Playlist
Show Playlist
Hide Playlist
Resistance and Capacitance Vessels
-
Slides Structure-Function Relationships Cardiovascular System.pdf
-
Reference List Pathology.pdf
-
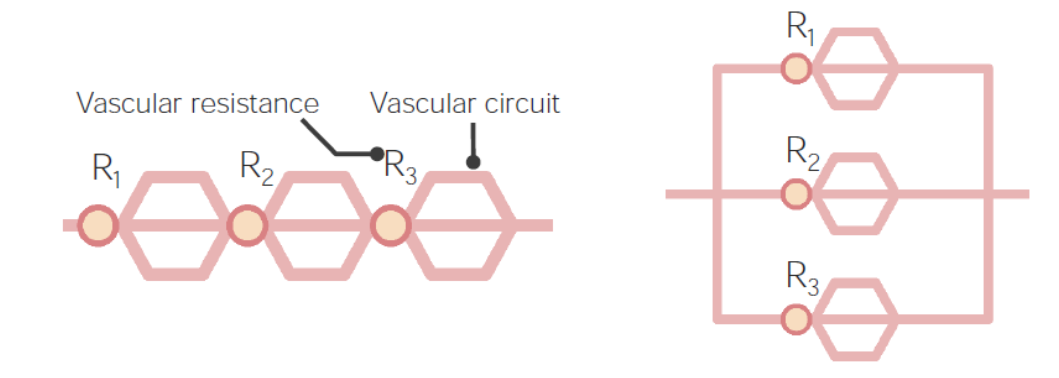
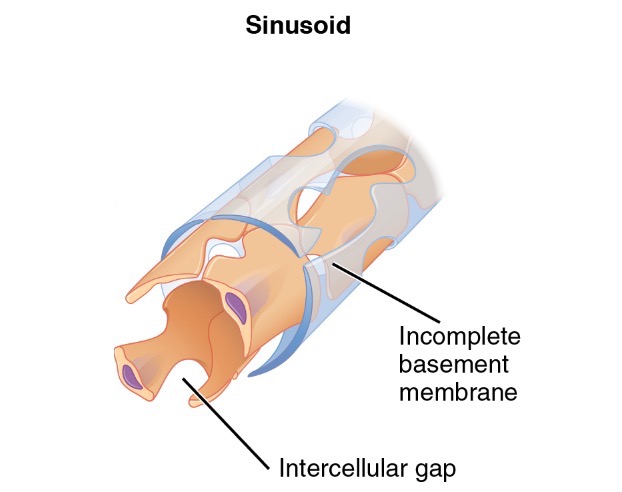
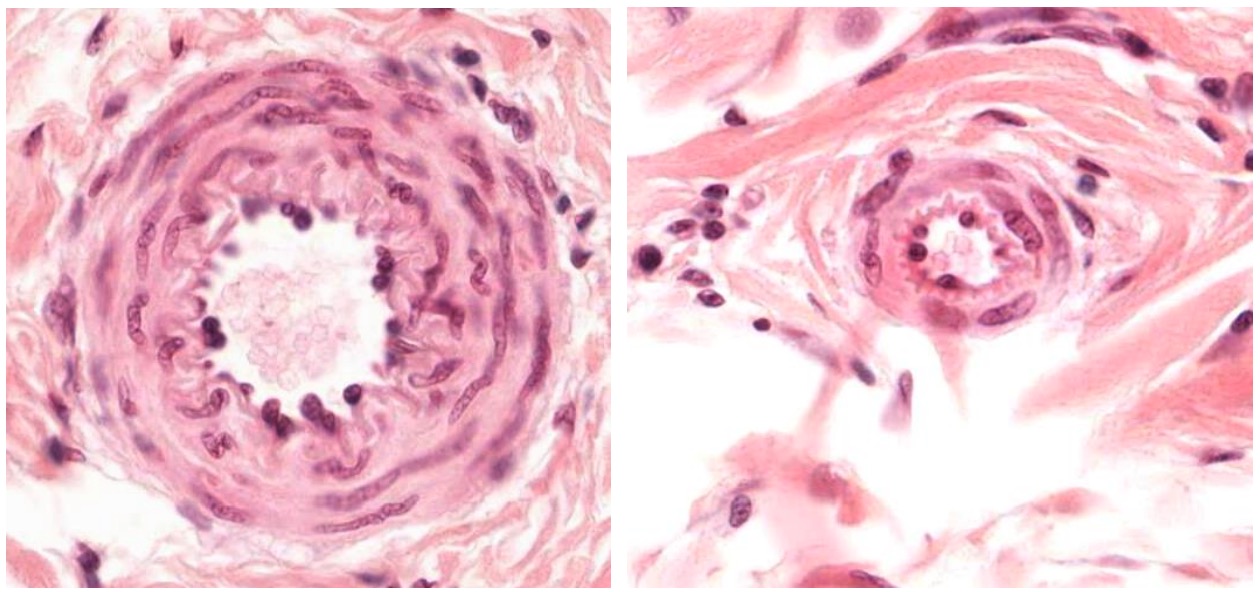
Download Lecture Overview
00:01 Okay, kind of beating a dead horse here, but we're just kind of now repeating, so it is a useful review. 00:09 So arteries, are your resistance vessels. 00:13 They are the small arteries and arterioles. 00:17 They regulate arterial blood pressure and blood flow within the organs. 00:21 They are highly responsive to hormonal and nervous stimuli. 00:24 So, I mentioned the nervous input. There is also hormonal input. 00:28 And we'll talk more about things like the renin-angiotensin system shortly. 00:34 Veins, on the other hand, are capacitance vessels. 00:37 Those are the veins in the venules. They're gonna store blood. 00:40 They can dilate up more, and they don't squeeze as well. 00:45 But that's where two thirds of the blood is stored at any given time. 00:49 Okay, bridging between the arterial circulation and the venous circulation is the capillary circulation. 00:56 That's the next level down. 00:58 Capillaries are simple tubes lined by a single endothelial cell sitting on a basement membrane, and then there are cells around the outside kind of look like fried eggs sitting on the surface there that are called pericytes, P-E-R-I-cytes. 01:15 And these are smooth muscle like cells that give some structure to the endothelium but they're not wrapped all the way around. 01:22 They're kind of loosely arranged over the surface of the endothelium within capillaries. 01:28 So again, the capillary is an epithelium on a basement membrane. 01:33 And it's going to be very thin wall specifically so that we can get gas exchange. 01:38 It's at the capillary level that we want to bring oxygen and release it into the tissues, and take carbon dioxide and get it back out. 01:45 So we need a very thin wall. 01:47 Hence just an endothelium on a basement membrane. 01:50 We also have to exchange metabolites. 01:52 We have to move glucose, and all the ions everything else to make the system run that also has to be provided by diffusion out of a very thin walled capillary. 02:05 This is now where I've identified that fried-egg look that pericytes sitting on the surface kind of scattered around on the surface of endothelium within the capillaries. 02:15 And now we're going to come out of the capillaries into the postcapillary venule. 02:20 Alright, so we've coalesced, we've gone from an artery on the left hand side to an arterial, to a capillary bed where all that nice exchange occurred, that's all coalesced back down to a postcapillary venule. 02:33 So what's so special about that? Well, this is actually going to be the site of all the action with regard to inflammation. 02:40 Ah, this is where inflammatory cells are recruited into sites where we have infection or injury. 02:46 It's also going to be where most vascular edema occurs. 02:49 So when we have increased vascular pressure, when we have increased permeability of vessels, the fluid is generally leaking out of the postcapillary venules. 03:00 So you need to pay attention to that. 03:03 One other part of the vasculature that we need to talk about and often doesn't get much attention, are the lymphatics. 03:10 Lymphatics are lined by endothelial cells too. 03:12 These are different than the endothelial cells that line the blood vessels. 03:17 Yes, they're endothelial cells, but they have some different features. 03:21 They line the lymphatics and are thin-walled structures that then drain into various lymph nodes, eventually, we'll take edema fluid from the tissue and drain it back into the circulation. 03:37 So if you have edema, it gets out. 03:40 Lymphatics pull it back in. 03:42 It gets sampled along the way in the various lymph nodes and eventually will return through the thoracic duct- main structure in the middle-. 03:52 And that returns the contents that fluid that would otherwise be lost that returns it to the left subclavian vein. 03:59 So that's how we get fluid in a circulation. 04:02 Once it leaves the vasculature, it comes back via the lymphatics. 04:07 The lymph nodes along the way, are not just kind of way stations they're actually going to be very important for antigen presentation and immune surveillance. 04:14 What's going on in that tissue that's draining that fluid? Is there infection? Is there a tumor? Is there something else going on? So the lymph nodes are going to be important elements that will allow us to kind of assess what's happening in the tissues. 04:29 Alright, so, we're gonna be talking more again about resistance and capacitance vessels. 04:34 Again, a little bit of a review, but it's an important set of concepts that you really need to kind of understand a visceral level. 04:42 Alright. So initially, we have, I'm going to just start with the blood leaving the rigt heart and coming out through the pulmonary artery. 04:52 Note that it's blue. This is deoxygenated blood even though it's an artery. 04:56 It's going to go into the arterioles in the lung, and then eventually into the capillary bed of the lung, where we'll get gas exchange, and we will release carbon dioxide, and we will take up oxygen. 05:08 Now, the blood becomes red. 05:10 So a venule here actually has oxygenated blood, That post-capillary venule. 05:16 It returns via the pulmonary veins, through the left atrium, and then through the left ventricle, and eventually out through the aorta. 05:26 High pressure system. 05:28 That high pressure system branch is into arteries and arterioles. 05:32 And then finally into a capillary bed where gas exchange and metabolite exchange occurs. 05:38 That coalesces back to a venule and back into the systemic veins, which is indicated here as a big dilated lump, mainly because that's to indicate there is high capacitance. 05:49 That returns to the right atrium, to the right ventricle, the circuit is complete. 05:55 On the right hand side here, in the high pressure, oxygenated vessels of the aorta, that's conductance. 06:04 Basically, the ascending aorta, and the descending aorta, the thoracic aorta, all those are just conductance. We're just trying to get blood out. 06:13 And then we're going to distribute it at the level of the arteries and the arterioles. 06:17 It turns out that the major resistance vessels in this entire circuit are at the level of the arterioles. 06:25 So whatever the arterioles are doing in terms of squeezing or relaxing, will determine for the most part, the pressure within the systemic arterial circulation. 06:36 At the capillary level, we're now getting diffusion. 06:39 Again, oxygen into the tissues, carbon dioxide out of the tissues, metabolites into the tissue, waste out of a tissue. 06:48 We then return blood to the venous circulation, that's our capacitance, that's where the blood is basically stored. 06:54 And we're off and running. 06:56 Okay. Blood pressure varies systematically across the vasculature. 07:01 So let's start with the left ventricle. 07:03 And basically, we're looking at the left ventricle pressure. 07:06 It goes almost from zero to 120 millimeters of mercury. Okay, that's the trough to the peak. 07:14 That's in the left heart. 07:15 But we don't see zero to 120, out in the vessels. Why? Well, that's because what's happening in the aorta is that we get that peak pressure of 120 millimeters of mercury. 07:28 But soon as we get below the level of pressure in the ventricle, the valve closes. 07:35 So we get a diastolic pressure of 80 millimeters of mercury, roughly, 90 shown here. 07:40 roughly, 90 shown here. 07:40 So thats your peak and your trough within the aorta. 07:43 As we go more distally, then we're looking at the arteries. 07:48 And now we're getting into smaller and smaller vessels for getting distribution of that big bolus of blood that came out of the aorta. 07:55 And so we're still seeing the pressure wave, but it's now diminished. 07:59 And so at the level, say, of the renal artery, we might expect 90 over 60, in terms of peak trough. 08:07 and as we go further and further away from the heart, we will see a diminution of that pressure wave. 08:13 By the time that we are into the arterioles, the pulsatility has been diminished. 08:19 Again, the arterioles, because of their resistance characteristics have now smoothed out that pressure away from pulsatile to a smooth curve. 08:28 So out of the arteries into the arterioles. 08:31 By the time that we get into the capillaries and veins, we are down to 10, 20 millimeters of mercury. 08:40 On the right side of the heart, that is we're returning we're seeing a little bit of pulsatility, but it's still a very low pressure. 08:47 And now as the right ventricle pumps, we are able to see now pulsatility again, going out into the lungs. 08:55 The pressure differential here though is more like 30 to 10, as opposed to 120 to zero, when we were looking at the left ventricle. 09:08 By the time we get out into the arteries of the pulmonary arterial circulation, again, that pressure wave has been diminished. 09:15 And in the capillary circulation of the lung, it's very low pulsatility but it's very low pressure. 09:21 This is going to be really important when we talk about things like congestive heart failure, where we have high arterial pressures backing up from the left heart into the lung. 09:30 The lung does not like that. 09:32 The lung likes to be at about 5 to 10 millimeters of mercury maximally. 09:38 And then we're into the veins of the lung. 09:40 And then we complete the circuit by coming into the left atrium and then we're off and running again. 09:45 Okay. So that's kind of, to make the point the pressures change throughout the vascular tree.
About the Lecture
The lecture Resistance and Capacitance Vessels by Richard Mitchell, MD, PhD is from the course Structure-Function Relationships in the Cardiovascular System.
Included Quiz Questions
Why is it necessary for the arterial system to be responsive to neural and hormonal stimuli?
- It allows the arterial system to regulate blood pressure and flow.
- It allows the arterial system to contain a majority of the blood volume as it is pumped from the heart.
- It allows the arterial system to increase resistance in the aorta.
- It allows the arterial system to contain a majority of the blood as it returns to the heart.
- It allows the arterial system to facilitate the closing of the tricuspid valve.
Which components of the vascular tree regulate gas exchange?
- Capillaries
- Arterioles
- Lymphatics
- Venules
- Arteries
Where in the vascular tree is the greatest increase in smooth muscle contraction seen with hypertension?
- Arterioles
- Venules
- Capillaries
- Large arteries
- Large veins
The structure and function of which of the following are correctly paired?
- Aorta - conductance
- Arterioles - diffusion
- Venules - distribution
- Veins - resistance
- Capillaries - capacitance
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |