Playlist
Show Playlist
Hide Playlist
Spontaneous Intracerebral Hemorrhage (ICH): Management
-
Emergency Medicine Bord Intracranial Hemorrhage.pdf
-
Download Lecture Overview
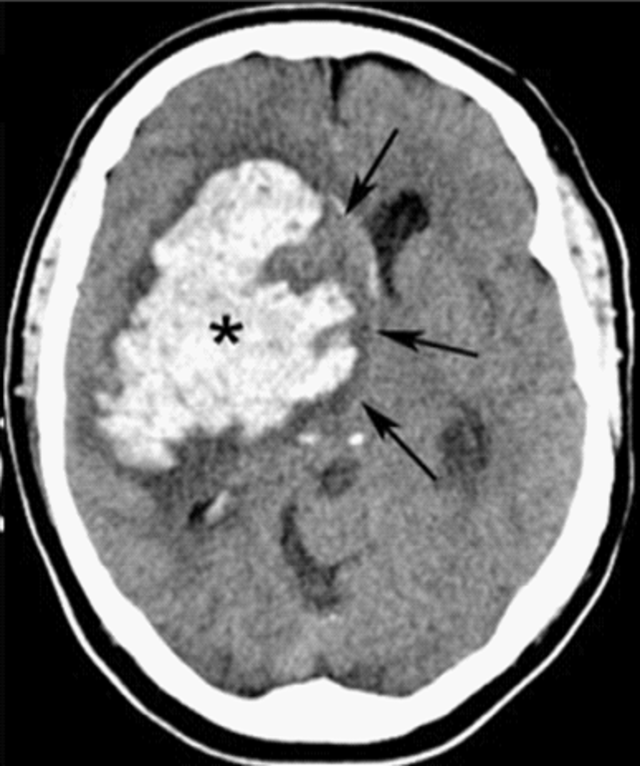
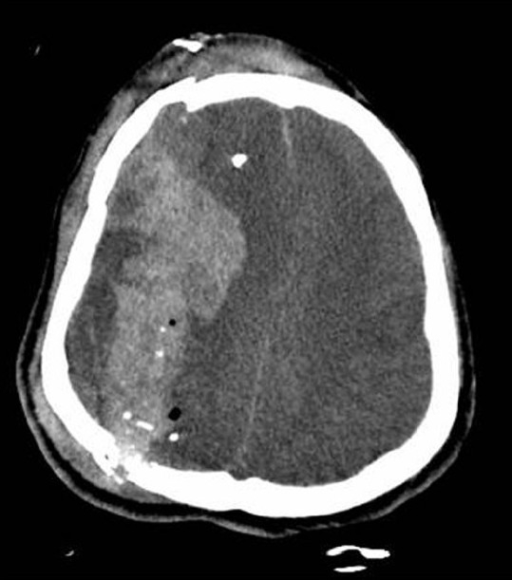
00:02 So what are those steps in managing patients with intracerebral hemorrhage? So first and foremost, airway management as indicated. So if your patient does not have a patent airway or they're not able to protect their airway, then you want to start thinking about performing intubation for those patients. 00:17 You wanna treat the elevated blood pressure. 00:20 As the blood pressure stays persistently elevated, that area in the brain that’s bleeding is gonna keep bleeding. 00:27 So you wanna try and lower the blood pressure so that bleeding stops or slows down. 00:33 The goal blood pressure is debatable and there have been lots and lots of studies out there that have looked what is the best blood pressure, where do you want it to be? Ultimately, between 140 to 160 systolic is where you want the blood pressure to be. 00:48 You don’t wanna be too aggressive about it because keep in mind that a majority of these patients have chronically elevated blood pressure. 00:54 So you’re not taking care of someone who has a normal perfect blood pressure. 00:58 And if you decrease the blood flow too much that could potentially decrease the cerebral blood flow in other areas of the brain. 01:05 So you wanna make sure you’re being cautious about decreasing the blood pressure but not decreasing it too dramatically. 01:11 You also wanna reverse coagulopathy. 01:14 Historically, we used to have few medications that would anticoagulate someone. 01:18 So it used to be someone who was on aspirin potentially or Clavix and then warfarin or Coumadin where are most common anticoagulation medications. 01:28 Now, there are novel or new oral anticoagulant medications. 01:32 And those can be tricky because they don’t have any effect on the coagulation profile. 01:39 So for instance, if a patient is on warfarin that would be reflected in the INR level. So the INR will be elevated. 01:45 If someone is on one of the newer oral anticoagulant medications, those actually are not at all reflected in the coagulation studies. 01:53 So it can be very tricky to know whether or not someone is on those. 01:57 Very key thing is to try and get that information from the pharmacy, from the family member, from the patient if they’re able to write it to you, from the medical record. 02:05 Because if someone is on an anticoagulant, you wanna make sure you reverse that. 02:09 And there’s different pathways for reversing the different anticoagulation medications. 02:13 So for warfarin or Coumadin, you can give prothrombin concentrate or you can give vitamin K or FFP. 02:22 And for the other oral anticoagulants, there’s a whole slow of different pathways that you can give to reverse those. 02:28 But the key thing is finding out whether or not someone is on it, and if they are, take them to the next steps to reverse that medication. 02:36 You also wanna reduce the intracranial pressure if there’s concern that it's elevated. 02:40 That can be done either using Mannitol which is a very potent diuretic. 02:45 You wanna be cautious about using that in the rare patient that would have low blood pressure. 02:49 Because what that can do is it can further drop the blood pressure. 02:54 You can give hypertonic saline for those patients who have low blood pressure and you can also hyperventilate the patient. 03:00 Now, what the Mannitol and hypertonic saline do is they essentially take the fluid out of the brain. 03:06 I describe it that you’re taking a brain from being a grape to making it into a raisin. 03:09 They’re essentially kind of sucking some of the water out of the brain. 03:13 And by sucking some of the water out of the brain, you’re making the size and the pressure in turn smaller. 03:19 Hyperventilation works by lowering the PCO2 levels by lowering the carbon dioxide levels which will in turn cause vasoconstriction or constricting of the blood vessels in the brain. 03:31 Yeah you can really only hyperventilate your patient if they’re on a ventilator machine. 03:36 You can’t just ask your patient to breathe more rapidly, that won’t necessarily do it. 03:40 A key thing to remember with hyperventilation is you wanna make sure that the PCO2 level, that carbon dioxide level, doesn’t go down too dramatically. 03:49 Cause again if you lower that level too dramatically, you can cause too much constriction of the blood vessels. 03:54 And if you cause too much constriction of the blood vessels, then again, you’re in a situation where the brain might not necessarily be getting enough blood flow. 04:02 The last thing you wanna do is you wanna get a Neurology consult. 04:05 Often times, these patients are quite ill and need to be admitted to the hospital. 04:08 Under the Neurology service, rarely will the neurosurgery team get involved because there’s really not too much surgical process that can be offered to these patients. 04:18 But generally, they need to be very closely watched and to be monitored and also will need physical therapy to help them work on their disability. 04:26 And a lot of critical management to get them through those initial phases. 04:31 Now, the mortality, like I mentioned, is quite high. 04:33 And their scoring system is based on the GCS, how large the volume of the intracerebral hemorrhage is on the CT scan. 04:42 If there’s any blood in the ventricular system of the brain. The location of the bleed, so is it infra versus supratentorial? Supratentorial bleeds are bleeds that are in the upper portions of the brain, the frontal lobe, the temporal lobe. 04:56 Infratentorial are bleeds that are in the cerebellum and the brain stem. 05:01 And then the age. So 80 is generally the age cut off in which the mortality increases over 80.
About the Lecture
The lecture Spontaneous Intracerebral Hemorrhage (ICH): Management by Sharon Bord, MD is from the course Neurologic and Psychiatric Emergencies.
Included Quiz Questions
Which of the following helps reduce intracranial pressure in a patient with acute intracranial hemorrhage?
- Hypertonic saline
- Nicardipine
- Hypoventilation
- Metoprolol
- Blood transfusion
What is one disadvantage of newer anticoagulant medications?
- Lack of reliable blood tests to ascertain therapeutic effect or toxicity
- Higher risk of rebound thrombosis
- Delayed onset of action
- Weaker effects
- Major decrease in cerebral blood flow
Which of the following statements is MOST ACCURATE regarding hyperventilation in patients with acute intracranial hemorrhage?
- It leads to constriction of intracranial vessels.
- It leads to increased serum carbon dioxide.
- It exacerbates bleeding.
- It increases intravascular volume.
- It is conducted in patients before endotracheal intubation.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |