Playlist
Show Playlist
Hide Playlist
Role of Platelets in Hemostasis
-
Slides Thrombus Formation Platelets.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
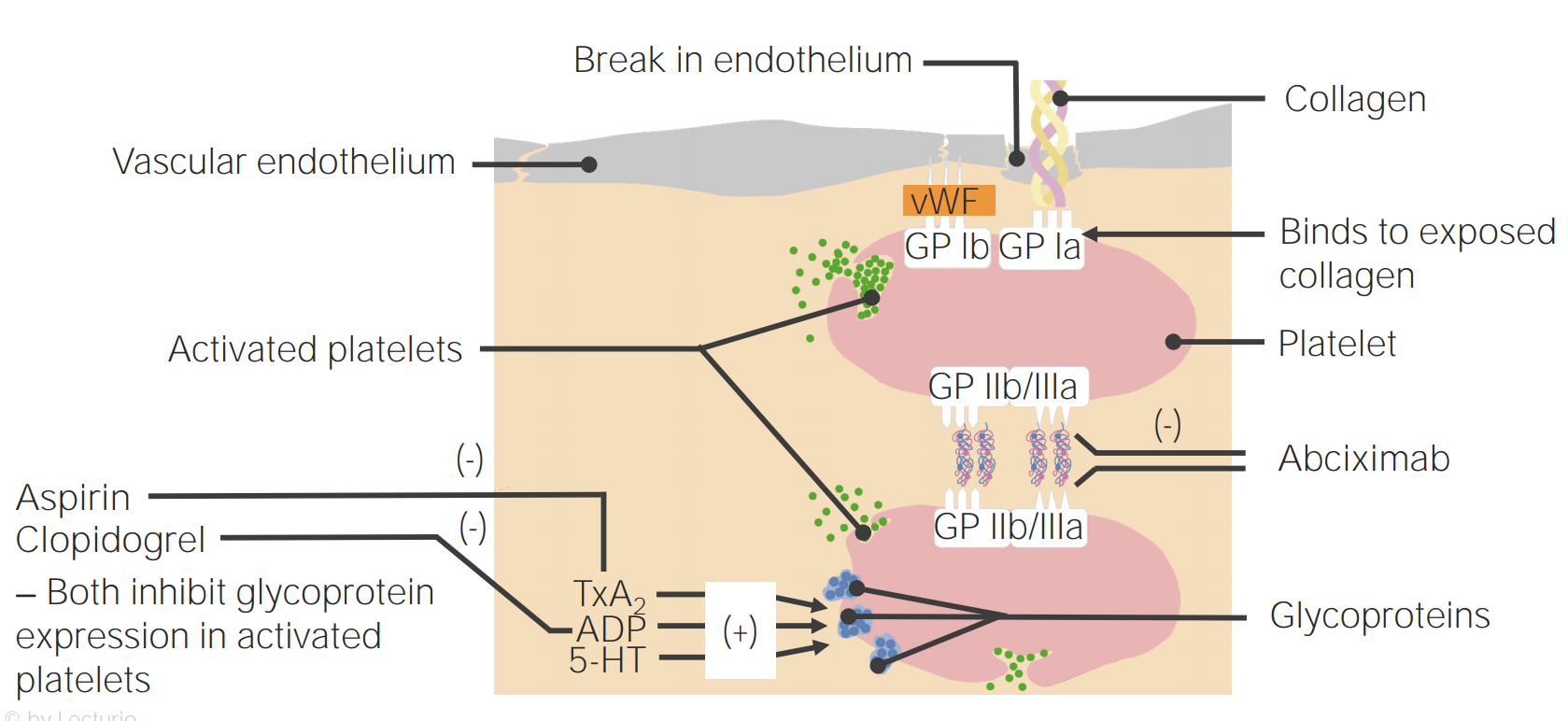
00:00 Okay, back to the components of thrombosis; platelets that are in the bloodstream, coagulation cascade that we will come back to that is going to be activated concurrently with our platelet recruitment and activation, and endothelial cells. All are going to be major players, but for the remainder of this session we're going to talk about platelets and the specifics. So, endothelial cells in the normal endothelium we have a monolayer that sits on top of the basement membrane and they're normally not activated. They are going to be, however, maintaining blood in a liquid state when they become damaged, and that damage is not just certainly just ripping them off as you see there on the right hand side, but could also be inflammation. It could also be just an activation because of additional biomarkers that are released. Once we have the activation of the endothelium, we then begin to recruit the platelets and you can see them binding now to the underlying endothelial surface. 01:09 So what's going on there? Damaged endothelium where we've lost it or it's become activated, reveals underlying collagen in Von Willebrand factor. And the platelets are able to interact with Von Willebrand factor thru their surface receptor glycoprotein Ib. In the next few set of slides, there will be lots of details. Don't get too bogged down in the details. 01:35 They're very important because they represent therapeutic targets, but it can become overwhelming so just focus on kind of the broad pictures and realize that there are interesting details and you can come back and revisit this by watching the video over and over again. In any event, platelets will initially adhere to the Von Willebrand factor that's been exposed by losing the endothelium. When the platelets bind to that surface, they undergo a shape change and they get activated themselves so that they can now interact platelet to platelet through another surface molecule, the glycoprotein IIb/IIIa complex, that's shown in the upper left hand side. That GP IIb/IIIa complex binds to fibrinogen, not the polymerized fibrin but fibrinogen and that will bridge between platelets. So we can build that definitive secondary hemostatic plug. The platelets have also undergone a shape change and they become activated, that's how we got that expression of the GP IIb/IIIa, but they're also releasing granules that will be a recruitment for other platelets that will be going by in the circulation. So, let's talk about those recruitment through the granule release. So, matrix bound Von Willebrand factor shown there on the right hand side binds to glycoprotein Ib, that's the initial step. Additionally, things that are released by platelets or by activated endothelial cells, adenosine diphosphate, thrombin, thromboxane A2 collagen or epinephrine will bind to receptors on the surface of the platelets and they will drive, number 1, the activation of the glycoprotein IIb/IIIa that allows us now to interact with fibrinogen and to interact and make a secondary interaction with additional platelet. Okay. 03:49 So there you see the additional platelet now adhered. That ADP receptor or the other molecules; thrombin, thromboxane A2, collagen, etc. will drive the metabolic pathways within the platelets involving cyclooxygenase and platelet thromboxane synthase to covert arachidonic acid precursors to thromboxane A2. So a prostaglandin metabolite that will have secondary effects and that thromboxane A2 will activate other platelets and will drive granule release. So, multiple things are going on as a result of the initial interaction with various receptors and the activation of platelet. Let's look more specifically at the different granules that are going on after activation. And again, on the left hand side, we're seeing all the various things that can drive platelet activation. So adenosine diphosphate, thrombin that's going to be made us part of the coagulation cascade, exposed collagen because we've denuded the endothelium, epinephrine release from platelets and other cells, or thromboxane A2 released by platelets are all going to be part of an activation cascade. Now I'm going to show you just the ADP receptor on the surface of platelets, that once we activate that by binding adenosine diphosphate will lead to granule release. Okay. So, binding ADP to its receptor gives us intracellular signalling. That calls all the granules, we have green granules and blue granules. I'm going to tell you more about them in a minute, but we call them into the middle of the platelet. And then we have invagination of the platelet membrane so that we can have fusion of these granules that have collected in the middle and they can get into the canalicular framework there and the granules shoes get into the canalicular framework and are released into the extraplatelet environment. So then we get release to the granular content. Very cool, very interesting, it's part of that shape change that goes on with the platelet. The green granules, now we're going to give them a name, alpha granules. And they are going to be responsible for proliferation and growth and if you think about it, hmmm, that's an important thing that platelets should maybe control because they're going to be part of the initial response to injury. Clearly, if there's been injury we need to induce vascularisation, angiogenesis, and perhaps even drive epithelial proliferation. 06:39 So there will be a number of factors that are going to be in the alpha granules that are going to be released that drive proliferation and growth. This includes something aptly titled the Platelet Derived Growth Factor, but there's also transforming growth factor beta, platelet factor IV, Von Willebrand factor, P-selectin, all these are involved in the early healing process and in the regeneration process. So those are the green granules or the alpha granules. The blue granules, they are now called dense granules and they're going to be responsible for recruiting and aggregating and activating platelets and the coagulation cascade. So platelets are doing a lot of things besides just being a plug. They're actually releasing mediators that will drive many of the important secondary effects. These dense granules contain ADP, remember ADP is one of the ways that we can activate platelet. It will also release adenosine triphosphate. So it's going to be important for driving some of the inflammatory response and providing ATP for some processes. It will release calcium, going to be very important for driving the coagulation cascade. It will drive histamine and serotonin to affect vascular flow and tone and will make polyphosphate. These are going to be important substrates for the activation of the coagulation cascade that we will revisit in detail in a subsequent session. So, big picture, because that's where we should be is that the granule contents will activate platelets and factor XII and they will also drive proliferation and growth and granule deficiencies and we'll talk about some of those in a subsequent session, can cause bleeding. So this is where the big picture that we are, we have the platelets we have talked in detail about the various components of platelet activation and driving the coagulation especially early on. We have the coagulation cascade that we're going to be talking about next and we will come back to endothelium because these are very important players. And with that, we have concluded.
About the Lecture
The lecture Role of Platelets in Hemostasis by Richard Mitchell, MD, PhD is from the course Hemostasis.
Included Quiz Questions
Which of the following participate directly in platelet adhesion to the damaged endothelium in the process of platelet plug formation?
- GPIb
- Collagen
- Fibrin
- GPIIb-IIIa
- ADP receptor
What is the function of thromboxane A2?
- Activates other platelets
- Activates GPIIb/IIIa for aggregation
- Helps the platelets bind to each other through fibrinogen
- Helps intracellular signaling
- Forms hemostatic plug
An example of a mediator released by the dense granules is...
- ...adenosine diphosphate.
- ...transforming growth factor beta.
- ...platelet-derived growth factor.
- ...platelet factor 4.
- ...von Willebrand factor.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
2 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Dr.Mitchell is very reassuring to students learning this daunting topic. I followed his advice and re-watched the videos as well as keeping the big picture in mind for each step. Now I finally can understand and find this to be very interesting to learn!
1 customer review without text
1 user review without text