Playlist
Show Playlist
Hide Playlist
Hemorrhagic Stroke
-
Slides 01 Stroke Neuropathology I.pdf
-
Reference List Pathology.pdf
-
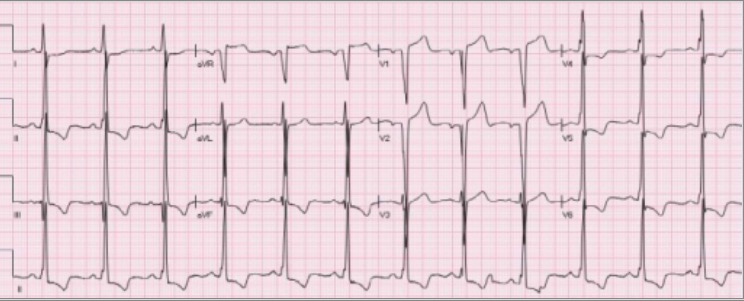
Download Lecture Overview
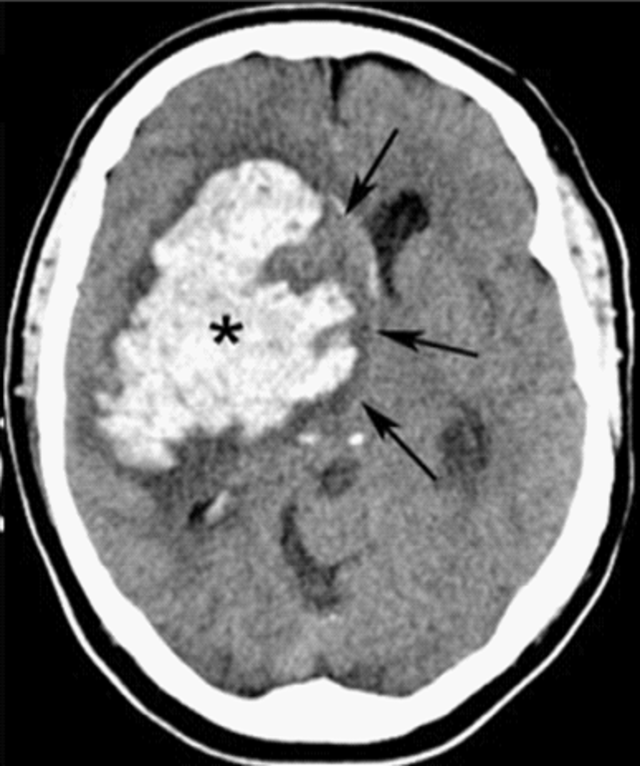
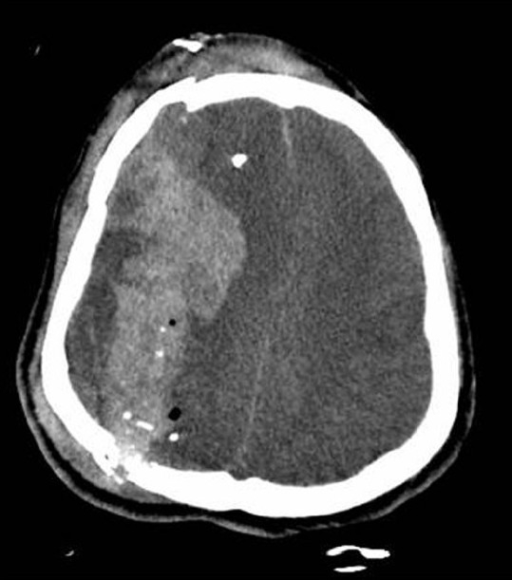
00:01 Our topic now moves in to Hemorrhagic Stroke. Under hemorrhagic stroke, intracerebral hemorrhage. Had this occur, was there hypertension? For example you refer to berry aneurysm. Whenever you hear about aneurysm, what are you worried about? With an aneurysm, you're worried about enough of expansion taking place where a rupture may take place resulting in a type of hemorrhage. Well, no exception here. And say that your patient has hypertension and you have a berry aneurysm in the anterior portion of the Circle of Willis, maybe the anterior communicating artery may result in intracerebral hemorrhage. Mass lesions, for example, metastatic lesions. You could have choriocarcinoma, extremely common in terms of where it metastasizes. So for example, you find your patient to have beta hCG to be elevated, choriocarcinoma, gestational and non-gestational choriocarcinoma. 01:00 Metastasis, unfortunately, could be up to the brain. Melanoma to the brain. Thyroid cancer to the brain. Lung to the brain. Renal carcinoma to the brain. This is a beautiful list of differentials, cancer differentials that commonly may have brain metastasis resulting in what, hemorrhagic type of stroke. Vascular malformations, amyloid angiopathy. Usually when you're ___ amyloid is ____ in the brain you should be thinking about your Alzheimer's. And some of that amyloid when this starts accumulating in your blood vessel you call this amyloid angiopathy. At risk for what? Hemorrhagic stroke. Cocaine, amphetamine use, some of these you'll find overlap with ischemic stroke as well. Remember, it's a little fine line, isn't it between an ischemic stroke and then if the blood vessel in fact does rupture it result in hemorrhagic stroke. It changes the complexion of the stroke clinically but it could actually be part of a continuum. So keep that in mind, don't be so black and white that you think "Oh it only must be this", where are you in terms of your timeline and how did it then manifest. 02:20 Maybe your patient has autosomal dominant polycystic kidney disease. What about bring that up? Because there could be that hypertension which once again may result in that berry aneurysm and if that ruptures "Oh my goodness" we call this thunderclap. Right? It is the worst headache that your patient has ever experienced and this of course should be referring to your subarachnoid hemorrhage. Trauma, anything that's causing subarachnoid hemorrhage. Now here, with hypertensive hemorrhage, so this time what we'll do is we'll take a look at blood vessel that ruptures but it was hypertension that existed prior. Once again, if there is hypertension, remember it may result in a type of ischemic type of stroke but if there is hypertension and it exists long enough, at some point in time the blood vessel may rupture. 50%-60% of the time it will be in the basal ganglia region. It could be down response, cerebellum, lobar. As you can see in the picture here, I've highlighted for you the different areas of the brain in which the hemorrhage may take place which then from your anatomy you will know as to how the patient is going to present. About 50%-60% of the time, the penetrating deep blood vessels, they are rather tiny in which an aneurysm would then rupture may result in a hemorrhagic type of stroke resulting in what kind of issues in your patient, good, contralateral motor type of issues. Right? Contralateral motor type of issue, associated with atherosclerosis and a diastolic blood pressure of greater than 110. Keep that in mind. 04:02 Remember, at the continuum, where are you in that continuum which will then categorize what kind of stroke. Hemorrhagic stroke treatment. Reverse coagulopathy. So at this point, you know your patient is bleeding. Obviously, TPA is absolutely contraindicated. Right? I laughed because that's such a silly statement and you're laughing with me because you know how silly that is. So you're going to avoid anticoagulation. You know that your PT, PTT probably is elevated. With regard to the most recent guidelines, you have to consider the following. In case of an emergency, you have to perform a baseline severity score before initiating treatment. Remember the reversal of coagulopathy. 04:46 Concerning anti-seizure medications? You have to know that patients with seizures or those with electrographic seizures must receive anti-epileptic medications. And finally, surgical management is reserved for patients with cerebellar hemorrhagic stroke who are deteriorating or who have symptoms and signs of brainstem compression. So why not try to give something that slows things down. Thus you don't have as much hemorrhage taking place in bleeding. Why not replenish some of those coagulation factors? Welcome to fresh frozen plasma huh. What plasma mean to you? It means that you're doing what, replenishing the coagulation factors so that you can address what you're looking at, the elevated PT, PTT. 05:33 Continue your management of hemorrhagic stroke. Remember we're trying to control the bleeding, platelets for thrombocytopenia. You find your platelet count less than 100 or 50,000, you start doing everything in your power to slow down bleeding and you want to now address the dam that is broken so that you stop the bleeding. Need to control that blood pressure regardless always, always, always. Maybe labetalol will be the drug of choice, non-specific. 06:00 With hemorrhagic stroke, remember some of the causes could be the list of cancers that I have given you such as your melanoma or your choriocarcinoma, renal cell lung cancers might metastasize the brain resulting in intracerebral type of hemorrhage. Well what if that was the cause of the hemorrhagic stroke? Why not identify it and see as to which you want to do next. Do you wish to then go into surgery, so on and so forth. If it's AV malformations, so here you've identified the cause of the hemorrhagic stroke by using cerebral angiography. 06:34 This is then showing you that there is an AB malformation and at that point appropriate steps in terms of surgery can then be taken. The risk factors in summarization of your hemorrhagic stroke are the following; hypertension, AB malformation, you'll notice that once again as I've told you earlier there is overlap between a hemorrhagic stroke and ischemic stroke. Most of the time it will be ischemic but there is every possibility that hemorrhagic stroke in fact would take place metastatic tumors. Preventive medicine, blood pressure control, signs and symptoms here, focal neurologic symptoms, decreased level of consciousness. Differential diagnosis once again in ischemic stroke, as I said, overlap Todd's paralysis and maybe perhaps metabolic derangement. Acute and post-acute diagnostic work-up. What are you trying to do here? Want to try to identify that hemorrhage, huh. CT or MRI to evaluate the underlying lesion, sometimes we'll repeat in 6 weeks when blood products resolve. Treatment: Blood pressure control; as we talked about earlier, reverse coagulopathy such as fresh frozen plasma, you're thinking about platelet being replenished; if your platelet count is decreased, thrombocytopenia and treating up underlying lesion.
About the Lecture
The lecture Hemorrhagic Stroke by Carlo Raj, MD is from the course Stroke (Cerebrovascular Accident). It contains the following chapters:
- Hemorrhagic Stroke
- Hemorrhagic Stroke: Summary
Included Quiz Questions
What is a possible cause of a hemorrhagic stroke?
- Metastatic lung cancer to the brain
- Smoking
- Meningitis
- Hyperlipidemia
- Diabetes
Which of the following is the most common site for a hemorrhagic type of stroke resulting from hypertension?
- Basal ganglia
- Pons
- Temporal lobe
- Thalamus
- Parietal lobe
What is the immediate management step for a patient with a hemorrhagic stroke to address coagulopathy?
- Provide fresh frozen plasma
- Administer tissue plasminogen activator (TPA)
- Give aspirin
- Increase blood pressure to ensure perfusion
- Initiate anticoagulation therapy
Customer reviews
3,3 of 5 stars
| 5 Stars |
|
3 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
2 |
| 1 Star |
|
1 |
Excellent review of topic, covers essential points and gives key factors of treatment
excellent list about the factors that increase the risk of haemorrhagic stroke. Good explanation.
Lots of facts and information missing, goals for therapy not mentioned
Not sure if there will further talks on haemorrhagic stroke but significant omissions evident. For example target for BP lowering, discussion of management of complications incl vasopasm, raised ICP, seziure prevention. Work up of patient wasn't clear ie the use of lumbar punctures in high clinical suspicions but ct equivocal
2 customer reviews without text
2 user review without text