Playlist
Show Playlist
Hide Playlist
HIV Disease: Clinical Course, Treatment & Prophylaxis – Secondary Immunodeficiency Diseases
-
Slides Secondary Immunodeficiency.pdf
-
Reference List Immune System.pdf
-
Download Lecture Overview
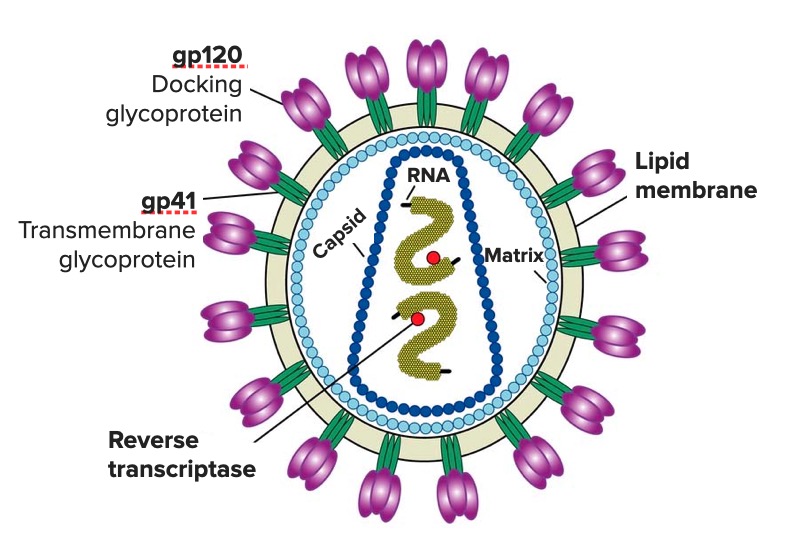
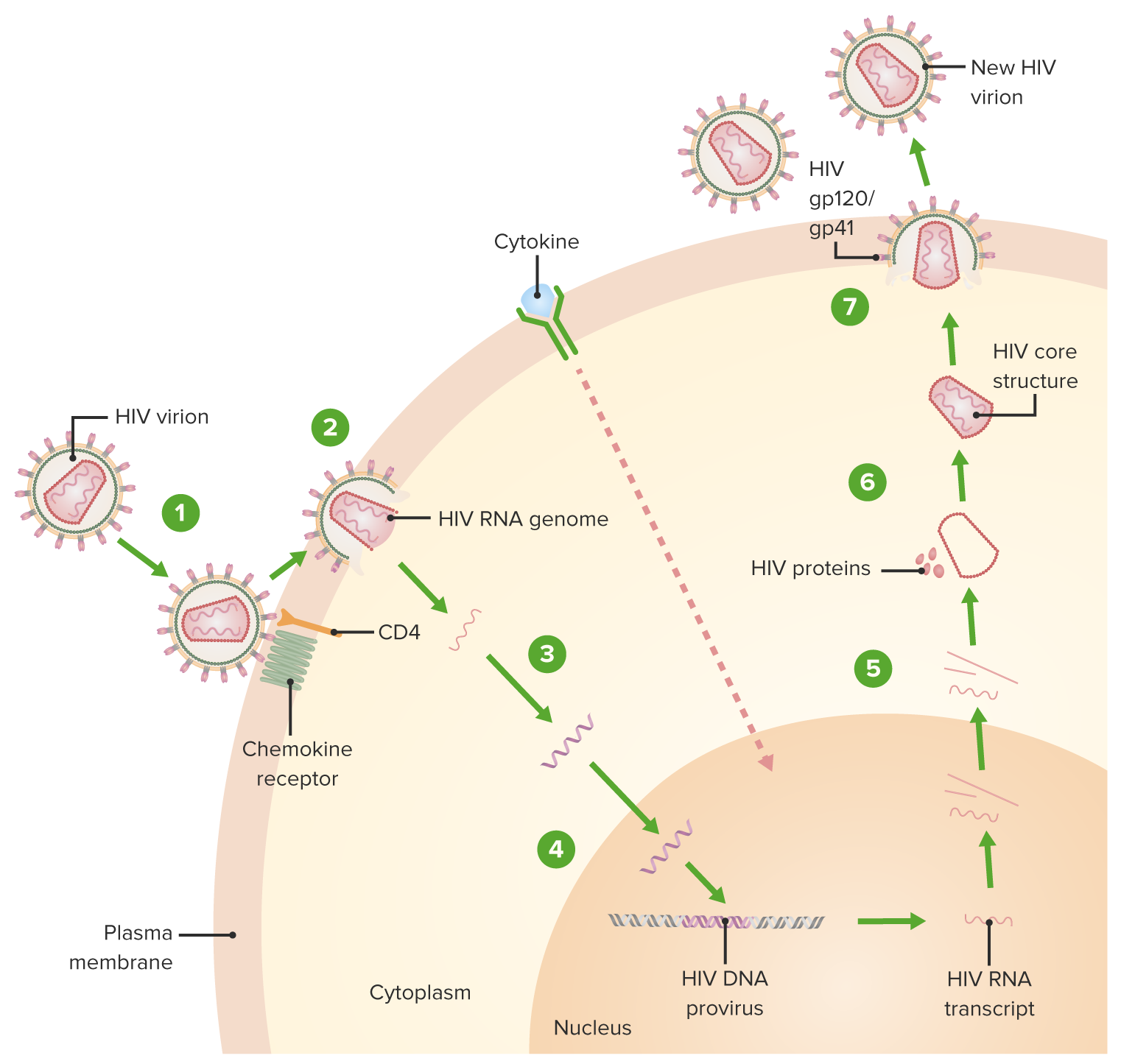
00:01 Let’s look at the clinical course of HIV disease. 00:05 If you look at the yellow line first of all, this is the amount of viremia, measured by the amount of HIV RNA that’s present. 00:15 As you can see, following the initial infection, the amount of virus RNA rapidly increases. 00:24 If you look at the blue line, which is the number of CD4 T-cells present, you can see that they decline. 00:34 At this point, following primary infection, there is the acute HIV syndrome with wide dissemination of virus, and a seeding of lymphoid organs with the virus. 00:49 However, within a small number of weeks, it seems like things are going well. 00:54 The number of CD4 T-cells begins to increase, and the amount of virus decreases. 01:03 However the virus is not being eliminated, it is entering a period of clinical latency. 01:11 Then after a very variable period of time, which may be a short number of years or maybe many, many years later. 01:19 The individual will begin to develop constitutional symptoms, there will be opportunistic infections, and opportunistic tumors that begin to arise. 01:31 And the amount of virus begins to increase. 01:35 And the number of CD4+ T-cells begins a rapid decline. 01:43 The patient then has the Acquired Immune Deficiency Syndrome, and without medical intervention, death would be more or less inevitable in the vast majority of individuals. 01:57 Fortunately, the use of antiretroviral drugs can prevent this process leading to death. 02:07 Here we see the amount of antibody and cytotoxic T-cells being produced, and the virus particles in the plasma. 02:16 So again, looking initially at the yellow line, you can see that the virus goes up following an initial infection and then radically goes down, looking at virus particles in the plasma. 02:28 You’ll see that it looks like a good immune response is being developed. 02:32 In the blue line, you can see that cytotoxic T-lymphocytes specific for HIV is being produced. 02:40 Cytotoxic T-lymphocyte response is being produced. 02:42 You can see that there are antibodies against envelope proteins. 02:46 Gp120 being produced; the red line there. 02:50 And the green line you can see that there are antibodies against p24, another component of the virus. 02:55 So everything looks to be good, the immune response is kicking off and the virus is going down. 03:02 But then over time, the immune response will decline and particularly the virus particles will come back up. 03:10 And the most crucial decline here as we saw on the previous slide, is the decline in CD4+ T-cells. 03:22 So what are the major hurdles to elimination of HIV infection? Well there are long term reservoirs of HIV that are established, which include the HIV being latent within macrophages and within memory T-cells. 03:40 The extremely high mutation rate of HIV leads to an evasion of the host immune responses, and to resistance to anti-retroviral drug therapy. 03:55 The clinical features of HIV infection depend upon the particular stage of the disease. 04:01 So during the acute phase, there is a fever, a headache, sore throat; really symptoms that are very similar to a flu-like illness. 04:11 During clinical latency, there is a declining blood CD4+ T-cell count. 04:17 And then when the disease progresses to become the acquired immune deficiency syndrome, there is a whole range of opportunistic infections that the hosts become troubled with. 04:32 And these range across the whole spectrum of different types of pathogen - protozoa, bacteria, fungi, viruses. 04:40 And you can see some of the more important ones listed there. 04:44 In addition to being more prone to opportunistic infection, there is a increased instance of certain tumors. 04:52 So lymphomas, including Epstein-Barr virus-associated B-cell lymphomas, Kaposi’s sarcoma and cervical carcinoma. 05:02 There is also encephalopathy, wasting syndrome, HIV associated nephropathy and immune reconstitution inflammatory syndrome. 05:17 So how do we treat HIV infection? Well the mainstay of treatment is anti-retroviral therapy. 05:26 And there are a number of anti-retroviral drugs that have been developed. 05:31 These include the non-nucleoside reverse transcriptase inhibitors, the nucleoside reverse transcriptase inhibitors, the protease inhibitors, fusion inhibitors, entry inhibitors such as CCR5 antagonists, integrase strand transfer inhibitors. And a combination of drugs being used as highly active anti-retroviral therapy, which comprises three of more drugs from at least two different classes. There is also the possibility of treating HIV post-exposure. Obviously preventative measures are best, but immediately following exposure, commencing within 72 hours of exposure, there are drugs-- anti-retroviral drugs that can be given. These must be taken for 28 days following exposure to HIV. And again, a combination of two or three anti-retroviral drugs is employed.
About the Lecture
The lecture HIV Disease: Clinical Course, Treatment & Prophylaxis – Secondary Immunodeficiency Diseases by Peter Delves, PhD is from the course Immunodeficiency and Immune Deficiency Diseases. It contains the following chapters:
- Clinical Course of HIV Disease
- Treatment and Prophylaxis
Included Quiz Questions
Post-exposure prophylaxis for exposure to human immunodeficiency virus (HIV) must commence within which of the following time frames?
- 3 days
- 24 hours
- 7 days
- 14 days
- 28 days
Which of the following may be detected in the serum of patients with HIV infection following the acute phase?
- Anti-envelope glycoprotein GP120 antibodies
- Anti-p60 antibodies
- Envelope glycoproteins E1 and E2
- Glycoprotein GP3
- Anti-DENV Envelope protein DIII
All EXCEPT which of the following are major hurdles to elimination of HIV infection?
- Defective plasma cell antibody production
- Large lymphoid tissue reservoirs
- The ability of virus to evade host immune response
- Anti-retroviral drug resistance
- High mutation rate of virus
Which of the following types of cancer is LEAST likely associated with acquired immunodeficiency syndrome (AIDS)?
- Small cell lung cancer
- Lymphoma
- Kaposi's sarcoma
- Cervical carcinoma
- Epstein Barr virus associated B cell lymphoma
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |