Playlist
Show Playlist
Hide Playlist
Respiratory Distress: Differentiation of Consequences
-
Emergency Medicine Bord Respiratory Distress.pdf
-
Download Lecture Overview
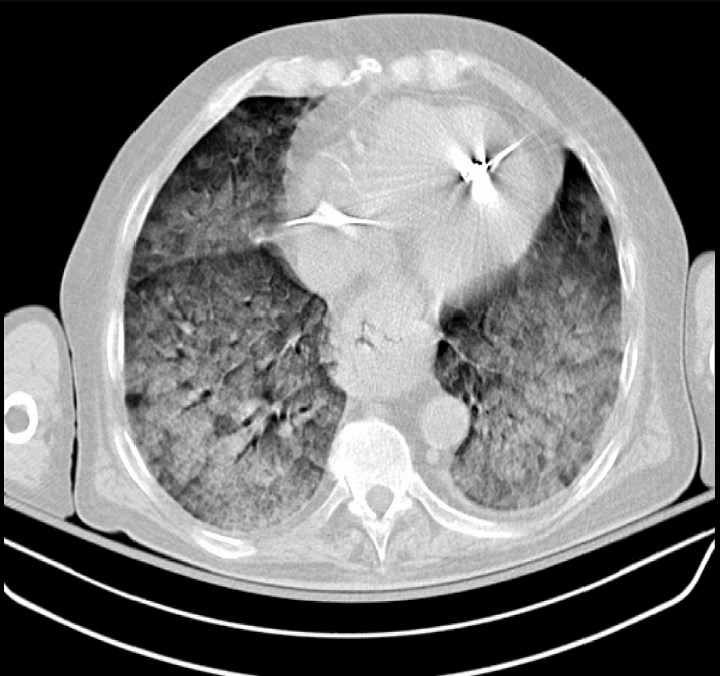
00:01 So what's on your differential of consequence. 00:03 Now, if you all remember, our differential of consequence is thinking about the things that are most life threatening to our patient. 00:10 In the ED, we wanna rule out what's the most likely thing to cause harm or to potentially kill our patient in the next few hours, days. 00:18 So what's on our differential of consequence here? There's a handful of organ systems which can cause respiratory distress. 00:26 The lungs are the main one that we think about, right? So you think about all the things that could be going on in the lungs. 00:32 But the heart can also cause respiratory distress, as can kidney failure, promus with the kidneys, liver failure as well, and then a handful of systemic stuff such as anemia or a low blood cell count. 00:45 So thinking about the lungs. 00:48 What in the lungs can cause shortness of breath? Pulmonary embolus is one that we always are thinking about in the Emergency Department and we'll be talking about that all of these in more detail in other lectures. 01:00 COPD, asthma, pneumonia, and pneumothorax, all things in the lungs that can cause a patient to present with shortness of breath. 01:09 Thinking about the heart, we think about congestive heart failure which leads to pulmonary edema, fluid on the lungs. 01:16 We think about acute coronary syndromes and we always have to make sure we're considering these. 01:20 So these are your stemis, your non-stemis. 01:25 We think about cardiac tamponade. 01:27 This is another key area that an echocardiogram can potentially really help you. 01:31 Cardiac tamponade often times presents following trauma, but also can be related to you can get large effusions related to different malignancies, as well as related to pericardial effusions. 01:44 So definitely, you wanna make sure you're thinking about cardiac tamponade. 01:48 And then acute valvular insufficiency. 01:50 Does the patient have sever aortic regurgitation, severe aortic stenosis, all of those things can lead to shortness of breath. 02:01 And then last but not least, we have a big list of other things. 02:04 Now, this is by no means all-inclusive. 02:06 There are a lot of things out there that can make someone feel short of breath. 02:10 Symptomatic anemia is one. 02:12 Every so often, I have a patient in the Emergency Department who comes in with this gradual onset of shortness of breath and every so often, I get the labs back, and I’m surprised that a patient is found to have been severely anemic. So that they have very low blood cell counts and I say to them that we found the answer for your problem and often times, those patients will need a blood transfusion. 02:34 Symptomatic anemia can be due to lot of different things, due to bleeding in the GI tract or you know, a variety of things. 02:42 But we wanna make sure that we're thinking about this. This is one of those reasons why those basic blood test that we send off can really help us out. 02:50 In the appropriate situation, you wanna think about carbon monoxide poisoning. 02:53 Definitely, it’s a good idea when these people present shorter breath especially in the winter months when people are running indoor heaters and various generators, to think about carbon monoxide poisoning, definitely after a fire kind of a situation, you wanna think about that. 03:09 Pregnancy can by in it of itself cause people to be short of breath and that’s due to various physiologic changes in the body during pregnancy. 03:19 Kidney failure, problems with the kidneys. 03:22 Patients who are maintained on hemodialysis can often times get a backup of fluid mainly into their lungs so can cause pulmonary edema. 03:31 And we know that patients from time to time are non-compliant with their dialysis treatments that they don’t go like they’re supposed to. 03:38 Especially people are vulnerable in times when they're kind of peri dialysis, when they’re about to be started on dialysis treatments. 03:45 So asking about kidney failure can be key. 03:48 And for patients who come in with severe respiratory distress and you’re not sure if they have kidney failure. 03:53 One key thing that you can do for those patients is you can go ahead and again, examine your patient. 03:58 You can look for points of dialysis access, you can look for an AV fistula. 04:02 You can look to see if they have a lining, or if they have had a prior lines that indicate that they have had kidney failure before. 04:10 And then last but not the least, thinking about liver failure with ascites. 04:14 So in the situation of liver failure, your body can develop a lot of ascites or fluid in the abdomen. 04:20 If you get significant fluid in the abdomen, then that can in turn push up on the lung fields and potentially cause shortness of breath. 04:27 So thinking about liver failure as well. 04:29 Again, your examination can help you here. 04:32 Does the patient have any stigmata of liver failure? Do they have scleral icterus or yellowing of the eyes? Does their skin appear to be yellow? So before you even get your labs back, you can start thinking about this as a possible ideology just by utilizing your physical exam. 04:49 Very important here to consider a broad differential of consequence. This is one of the areas in emergency medicine where potentially early closure can really hurt us. 04:58 So we see a patient who has a known history of COPD, who comes in short of breath, we sometimes automatically assume that this is an exacerbation of their COPD. 05:08 But in reality, you wanna also make sure they don’t have a pneumonia that they're not having a heart attack and it's not a blood clot in their lungs. 05:14 So you really wanna keep that differential of consequence broad to prevent missing a critical diagnosis. 05:20 You wanna really try to avoid early closure on these patients. 05:24 Before we wrap up our discussion of respitory distress in the ED I want to touch on COVID-19, which remains an important consideration in our differential. 05:34 In the ED, our approach starts with rapid testing We typically do both COVID and flu antigen tests together since the presentations can be similar. If these are negative, but we have high clinical suspicion, we#ll move to PCR testing. 05:49 For critically ill patients, we might consider a broader viral panel When it comes to oxygenation, we’ve learned a lot since early in the pandemic. 05:57 We now use a tiered approach. During initial resuscitation we aim for an oxygen saturation of at least 94%. 06:05 Once the patient is stabilized, we can maintain SpO2 between 90-96% . 06:11 Importantly, and this is a patient safety issue, pulse oximetry can overestimate oxygen levels in patients with darker skin. So we have a low threshold for getting an ABG in these cases. 06:23 Just like everything else we’ve discussed today about respiratory distress, we need to avoid early closure. 06:29 Yes, a patient might have COVID, but they could also have a PE. 06:33 In fact, COVID increases that risk. 06:36 And remember to adjust your oxygen targets, based on the patient’s comorbidities, lower for COPD patients, higher for pregnant women. 06:45 Looking at this chest X-ray, you can see the bilateral patchy infiltrates typical of COVID ARDS: These findings, along with inflammatory markers and the patient’s clinical status, help guide our decisions about admission and level of care. 07:01 The key message here, which ties back to our whole discussion of respiratory distress is to keep your differential broad. 07:07 COVID might be common, but it doesn’t exclude other life threatening conditions we’ve discussed today.
About the Lecture
The lecture Respiratory Distress: Differentiation of Consequences by Sharon Bord, MD is from the course Respiratory Emergencies.
Included Quiz Questions
Among the following conditions, which is the LEAST LIKELY cause of respiratory distress?
- A kidney stone which migrates and entirely obstructs the ureter
- Lung disease
- Liver failure
- Anemia
- Cardiac tamponade
Which of the following is the main reason why we must consider a broad differential of consequence for patients who present with shortness of breath?
- To avoid making the cognitive error of premature closure (i.e., failing to consider reasonable diagnostic alternatives after an initial diagnosis is made)
- To select the best laboratory examinations
- To exclude benign conditions
- To minimize the possibility of a malpractice suit
- To obtain the correct final diagnosis in the shortest time possible
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |