Playlist
Show Playlist
Hide Playlist
Benign Breast Diseases
-
Slides BenignBreastDiseases Surgery.pdf
-
Download Lecture Overview
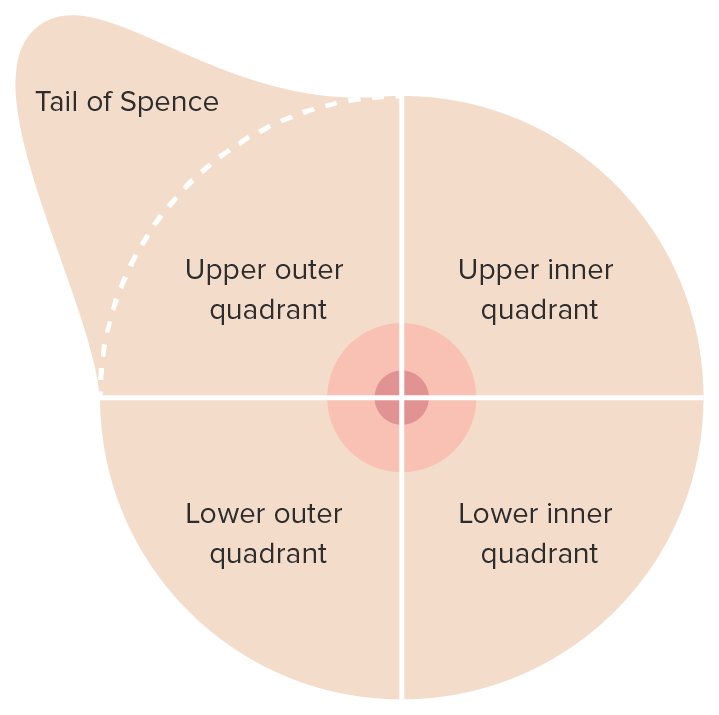
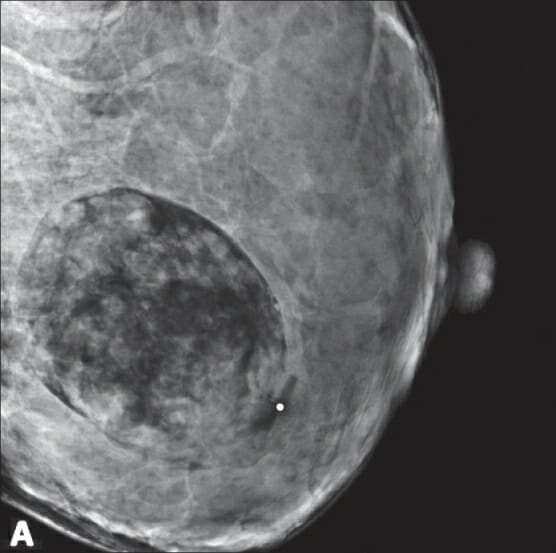
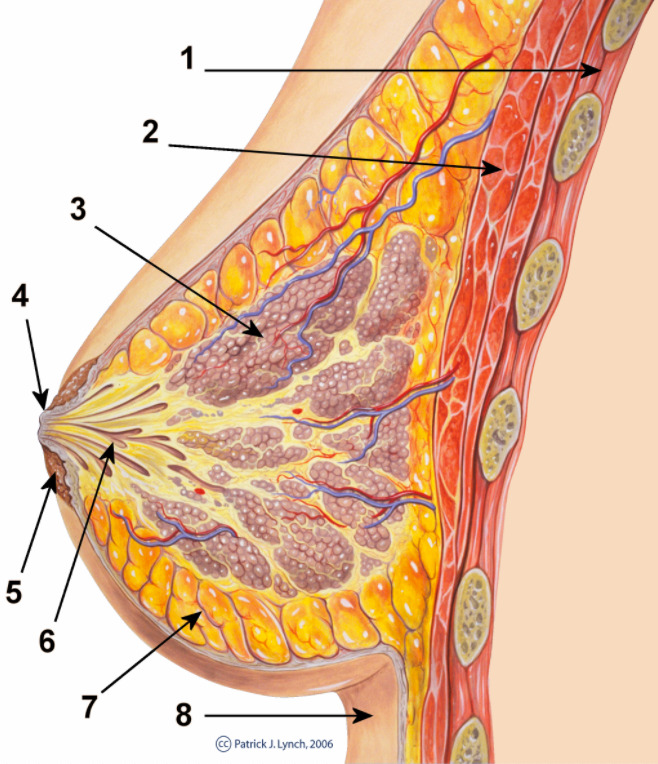
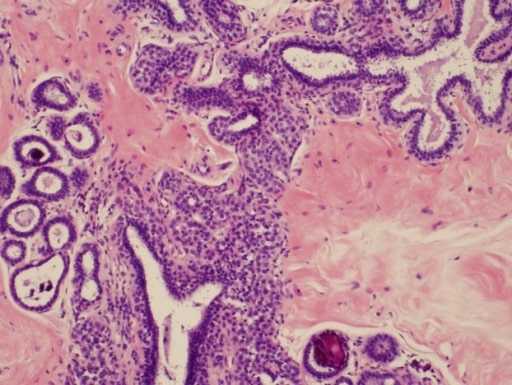
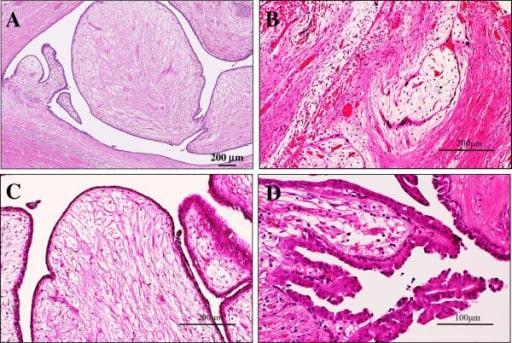
00:01 Welcome back. Thanks for joining me on this discussion of benign breast diseases in the section of general surgery. Let´s start with the question, when should women start screening for breast cancer? I´ll give you a second to think about this. Well, according to the United States Preventative Services Task Force which is the authority on such measures, women, 40 years of age to 74 years of age of average risk based on recommendation should start a mammogram every two years. 00:32 It´s controversial what patients between the ages of 40 and 49 should do. That decision is left up to a discussion between the doctor and the patient. Breast masses are usually thought of as either benign or malignant. In this lecture module, we´ll focus on the breast masses that are benign. 00:56 In benign breast masses, the vast majority of patients in fact have fibrocystic change. 01:02 Fibrocystic change may be cyclical changes associated with one´s menstrual periods. We´ll discuss fibroadenoma in a little bit more detail. The most important decision regarding breast masses is to define whether or not this mass is benign or malignant. 01:22 Benign Breast Dieases Benign breast lesions can be divided in three categories: non-proliferative, proliferative without atypia and proliferative with atypia. 01:34 Non-proliferative lesions are not associated with an increased risk for breast cancer. 01:40 These include: breast cysts, papillary apocrine changes, epithelial-related calcifications, mild hyperplasia of the usual type and apocrine metaplasia. 01:54 Proliferative lesions without atypia are associated with 1.5 to 2 times increased risk for breast cancer. 02:02 This category includes sclerosing adenosis, ductal hyperplasia, intraductal papillomas, radial scars and fibroadenomas. 02:12 Although fibroadenomas have been historically classified in the category of non-proliferative lesions, they are now considered proliferative lesions. 02:21 They are associated with a slightly increased risk for breast cancer in the case of complex fibroadenoma pathology, breast cancer history in the family or adjacent proliferative changes. 02:33 In the absence of these features the majority of women with fibroadenomas do not have an increased risk for breast cancer. 02:40 Proliferative lesions with atypia are associated with 4 to 5 times increased risk for breast cancer. 02:47 This category includes atypical ductal or lobar hyperplasia. 02:55 This is my general approach to patients with breast diseases. 02:58 We want to start by obtaining a careful history. 03:01 More than any other disease process, a careful history is very important in patients with breast disease particularly in patients with family history of breast cancer. Next, we perform a thorough examination, both of the breast itself as well as the lymph node draining basins. 03:18 We then obtain age-appropriate diagnostic imaging. What do I mean by that? Young patients may have very dense breast tissue and may be more amenable to ultrasound imaging as opposed to age-appropriate patients undergoing mammograms. 03:34 Regardless, one wants to get an image prior to disturbing the anatomy with biopsies. 03:39 Speaking of, we usually get tissue biopsies to help us guide the next step of management. 03:45 When we put all this information together, we can counsel the patient on the most optimal treatment plan. 03:52 This is very important. Next steps in management are usually determined on whether or not the mass is palpable or nonpalpable. 04:01 You can imagine for a palpable lesion, biopsy is easy. 04:06 But for a nonpalpable lesion, how do we pursue biopsy? Well, that usually involves image guidance. 04:12 Physical examination of the breast is very important. Not only do we want to do a thorough bilateral examination with the patient completely undressed, we also want to focus on the draining lymph nodes. 04:23 These are lymph nodes both in the supraclavicular region as well as in the armpit and behind the pectoralis muscles. If you were to get routine laboratories, they are unlikely to be helpful whether it´s chemistry or CBC. 04:39 Particularly in young patients where the breast tissue may be too dense for mammograms to be useful, ultrasound is a primary modality. Here in this ultrasound, you see an anechoic lesion just below the surface of the probe. 04:58 Remember, fluid-filled or anechoic masses on ultrasound appear dark. 05:04 Here is a typical mammogram. This is a normal mammogram. Mammograms are usually obtained in two different views. 05:14 Lets focus on fibroadenomas. Fibroadenomas are usually found in young women. 05:21 The exact etiology is unknown. They may respond to hormones. 05:27 Here is an ultrasound image of a large fibroadenoma. Biopsy is usually not necessary for fibroadenomas. 05:40 Lets talk about specific biopsy options. When it´s a palpable lesion, one can actually perform the biopsy right in the office. This is called the core needle biopsy. 05:50 If you have an ultrasound in the office, you can perform this under ultrasound guidance. 05:55 If pathology demonstrates a fibroadenoma, no excision is needed. Remember, large excisional biopsies can result in poor cosmetic outcome. Just to remind you, excisional biopsy means that you´re removing the entire mass both at the same time as biopsy and potentially as the final therapy. 06:17 What about giant fibroadenomas? These are described as lesions that are greater than 10 cm. 06:26 We recommend excision in these situations because it is often difficult to distinguish from phyllodes tumors which may be precancerous.
About the Lecture
The lecture Benign Breast Diseases by Kevin Pei, MD is from the course General Surgery.
Included Quiz Questions
Which of the following age groups are recommended by US preventive services task force to undergo mammography every 2 years as a screening for breast cancer?
- 40 to 74-year-olds of average risk
- 30 to 74-year-olds of average risk
- 45 to 75-year-olds of average risk
- 55-year-olds and older regardless of risk
- 50 to 80-year-olds of high risk
Which of the following breast masses confer an increased risk of developing breast cancer?
- Atypical ductal hyperplasia
- Breast cysts
- Fibrocystic changes
- Nonproliferative tumors
- All benign tumors confer an increased risk of malignancy
A 29-year-old woman with no past medical history presents with a lump on her left breast that she has noticed in the past 3 months. On exam, the mass is firm, smooth, non-tender, and feels to be about 3 cm in diameter. What is the next best step in management?
- Obtain a breast ultrasound
- Obtain a mammogram
- Core needle biopsy of the lesion
- Full mass excision
- Stereotactic biopsy of the lesion
When is excision of a fibroadenoma recommended?
- If it measures greater than 10cm.
- Never - fibroadenomas are nonproliferative benign masses
- If the woman has a first degree relative with breast cancer.
- If the woman is less than 35 years old.
- If the woman has two or more distinct fibroadenomatous masses.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |