cervical swabs as I just described, urethral swabs, vaginal swabs and also a PAP smear. 05:09 But we typically don't use a PAP smear to screen for STIs. 05:14 And don't forget, you can do serology especially when you have LGV present. 05:19 Today, I'll discuss current treatment guidelines for gonorrhea, which reflect our response to increasing antibiotic resistance worldwide. 05:26 Let's start with treatment. 05:28 The standard is now high dose ceftriaxone, given intramuscularly as a single dose. 05:33 The dose is weight based 500mg for patients under 150kg, and one gram for those 150kg or heavier. 05:43 This higher dosing strategy helps combat emerging resistance patterns. 05:47 When we diagnose gonorrhea, concurrent STI testing is crucial. 05:52 Always test for HIV, syphilis, and chlamydia. 05:56 Consider hepatitis testing, too. 05:58 If your patient tests HIV negative, this presents an important opportunity to discuss HIV pre-exposure prophylaxis. 06:06 As gonorrhea indicates high risk sexual behavior. 06:09 Chlamydia frequently coexists with gonorrhea, so we give presumptive treatment unless testing has specifically ruled it out. 06:16 For non-pregnant patients. 06:17 Doxycycline is preferred 100mg orally, twice daily for seven days in pregnancy. 06:24 We switch to azithromycin one gram as a single oral dose, since doxycycline is contraindicated. 06:31 Partner management is critical. 06:32 We need to treat all sexual partners from the past 60 days. 06:36 This can be challenging. 06:38 So we have EPT expedited Partner therapy, where we can provide prescriptions or medications for partners without requiring them to come in for evaluation. 06:47 For this, we use cefixime 800mg orally once plus chlamydia treatment if needed. 06:53 However, EPT isn't recommended for men who have sex with men due to their higher risk of coexisting infections, particularly HIV, which require direct evaluation. 07:04 Remember, effective partner treatment prevents re-infection and helps control the spread of resistant strains. 07:10 Let's continue our discussion with follow up testing and alternative treatment regimens for gonorrhea. 07:16 Follow up testing happens in two distinct time frames. 07:19 First, we have the test of cure at 7 to 14 days after treatment. 07:24 This isn't needed for everyone. 07:25 It's specifically required for pharyngeal infections because they're harder to treat. 07:30 For anyone who received an alternative treatment regimen. 07:33 And for pregnant women who couldn't receive standard therapy. 07:36 However, and this is crucial. 07:38 All patients need retesting at three months. Why? Because the re-infection rate is surprisingly high. 07:45 About 20%. 07:46 This happens for several reasons. 07:48 Untreated partners, new infected partners, or asymptomatic reinfections. 07:54 This high reinfection rate also signals ongoing high risk sexual behavior that needs to be addressed. 08:00 Now what if your patient can't receive our standard ceftriaxone treatment? For those with severe beta lactam allergies? We have alternative regimens. 08:09 The main option is combining gentamicin 240mg intramuscularly with a high dose of azithromycin two grams orally, both given once. 08:20 Other cephalosporins are also options. 08:23 Though their routs of administration vary. 08:25 Remember, these alternative regimens are only for patients who truly can't receive Ceftriaxone. 08:32 They're not our first choice because we want to preserve our most effective treatments and prevent antibiotic resistance. 08:38 Let's discuss the current treatment guidelines for chlamydia. 08:42 For non-pregnant patients, our first line treatment is doxycycline 100mg, taken by mouth twice daily for seven days. 08:50 We prefer this medication because it shows better cure rates than other options, particularly for rectal infections. 08:57 We do have alternatives. 08:58 Azithromycin, given as a single one gram oral dose, is our backup option. 09:03 We use this when we're worried about patient compliance with the seven day doxycycline course. 09:08 And it's our go to medication for pregnant patients. 09:12 There's also levofloxacin 500mg daily for a week. 09:16 But we rarely use it due to cost and side effect concerns. 09:20 When we diagnose chlamydia, we must do additional testing. 09:23 Every patient needs HIV, syphilis, and gonorrhea tests. 09:27 We should consider hepatitis screening. 09:30 And for women of childbearing age, pregnancy testing is essential. 09:34 If the HIV test is negative, this presents an opportunity to discuss HIV pre-exposure prophylaxis. 09:40 Some critical patient education points no sexual activity during treatment. 09:45 All sexual partners from the past 60 days need treatment. 09:49 This is crucial for preventing reinfection. 09:52 Remember that many infections are asymptomatic but can still cause complications if untreated. 09:58 While we don't routinely need a test of cure, we do want to retest all patients in three months because a reinfection is common. 10:05 This comprehensive approach helps ensure effective treatment and prevents both complications and transmission. 10:11 Let's now review PID. 10:14 10 to 20% of women who have gonorrhea and chlamydia actually develop PID. 10:20 In north America, there is a high proportion of chlamydia than gonorrhea in patients who have PID symptoms. 10:29 Let's now review the CDC minimal criteria. 10:31 You may have uterine tenderness, adnexal tenderness or you may have cervical motion tenderness. 10:38 Remember that the adnexa is a zip code, not an address. 10:42 There are many things that live in the adnexa including the ovaries and the fallopian tubes. 10:47 However, we also have bowel and also sometimes the ureter. 10:55 Other symptoms include: endocervical discharge, fever, lower abdominal pain. 11:01 And the complications result in infertility. 11:04 With one episode of PID, you could have a rate of 15- 24% of infertility secondary to gonorrhea or chlamydia. 11:12 You have an increased risk of ectopic pregnancy with just one episode of PID. 11:17 And of course, chronic pelvic pain is increased in the population who has suffered from PID. 11:23 Prevention is best. 11:27 Let's now talk about some of the pathologic findings that you see upon laparoscopy. 11:32 This may not be too clear here but this is a laparoscopic picture what we would look up at the liver and see that there are adhesions forming from the anterior abdominal wall to the liver. 11:45 This is called Fitz-Hugh Curtis syndrome. 11:48 It look like violin strings and if you see this, this is pretty much confirms that the patient has had PID. 11:57 Also, if a patient becomes pregnant after PID, remember that her ectopic pregnancy risk is increased seven times after a single incidence of PID. 12:09 And ectopic pregnancy is a medical emergency and can be potentially fatal if not promptly diagnosed and managed. 12:17 Let's now talk about the treatment of PID. 12:20 Think of pelvic inflammatory disease or PID as a detective case. 12:25 What are we looking for? Three key physical findings in sexually active women cervical motion tenderness, uterine tenderness or adnexal tenderness. 12:35 Just one of these findings with pelvic pain is enough to act. 12:39 The causative organisms tell us what we're fighting, mainly Neisseria gonorrhea and chlamydia. 12:44 trachomatis, plus other vaginal bacteria that have moved upward. 12:48 This is why we need broad antibiotic coverage. 12:51 When do you hospitalize? Remember these four scenarios? Really sick patients, high fever, severe vomiting, pregnant women. 12:59 Suspected pelvic abscess. 13:01 Possible surgical abdomen. 13:03 The key. Take home point. 13:04 Don't wait for severe symptoms to treat early treatment. 13:08 Prevent serious complications like infertility. 13:11 Let's talk about treating PID. 13:13 We have two pathways outpatient and inpatient. 13:16 And your job is to choose wisely. 13:18 For outpatients, think triple therapy. 13:21 One shot of ceftriaxone intramuscularly plus two oral medications doxycycline and metronidazole for two weeks. 13:30 The dosing is straightforward. 13:31 Doxycycline 100mg twice daily. 13:34 Metronidazole 500mg twice daily for sick patients needing hospitalization we’re more aggressive IV ceftriaxone or cefoxitin plus the same oral medications once they're improving. 13:48 Usually within 24 to 48 hours, we can switch to all oral medications. 13:54 Here's the critical point that you'll be tested on outpatient must be reassessed within 72 hours. 14:00 No exceptions. 14:01 If they're not better, they needed admission and IV antibiotics. 14:06 This 72 hour check is your safety net. 14:08 Remember, PID treatment isn't just about checking boxes for antibiotics. 14:13 It's about preventing long term reproductive complications. 14:17 That's why we're aggressive with treatment and careful with follow up. 14:20 Let's now talk about Trichomonas vaginalis. 14:23 Trichomonas vaginalis is a sexually transmitted parasite and the most common nonviral sexually transmitted infection (STI) worldwide. According to the World Health Organization, there were approximately 156 million new cases globally in 2020. 14:42 Prevalence rates of Trichomonas vaginalis vary significantly by region and population. In the United States, the prevalence among women ranges from 8.7% to 27%, with higher rates observed in STI clinics. 14:56 Among men in the U.S., the prevalence ranges from 4% to 10%, but can be as high as 70% in partners of infected women. The infection exhibits a bimodal age distribution, peaking at ages 21-22 years and 48-51 years. 15:12 In African countries, the prevalence of Trichomonas vaginalis ranges from 2% to 30%, reflecting significant regional variability. 15:21 It is important to note that prevalence rates can vary depending on the diagnostic method used. 15:27 Nucleic Acid Amplification Tests (NAATs) are more sensitive and specific compared to microscopy, leading to higher detection rates. 15:36 The Centers for Disease Control and Prevention (CDC) highlights that trichomoniasis is not a reportable disease in the U.S., which complicates the understanding of its full epidemiology. 15:47 However, population-based studies indicate that the prevalence remains high among women over 24 years of age, unlike other STIs such as chlamydia and gonorrhea, which are more common in younger populations. 16:00 This is what you might see upon speculum examination. 16:04 Here you see a cervix that has a copious discharge. 16:08 It may not always be colored but it can be yellow or white and sometimes appear as frothy but that varies and is difficult to ascertain. 16:19 Let's now talk about the treatment. 16:21 Again, I don't think this will be on your test, but just know for the boards and the wards that metronidazole is the primary treatment. 16:29 There are alternatives such as tinidazole. 16:35 Remember that metronidazole is the preferred agent in women who are HIV infected. 16:43 Thank you for listening and good luck on your exam.
About the Lecture
The lecture Sexually Transmitted Infections: Drips/Discharges, Pelvic Inflammatory Disease, and Trichomonas Vaginalis by Lynae Brayboy, MD is from the course Gynecologic Pathology: Infections, Neoplasms and Screening. It contains the following chapters:
- Case Study and Drips/Discharges: Gonorrhea, Nongonococcal Urethritis and Chlamydia
- Pelvic Infammatory Disease (PID)
- Trichomonas Vaginalis
Included Quiz Questions
Which of the following is the primary site of infection of gonorrhea?
- Endocervical canal
- Ovary
- Fallopian tube
- Vagina
- Endometrium
A two-week-old neonate is brought to the clinic by the mother who explains that her child is wheezing. Upon examination, the infant is afebrile with a wheeze and staccato cough. The lungs are tympanitic to percussion and the eyes appear crusty bilaterally. A Gram stain of the crust is negative for bacteria but shows neutrophils. Which of the following organisms could be responsible?
- Chlamydia trachomatis
- Neisseria gonnorhea
- HIV
- Trichomonas vaginalis
- Herpes simplex
Which of the following is NOT commonly a sensitive test to identify Chlamydia trachomatis?
- PAP smear testing
- Culture
- Nucleic acid amplification test
- Non-culture and non-amplified tests
- Serology
Which of the following is NOT a complication associated with pelvic inflammatory disease?
- Endometriosis
- Infertility
- Chronic pelvic pain
- Ectopic pregnancy
- Tubo-ovarian abscess
Which of the following best describes the adhesions in Fitz - Hugh - Curtis syndrome?
- Adhesions from anterior abdominal wall to the liver
- Adhesions from anterior abdominal wall to the spleen
- Adhesions from anterior abdominal wall to the pancreas
- Adhesions from anterior abdominal wall to the colon
- Adhesions from anterior abdominal wall to the urinary bladder
Which of the following is a recommended treatment of choice for outpatient treatment of pelvic inflammatory disease?
- Ceftriaxone + doxycycline + metronidazole
- Ceftriaxone + ciprofloxacin + metronidazole
- Cefexime + doxycycline + metronidazole
- Ceftriaxone + ampicillin + metronidazole
- Cefotaxime + doxycycline + metronidazole
Which of the following is the recommended treatment of choice for outpatient treatment of pelvic trichomonas vaginalis?
- Metronidazole
- Ciprofloxacin
- Ampicillin
- Ceftriaxone
- Azithromycin
Customer reviews
2,3 of 5 stars
| 5 Stars |
|
0 |
| 4 Stars |
|
0 |
| 3 Stars |
|
2 |
| 2 Stars |
|
0 |
| 1 Star |
|
1 |
The lecture is well organised and the facts are explained clearly. I just think the lecture could be more detailed than it is.
2 customer reviews without text
2 user review without text