Playlist
Show Playlist
Hide Playlist
Hypoxia – Lung Physiology
-
Slides 02 LungPhysiology Basic.pdf
-
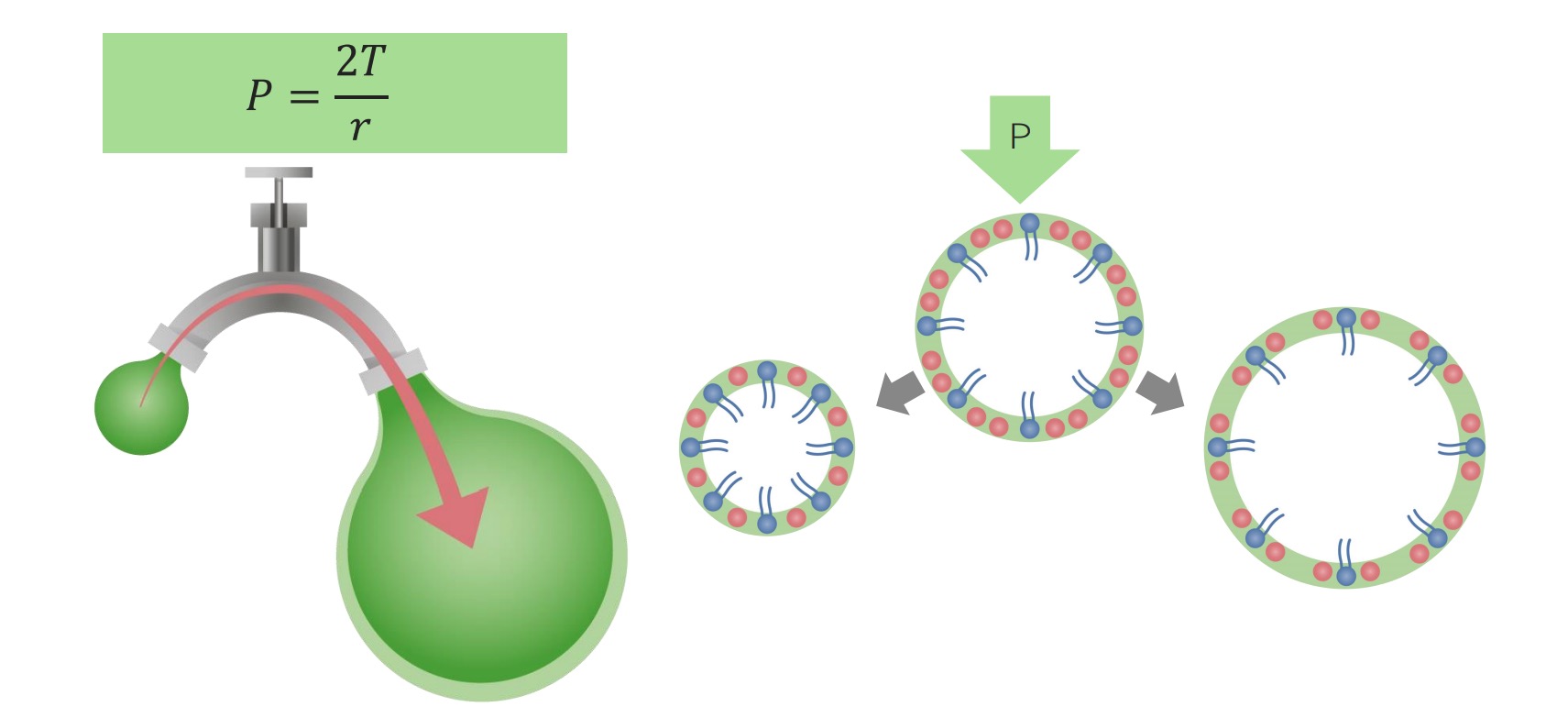
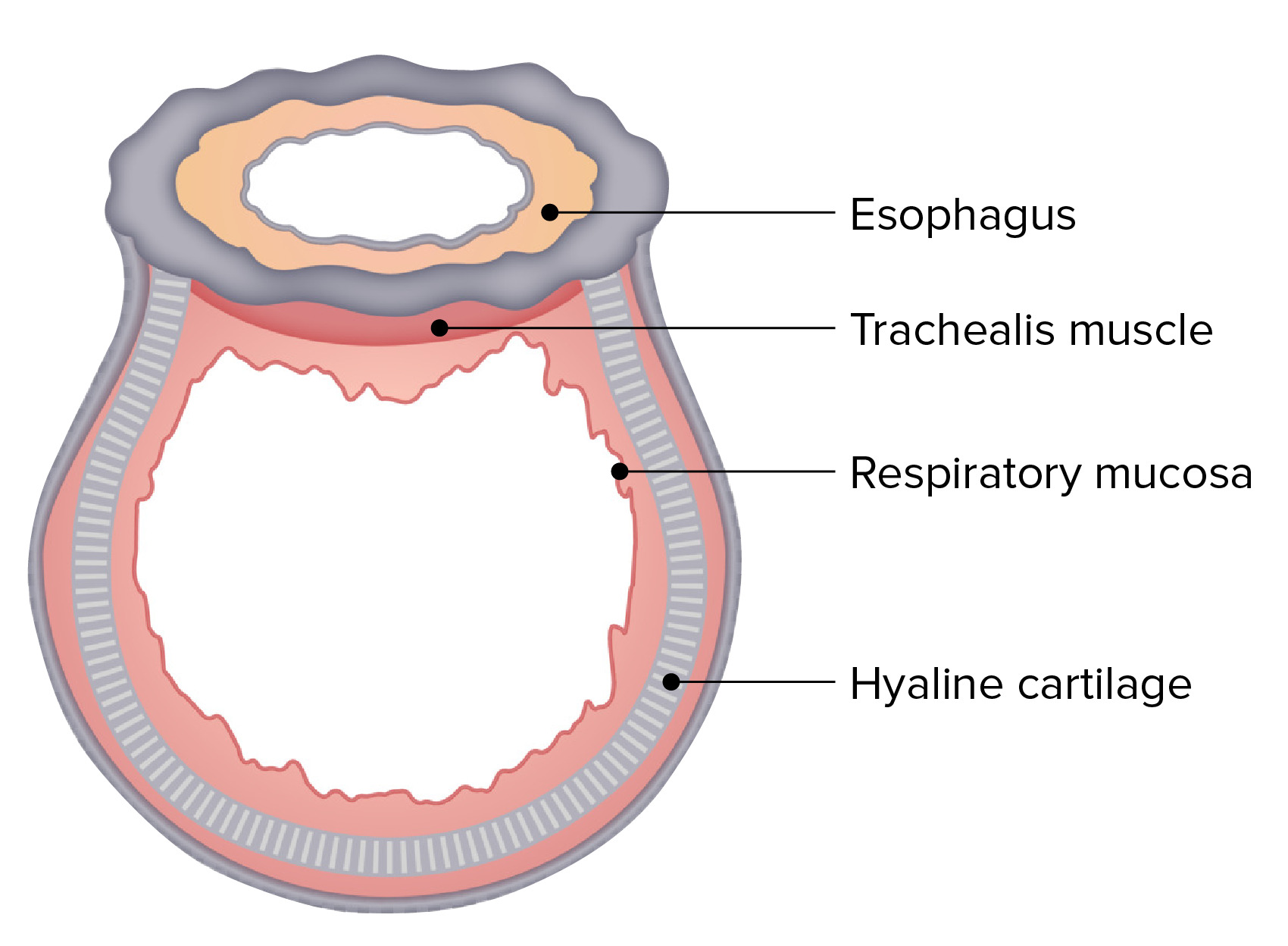
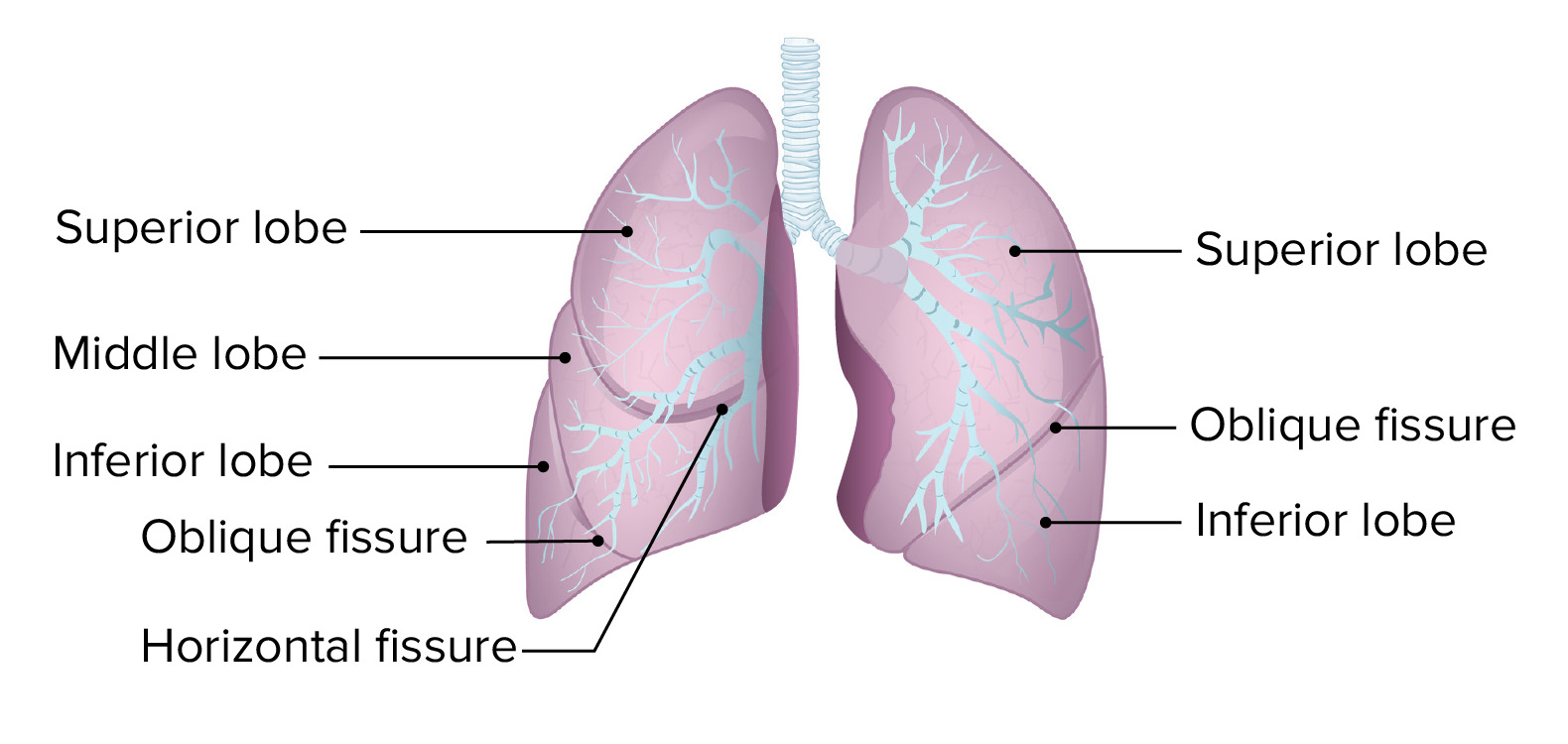
Download Lecture Overview
00:01 when ventilation occurring as the pH comes back up again and the CO2 goes down. 00:01 So in the last part of this talk, I am going to talk about the factors that cause arterial hypoxia and these are down to five different factors. 00:09 1. Diffusion limitation and we discussed that already. And that is related to how oxygen gets in the alveolar, into the pulmonary capillaries. The factors that affect the diffusion are surface area, blood supply to the alveoli, and the gap that has to be crossed by the diffusing oxygen molecule. The thickness of the alveolar membrane. Clearly if you inspire air at a lower inspired oxygen concentration that could cause hypoxia. That is a pretty obvious situation and it is not terribly relevant in most circumstances. 00:44 2. Underventilation. If you are not moving the air enough will cause hypoxia and then right to left shunts is the fourth mechanism that is where blood that is deoxygenated in the pulmonary artery for some reason gets shunted past the pulmonary capillaries directly into the pulmonary veins delivering unoxygenated blood into the pulmonary veins and therefore to the systemic circulation. 3. Ventilation perfusion inequality we have discussed already to a certain extent. Essentially what that is a right to left shunt occurring at the micro levels and in individual alveolar areas where you may get alveolus which have not been ventilated and the artery supply to that area it is still open and not constricting will allow blood which is deoxygenated to go straight past the alveoli and back into the pulmonary venous circulation. 01:37 So these are mechanisms that would describe why somebody may have arterial hypoxemia. 01:43 So let's talk about each of these in more detail. Oxygen diffusion we have discussed already is dependent on Fick’s Law so is affected by the surface area and that is reduced in the emphysema and surgical removal of parts of the lung. It's affected by the barrier of thickness and if you have got increased barrier to the pulmonary fibrosis or pulmonary edema that will affect oxygen transfer. And also it's importantly it is affected by the reduced blood supply to the lung and that occurs in pulmonary artery disease, either pulmonary embolism or pulmonary hypertension. All of those will lead to less oxygen being transferred across the alveolar membrane and therefore reduced oxygen diffusion. Another factor that affects transfer factor and measure how well oxygen is getting in from the alveoli to the blood is the concentration of haemoglobin, and that actually is not a cause of hypoxia itself but is a cause of tissue hypoxia because if your haemoglobin is low in quantity then delivery of oxygen to the tissues will be reduced. And that would be despite having normal oxygen concentration in the blood and normal haemoglobin oxygen saturation. 02:53 The second cause of hypoxia reduced inspired oxygen pressure. Well if you take somebody to the top of the Mount Everest and you measure their PO2 it would be incredibly low. Right so this was done fairly recently with Intensivist from my university and they discovered they had oxygen saturations which were barely recordable when they were on top of the Mount Everest and it appeared to about 30 mm of Hg. Obviously mostly people don’t get to top of Mount Everest without oxygen however many people do fly. And the cabin pressure when you are flying, at an altitude of about 5000 to 8000 feet so that oxygen saturation may be a little about 3% lower in the normal person than when you are at sea level and that is not really going to affect healthy people at all. But it is important to have chronic respiratory disease because they may have borderline oxygen saturation. They may be running about 92, 93 and that 3% will make a substantial difference to how they feel whilst flying. And these patients may need oxygen supplementation during the flight. Now 8000 feet is not that high and there are many places in the world where actually people live at that height and that can be relevant for those patients who have chronic lung disease and living in relatively high altitude. 04:13 The third cause is under ventilation. This is where you are unable to shift the air in and out of the lung as well as you should be able to and that would cause what we call type 2 respiratory failure where not only you get a fall in the oxygen concentration and that is relatively small for a oxygen concentration normally but the carbon dioxide level will be increased, because you are under ventilating. You are unable to get the carbon dioxide out of the system. And this occurs largely in situations where there is no disease of the lung itself. So the big list of causes are outside the lung. Reduced central nervous systems drive. So if I give somebody a sedative that will lower their respiratory drive respiration and may cause some degree of type 2 respiratory failure. If the nerves supplying the muscles which are meant to move during respiration are damaged in some way then again you may get under ventilation and that occurs in Guillain-barre syndrome and phrenic nerve palsies etc. The muscles themselves are if they affected by disease such as myasthenia gravis, muscular dystrophies, motor neuron disease, then you end up with under ventilation occurring. Of course the mechanics of the chest wall is very important. So if you have somebody who is obese or their spine has a curvature or a severe curvature, or the ribs are broken on both sides of the chest, causing what we call flare of the chest then all of those conditions will make the mechanics of ventilation very difficult and potentially cause hyperventilation and a rise in CO2 and fall in oxygen. And the same for extensive pleural disease. You have extensive pleural thickening that basically grips the lungs and prevents them from moving. 05:50 It has to be bilateral normally to cause problems because one lung can normally compensate for the loss of the other one. 05:57 Now there are lung diseases which cause under ventilation and in fact if you look at the people coming into hospital that is probably the commonest cause of under ventilation and that is COPD. And severe acute asthma. And that is where the airways are very tight. 06:10 And so actually you can’t shift the airways in and out of the lungs enough to supply the alveoli and that leads to a degree of hyperventilation. Right to left shunts, this actually is only commonly and rarely occurs pneumonia where you have consolidated lung and the pulmonary artery delivering blood to consolidated lungs will means that there are no alveoli consolidation itself, means the alveoli will have no oxygen in them so the delivered blood cannot be oxygenated in that consolidated lung and will be returned to the left side of the heart in a deoxygenated state. And the heart makes sure that the deoxygenated blood plus the returning from the normal parts of the lung means that somebody may be hypoxic. There are other conditions where you get right to left shunts, hole in the heart, congenital heart disease, and unusual conditions called pulmonary artery venous malformations where the pulmonary artery and the pulmonary vein are linked directly by anatomical malformation. Those are very rare. 07:09 This is an example of what happens in the consolidation with right to left shunt. You can see this patient has a bad pneumonia of the right hand side with white shadowing and that area reflects part of the lung where no oxygen uptake can occur. So if 25% of the circulation from the pulmonary artery is being delivered to that area then now will return to the heart at the same concentration of the oxygen as it came in which is 40 mmHg and then it will mix with oxygen, with oxygen replete blood being delivered to the rest of the lung and the end results will be that your pH will be about 85 mmHg which is significantly hypoxic. 07:51 The last cause of hypoxia was ventilation perfusion mismatching. It is the equivalent to the mini right to left shunts occurring through out the lung and they occur actually in very long lung conditions, pulmonary emboli, pneumonia, pulmonary oedema, atelectasis, asthma, COPD although these conditions have a little bit of V/Q mismatch occurring and contributing towards the hypoxia. And so in practice it is pretty one of the commonest cause of arterial hypoxia in clinical medicine. This is a diagram to show in a bit more detail the one which is important is probably a) on the left hand side that is where you can see the alveolus has been blocked and the oxygen concentration there is low but it is still having blood delivered. So that is the mini shunt occurring of deoxygenated blood going straight past the alveolus and back into the systemic circulation at a low level of oxygen. The other side, on the right hand side, shows a situation where you have no blood delivery but what happens there is that although the alveolus is being ventilated and there is no blood being delivered that means there is no actual oxygen uptake that occurs that is basically a wasted part of ventilation. 09:00 The last slide of day is about additional functions of lung. Now we have talked about oxygen uptake getting rid of carbon dioxide but there are quite a few other functions of the lung. It is an immunological organ. If you are exposed to microorganism in the lung that will cause undoubtedly immunoresponse and that is important to protect you against infection, against subsequent infection. It also is a filter. Any organism that manages to make it into the venous blood will go to the right side of the heart and then it will be distributed through the lung from the pulmonary artery circulation and that can filter out bacterial infection and stop that from becoming a significant problem. That filter process also occurs when you have small clots occurring perhaps in the deep veins of your leg. They can move up to the lung and they will be filtered out by the lung. Now that may cause pulmonary embolus that cause lung disease but a clot that reach the systemic circulation can cause a stroke, it cause infarction of your gut, and infarction of your leg. So in fact it is actually a safer process to have it filtered by the lungs, than reach the systemic circulation. 10:08 And the pulmonary circulation is a reservoir of blood. If you need that for whatever reason. 10:14 And there are various metabolic processes the lung does. It converts angiotensin I to its active form and it synthesizes various things such as coagulation factors and it activates other metabolic factors such as bradycardia and histamine etc. But the major function of the lung is transfer of oxygen to the blood, excretion of carbon dioxide, and because of that excretion of that carbon dioxide it’s controlling pH. 10:40 So just to summarize the learning points on lung physiology: • Ventilation is active expansion of the chest falling on inspiration followed by passive expiration on your at rest due to static recall or elastic recall of the lungs. 10:55 • Gas exchange is by diffusion. Oxygen gets into the blood from the alveolus. 11:01 • Carbon dioxide gets from the blood into the alveoli and that is dependent on Fick’s Law that we described today. • Oxygen transport to tissues, oxygen that is largely bound to haemoglobin, very small amount dissolved in blood as well. Respiration is largely controlled by the brain stem and medulla, and the pons and increased ventilation is the response mainly to the increases in carbon dioxide level or decrease in pH. 11:28 • Respiration is vital for excreting acid due to this relationship between carbon dioxide, bicarbonate, and acid concentration. • Hypoxia can be caused by five mechanisms, reduced the amount of oxygen in inhaled air and under ventilation of the lungs reduced diffusion across the alveoli membrane of the oxygen from the alveolus, right to left shunt, and V/Q mismatching. 11:55 And thank you for listening.
About the Lecture
The lecture Hypoxia – Lung Physiology by Jeremy Brown, PhD, MRCP(UK), MBBS is from the course Introduction to the Respiratory System.
Included Quiz Questions
Which of the following factors does not cause arterial hypoxia?
- Hyperventilation
- Hypoventilation
- Decreased inspired O2 (PIO2)
- Right-to-left shunts
- Ventilation/perfusion mismatch
Which of the following does not limit oxygen diffusion?
- Respiratory muscle weakness
- Pulmonary embolism
- Pulmonary emphysema
- Cystic fibrosis
- Reduced Hb concentration
In an aircraft cabin which is pressurized to an altitude of 5,000 to 8,000 feet, oxygen saturation may drop by how much?
- 3%
- 5%
- 8%
- 9%
- 10%
In which of the following scenarios would there be a decrease in PO2 associated with a rise in PCO2?
- Use of sedatives
- Hyperventilation
- Right-to-left shunt
- High altitudes
- Low Hb concentration
Which of the following conditions induces respiratory muscle weakness and consequently hypoventilation?
- Myasthenia gravis
- Obesity
- Flail chest
- Kyphoscoliosis
- COPD
Which of the following conditions commonly develop right-to-left shunts?
- Pneumonia
- Sarcoidosis
- Tuberculosis
- COPD
- Pulmonary embolism
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |