Playlist
Show Playlist
Hide Playlist
Chronic Dyspnea and Cancer – Lung Disease
-
Slides 06 Respiratory Medicine Basics Brown.pdf
-
Download Lecture Overview
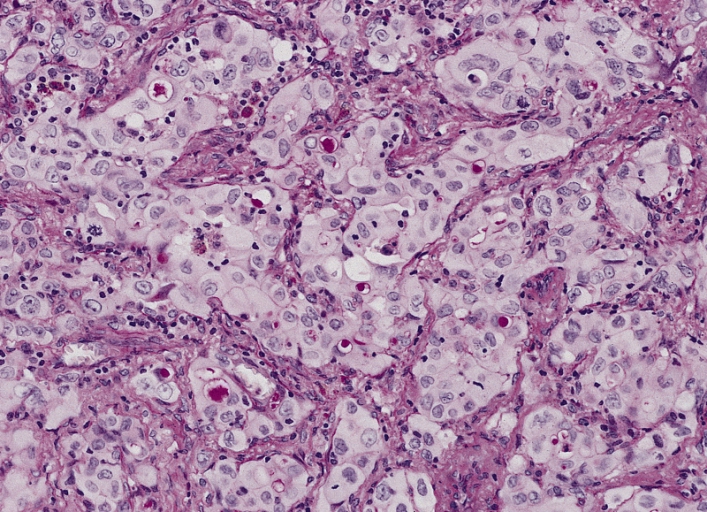
00:00 I’m just going to describe a little bit about how we might use these tests in real life. 00:05 So, for example, we have a patient who presents in outpatients with breathlessness. They’ve been breathless for a few weeks on exertion. The question is: what’s the disease that’s causing it? Well, firstly, we do a full blood count. Are they anaemic? We must make sure they’re not anaemic as that’s a good cause of dyspnoea and is easy to discount by a full blood count. If they have a lung disease causing breathlessness, then their physiology will be abnormal. So we do a spirometry, lung volumes and we do a transfer factor as well. And that will fully evaluate whether the lungs might be contributing towards their dyspnoea. 00:42 A chest x-ray is also done because, if they have any pleural interstitial lung diseases, they should have an abnormal chest x-ray. For airways diseases such as asthma and COPD, the x-ray will look fairly normal but, if they have any infiltration in the lung due to interstitial lung disease such as pulmonary fibrosis, it should be visible on a chest x-ray. 01:04 And the last thing we need to think about is: could this be a cardiac problem? And we might want to do echocardiograms, an ECG, a measurement of the brain natriuretic peptide level in the blood, all of which will identify patients who have cardiac-valve problems or cardiac failure, issues which might be making them breathless. 01:21 And when we get the results of those tests, it might dictate what we do next. 01:25 So, for example, if you have somebody with abnormal lung function and it shows an obstructive spirometry, then that suggests they could have asthma or COPD. And that might be an adequate enough investigation to identify what the problem might be. 01:37 If it’s restrictive spirometry, then you have to think about interstitial lung disease or chest-wall problems as the cause of their breathlessness. And that may require further investigation. 01:48 If they have a fall in their transfer factor, then that’s actually a very important observation because there are only really two or three major causes for that. One is emphysema but they should have obstructive lung function with that as well. Two is interstitial lung disease. And the third would be pulmonary emboli or pulmonary hypertension. So pulmonary vascular disease of some description. 02:09 If the x-ray is abnormal, then you really need to get more information about what that abnormality might be due to. If it’s breathlessness that’s the problem, then we’re thinking about pleural disease which will require an ultrasound or a CT scan to assess in more detail. If it shows interstitial lung disease, then a CT scan is absolutely necessary to identify what’s going on in more detail. 02:28 So this will lead onto our next set of investigations, obstructive spirometry: is it reversible or irreversible obstruction? And that will dictate whether the patient has asthma or COPD to a certain extent. If it’s restrictive spirometry, you need a CT scan to assess the lung parenchyma in more detail. The same if you suspect potential interstitial lung disease because of the chest x-ray changes. And if there’s a low transfer factor, you do need that CT scan to look for interstitial lung disease but also you might need to think about the pulmonary vessels and do a CT pulmonary angiogram to assess those in more detail and potentially do an echocardiogram to make sure they don’t have pulmonary hypertension. 03:05 Now, that’s somebody presenting with dyspnoea – shortness of breath – in outpatients. 03:11 If you have somebody who’s got lung cancer, it’s actually a very different scenario and a very different set of tests become important. 03:17 So somebody presents: mass on the chest x-ray, they’ve coughed a bit of blood or something along those lines, they make you suspect they may have lung cancer. Actually they’ve had their chest x-ray. The next test is – there’s a mass, we need to define that in more detail. 03:32 Let’s do a CT scan to get a three-dimensional vision of that mass to see exactly where it is in the lung, what tissues it might adjoining to. And in addition, we may want to stage the patient to see whether they have liver or adrenal involvement, metastases perhaps from that original lung cancer. 03:52 We do some blood tests. And the reason why we do those is that, again, that actually helps identify patients who may have metastases because the alkaline phosphatase will be raised with bone metastases and with liver metastases. And we need to know about calcium, U&Es because there are complications of cancer that might affect those electrolytes. 04:09 And then actually the most important test will be a biopsy. So once you’ve done the CT scan, the next question is: which biopsy modality you will use? That would be dictated by the anatomy that you have defined using the CT scan. And you’ll do a biopsy and get the histological results and that will then dictate the treatment. And further tests might be required to see whether that treatment is suitable. 04:35 So, for example, if somebody has got a lung mass, it turns out to be a cancer, it turns out to be a localised cancer but they have background COPD making them short of breath on exertion. We may want to resect that cancer but the worry here is that that’ll make them more breathless because, to resect the cancer, we’re going to have to remove a large amount of lung. So you measure their lung function and get a feel for whether they could cope with that lung resection without ending up in respiratory failure. 05:01 And so on. We might do tests regarding kidney function to make sure they can cope with the chemotherapy. 05:08 So to summarise this lecture: Diagnostic tests have to be used in a targeted way to answer specific clinical questions when you’re assessing the patient. And the interpretation of those tests has to take into account the clinical context because the interpretation will be inaccurate without doing that. 05:24 Most patients presenting with suspected lung disease can be actually fully assessed using simple lung-function tests such as a peak flow, spirometry and a chest x-ray. 05:33 Lung function is actually vital for monitoring chronic lung disease. So those patients who have chronic lung impairment need monitoring over time to see whether that impairment is staying stable or deteriorating. And that’s the role of lung-function testing. Mainly spirometry but not just spirometry, occasionally transfer factor as well. 05:57 More complex diseases do require more complex investigations with more detailed lung-function testing – such as the transfer factor and the lung volumes and, potentially a CT scan. 06:07 For some lung diseases – mainly lung cancer – obtaining histology is vital and essential to actually confirm the disease and to guide therapy. And nowadays we have a multitude of different methods for obtaining histology from suspected lung cancer patients which allows us to do this in the vast majority of patients safely and quickly. 06:27 And thank you for listening.
About the Lecture
The lecture Chronic Dyspnea and Cancer – Lung Disease by Jeremy Brown, PhD, MRCP(UK), MBBS is from the course Introduction to the Respiratory System.
Included Quiz Questions
Which of the following is not an advantage of chest CT scans over chest x-rays?
- The patient lies down for a CT scan and stands up for a chest x-ray.
- They provide better definition of mediastinal anatomy.
- They can identify pulmonary emboli.
- They provide better definition of pulmonary parenchyma.
A 20-year-old patient comes into the ER complaining of shortness of breath. During the physical examination, you only notice pale skin and mucosae. Which of the following labs would you request first?
- CBC
- Bone marrow biopsy
- Chest x-ray
- Chest CT scan
- ECG
Which one of the following conditions may display a fairly normal chest x-ray?
- Asthma
- Sarcoidosis
- Cystic fibrosis
- Tuberculosis
- Pneumonia
Regarding pulmonary functions tests, which one of the following diseases will display an obstructive pattern?
- Emphysema
- Pneumonia
- Tuberculosis
- Sarcoidosis
- Cystic fibrosis
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |