Playlist
Show Playlist
Hide Playlist
Leukemia, Lymphoma & Myeloma
-
Slides Tumor Immunology.pdf
-
Reference List Immune System.pdf
-
Download Lecture Overview
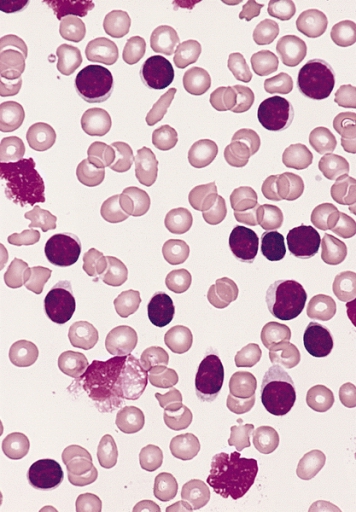
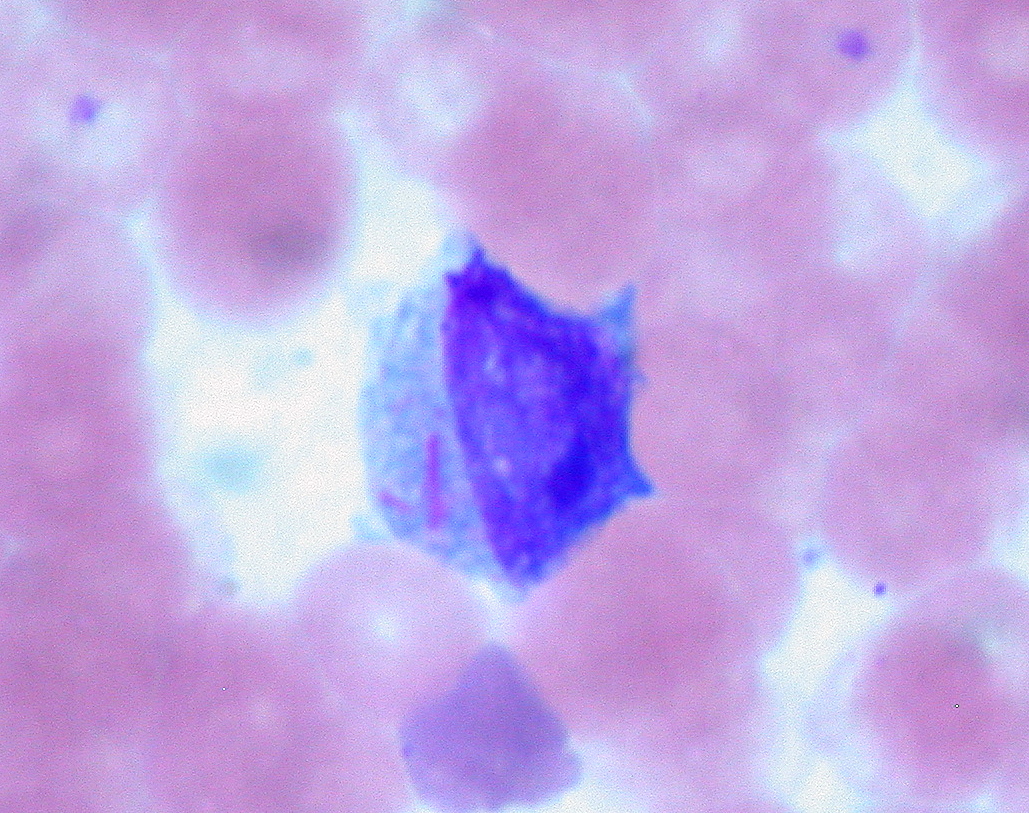
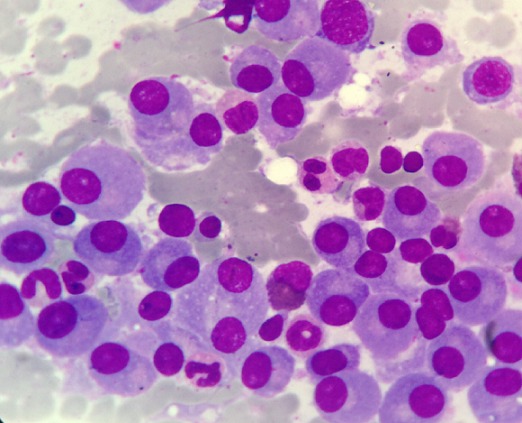
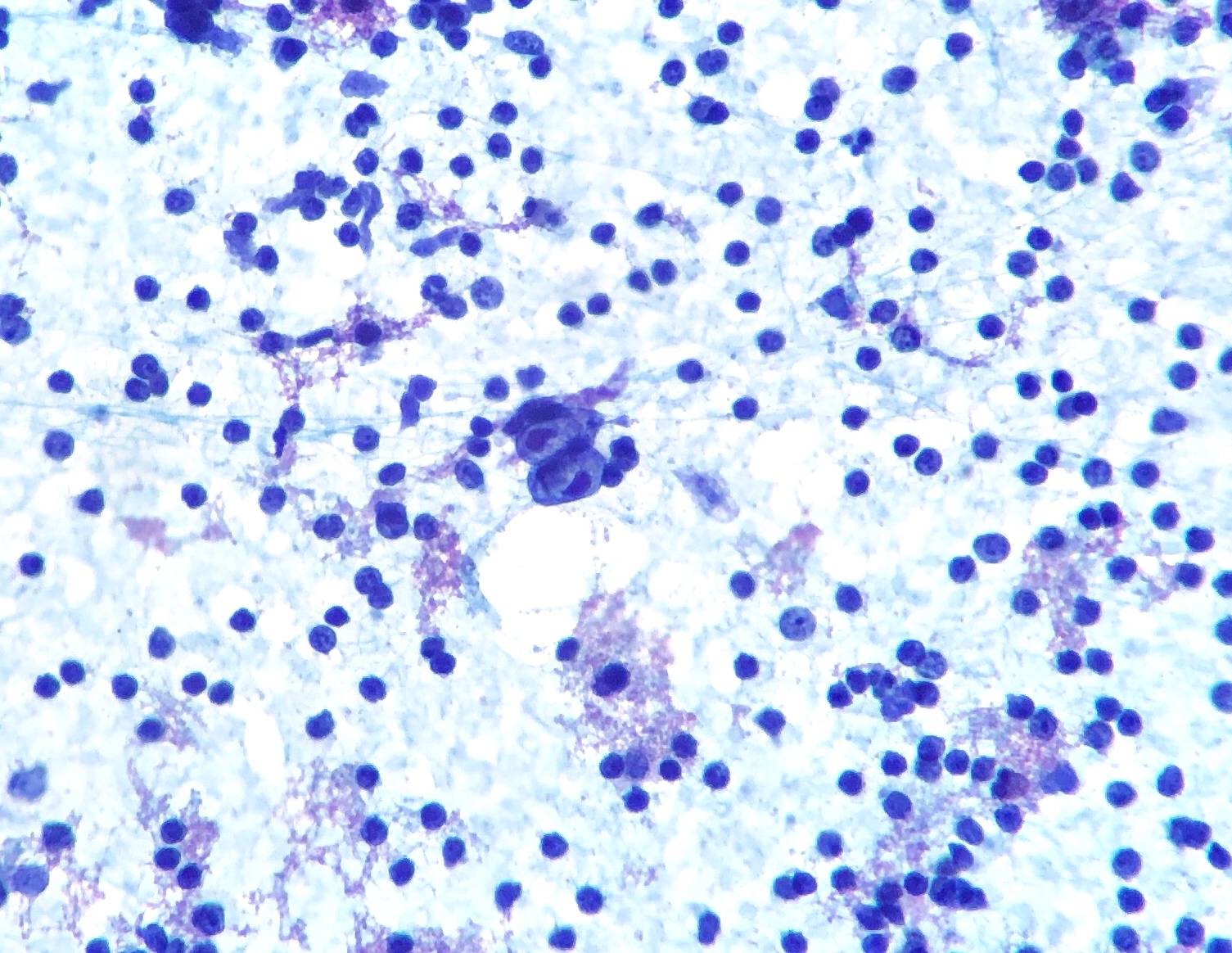
00:01 Let us look at tumors of the immune system. 00:04 Leukemia develops in the bone marrow. 00:07 There are a number of different types of leukemia. 00:11 The main ones are acute lymphoblastic leukemia, acute myeloid leukemia, chronic lymphocytic leukemia and chronic myeloid leukemia. 00:23 There are subtypes of each of these types of leukemia. 00:28 Lymphomas in contrast develop in the lymphatic system. 00:33 Lymphomas are broadly categorized into Hodgkin lymphoma and Non-Hodgkin lymphoma, with the latter comprising a diverse group of over 60 distinct subtypes including diffuse large B-cell lymphoma, follicular lymphoma, and many others. 00:49 Myelomas are tumors of plasma cells. 00:54 Each of the different main types of leukemias and lymphomas have many subtypes which are increasingly being classified based not only on their cellular origins, morphology and distribution but also on their genetic and molecular characteristics. 01:10 Here we have a stem cell that is giving rise to pre-B lymphocytes. 01:18 Acute lymphoblastic leukemia is derived from lymphoid progenitors. 01:23 About 75% of ALL cases are B-cell lineage, originating from immature pre-B cells, while about 25% are T-cell ALL, particularly in adolescents and young adults. 01:39 Blasts are present in the bone marrow and blood. 01:43 In chronic lymphocytic leukemia and lymphoma, the malignant population is mature B-cells. 01:51 In CLL, malignant cells primarily circulate in the blood and bone marrow. 01:57 When the same disease shows predominant lymph node involvement with minimal blood involvement, it's called small lymphocytic lymphoma or SLL. 02:08 CLL and SLL are essentially the same disease with different distribution patterns. 02:14 Plasma cells give rise to myeloma. 02:18 In myeloma, the clone of malignant plasma cells produces a monoclonal immunoglobulin; in other words, all the antibody is absolutely identical because it’s derived from a malignant clone of plasma cell. 02:35 T-cell malignancies are somewhat less common. 02:39 T-cells are not infected by Epstein-Barr virus, which is a major way in which B-cells can become malignant. 02:46 Also T-cells are somewhat more susceptible to apoptosis, and therefore less able to survive. 02:55 There are also myeloid leukemias derived from myeloid progenitors as well as these lymphoid leukemias that you can see on this slide. 03:07 Chronic lymphocytic leukemia is rather unusual, in that the leukemic cells have on their cell surface, a molecule that is normally present on B-cells, but also a molecule that is normally present on T-cells. 03:21 As you can see in this flow cytometry diagram, there are normally CD19+ B-cells, and then separately CD5+ T-cells. 03:34 However, in chronic lymphocytic leukemia, the cells express both of those molecules on their surface. 03:41 In other words, a molecule that is characteristic of B-cells, but also a molecule that is more normally characteristic of T-cells. 03:48 Post-transplant lymphoproliferative disorder, or PTLD, most commonly arises due to EBV infection in patients receiving immunosuppression following organ or tissue transplantation. 04:06 While many cases are EBV-driven as described, about 30% of PTLD cases can be EBV-negative. 04:15 PTLD ranges from benign polyclonal proliferations to aggressive monoclonal lymphomas, and typically improves if immunosuppression can be reduced. 04:26 Prior to a renal transplant, this woman had memory T-cells responding to Epstein-Barr virus. 04:33 The Epstein-Barr virus infection was controlled by the T-cells. 04:39 However following a transplant, the immunosuppressive drug cyclosporine has made the memory cells non-responsive. 04:48 And there is a polyclonal increase in EBV infected B-cells. 04:54 There becomes a situation in which there is uncontrolled EBV infection which drives B-cell proliferation. 05:07 The polyclonal B-cell proliferation will improve if the cyclosporine is stopped. 05:14 However with ongoing proliferation, Myc translocation can occur within the B-cells. 05:23 There is a malignant transformation resulting from this Myc translocation, and the development of lymphoma. 05:32 The polyclonal growth of B-cells has increased the risk for this translocation to occur. 05:38 The monoclonal B-cell proliferation will continue after cyclosporine is stopped, and the patient develops the symptoms of lymphoma. 05:50 In multiple myeloma, there are plasma cells in the bone marrow that become malignant. 05:58 Multiple myeloma diagnosis requires evidence of end-organ damage summarized as CRAB: elevated calcium, renal insufficiency, anemia and bone lesions. 06:12 Myeloma can also be diagnosed in patients with certain biomarkers even without these symptoms, including high percentages of clonal plasma cells in the bone marrow. 06:24 And therefore, a clone of rapidly replicating plasma cells pumping out huge amounts of antibody of a single specificity develop. 06:38 They produce what is referred to as a paraprotein. 06:41 And this can be detected on a electrophoretic gel. 06:45 We can see the paraprotein band in the gamma region from the patient on this gel. 06:52 In contrast, in a healthy individual, that monoclonal band is missing because their antibodies are totally polyclonal; a very huge mixture of different specificities.
About the Lecture
The lecture Leukemia, Lymphoma & Myeloma by Peter Delves, PhD is from the course Tumor Immunology. It contains the following chapters:
- Tumors of the Immune System
- Chronic Lymphocytic Leukemia
- Post-Transplant Lymphoma
- Multiple Myeloma
Included Quiz Questions
Infection with which of the following pathogens is particularly associated with post-transplant lymphoproliferative disorder?
- Epstein–Barr virus
- Human papillomavirus
- Hepatitis C
- Varicella zoster virus
- Cytomegalovirus
Which of the following tumors is INCORRECTLY matched to the associated progenitor cells?
- Lymphoma - myeloid progenitors
- Leukemia - myeloid progenitors
- Leukemia - lymphoid progenitors
- Myeloma - plasma cell progenitors
- Lymphoma - lymphoid progenitors
A patient presents with large numbers of mature B cells in their blood. Which of the following is the most likely diagnosis?
- Chronic lymphocytic leukemia
- Acute lymphoblastic leukemia
- Non-Hodgkin's lymphoma
- Multiple myeloma
- Chronic myeloid leukemia
Which of the following best describes paraproteins?
- Monoclonal immunoglobulins or immunoglobulin fractions that are produced by a clonal population of B-cell lineage cells
- Polyclonal immunoglobulins or immunoglobulin fractions that are produced by a clonal population of B-cell lineage cells
- Polyclonal immunoglobulins or immunoglobulin fractions that are produced by a clonal population of T-cell lineage cells
- Monoclonal immunoglobulins or immunoglobulin fractions that are produced by a clonal population of T-cell lineage cells
- Polyclonal immunoglobulins or immunoglobulin fractions that are produced by a nonclonal population of B-cell lineage cells
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |