Playlist
Show Playlist
Hide Playlist
Pemphigus Vulgaris (Review) and Staphylococcal Toxic Shock Syndrome
-
Slides Cutaneous Drug Reactions.pdf
-
Reference List Dermatology.pdf
-
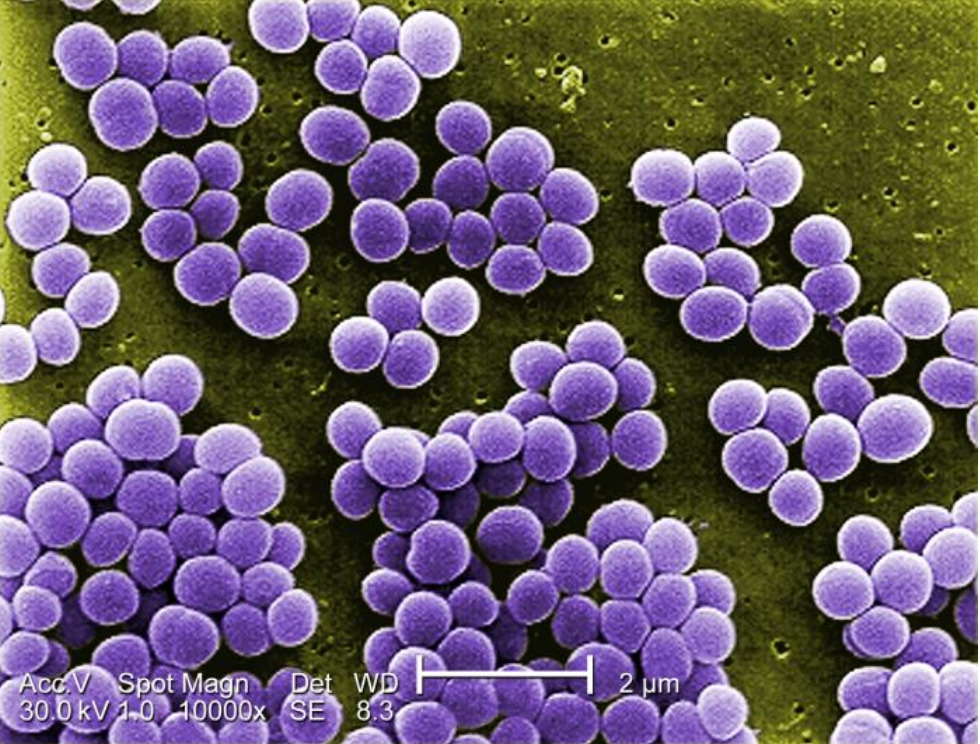
Download Lecture Overview
00:02 Okay, pemphigus vulgaris. Now, we know that this is an autoimmune bullous disease, and it's shown here on the right. It is most common in patients ages 40-60, and it's characterized by fragile, flaccid bullae on normal skin. 00:17 This is because the disease involves the keratolysis within the epidermis, rather than the divide between the epidermis and the dermal layers. 00:25 Patients experience painful erosions, bleeding from the lesions themselves, and you'll have a positive Nikolsky sign because the blisters are so thin-walled and the disease is in the epidermis that simply rubbing your thumb on the skin will lead the skin to separate. 00:41 And it's characterized, typically, by mucosal involvement, perhaps of the conjunctiva or the oral mucosa, or the genital mucosa. 00:50 Pemphigus vulgaris, however, typically involves the slow progression over weeks to months, as opposed to our patient who's describing symptoms that have progressed over 2 days. 01:00 If you were to biopsy a particular lesion in pemphigus vulgaris, you'd find acantholysis, which means there's a separation of the bonds between individual keratinocytes. 01:09 . Immunofluorescence, as well, would show anti-desmoglein immunoglobulin staining within the epidermis. 01:15 The treatment of configures for pemphigus vulgaris typically involves sending the patients to a burn unit because it can be a pretty severe disease. 01:21 You're going to use high-dose intravenous glucocorticoids, and rituximab as first line treatment, and likely add steroid-sparing agents such as azathioprine or mycophenolate mofetil once the disease is controlled. 01:35 The title of this slide is not to be confused with staphylococcal scalded skin syndrome, which is something that happens in babies. 01:41 This is staphylococcal toxic shock syndrome, and it's an acute, multi-organ illness due to an immune response to a staph aureus exotoxin. 01:51 Typically, there's some source of a staphylococcal infection somewhere in the body. 01:54 Historically, was due to tampons that had been contaminated, but oftentimes, nowadays, we'll find it in skin and soft tissue infection wounds, post-surgical incisions, sinusitis, burns, etc. 02:06 The specific toxin we're talking about is TSS toxin-1, TSST-1. 02:12 This is considered a superantigen, which means that it can activate large numbers of T cells without even needing any antigen presenting cells. 02:19 This leads to massive cytokine production with multiple system effects. 02:24 This can happen within a very short span of time, as well, within hours to 1 or 2 days. 02:30 Typical manifestations we would see would be fevers, chills, macular erythroderma, which is basically desquamation after the initial inflammatory phase. Patients may have diarrhea, myalgias, mucosal lesions, and perhaps progress to renal failure, hepatic failure, or encephalopathy. 02:47 Because of the decreased systemic vascular resistance, patients can go into distributive shock. As you can tell, these patients are sick. And importantly, since the infection may actually just be occurring in some local place and the toxin is being released systemically, you may actually have negative blood cultures, which can be somewhat paradoxical. 03:06 Nonetheless, we assume that there is a staphylococcal infection, so you're going to treat with things like vancomycin, Zosyn, and perhaps clindamycin. 03:13 The reason we add clindamycin is because it suppresses the synthesis of bacterial toxins, so it'll hopefully cool down any further release of the TSS t-1 toxin. 03:23 Now thinking about our patient, the speed of his illness is actually fairly consistent. His symptoms really progressed over 2 days. 03:31 On the other hand, nowhere in the story are we given any obvious sources of a staphylococcal infection, and the skin findings that our patient is having seems more specific than the nondescript, diffuse erythrodermic reaction of staphylococcal toxic shock syndrome. 03:46 So, we could certainly go ahead and re- examine him and look for some occult nfection that we're missing, but otherwise, I think we should take a look at something else on our list.
About the Lecture
The lecture Pemphigus Vulgaris (Review) and Staphylococcal Toxic Shock Syndrome by Stephen Holt, MD, MS is from the course Allergic and Immune-mediated Skin Disorders.
Included Quiz Questions
What is the first-line treatment of pemphigus vulgaris?
- High-dose IV glucocorticoids
- Oxacillin
- Supportive management
- High-potency topical corticosteroids
Which of the following is associated with staphylococcal toxic shock syndrome?
- Superantigens that lead to massive cytokine production
- Exfoliative toxins that bind desmoglein in the desmosomes
- Spontaneous resolution in 5–7 days
- Obstructive shock
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |