Playlist
Show Playlist
Hide Playlist
Bacterial Meningitis: Diagnosis & CSF Findings
-
Slides Meningitis InfectiousDiseases.pdf
-
Reference List Infectious Diseases.pdf
-
Download Lecture Overview
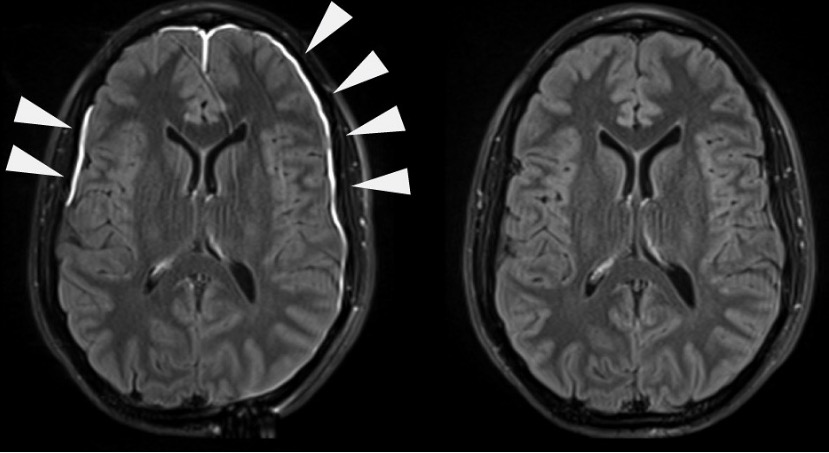
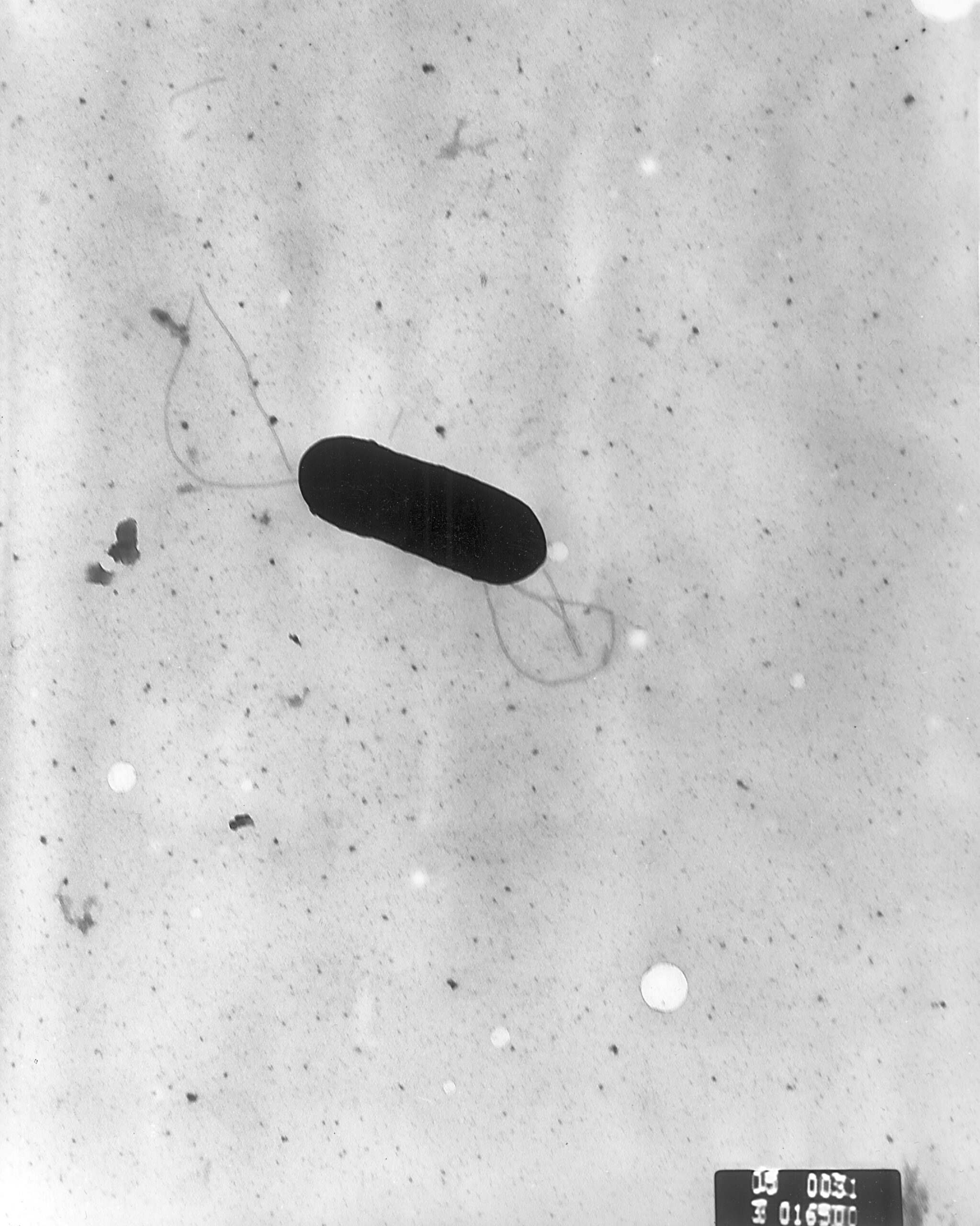
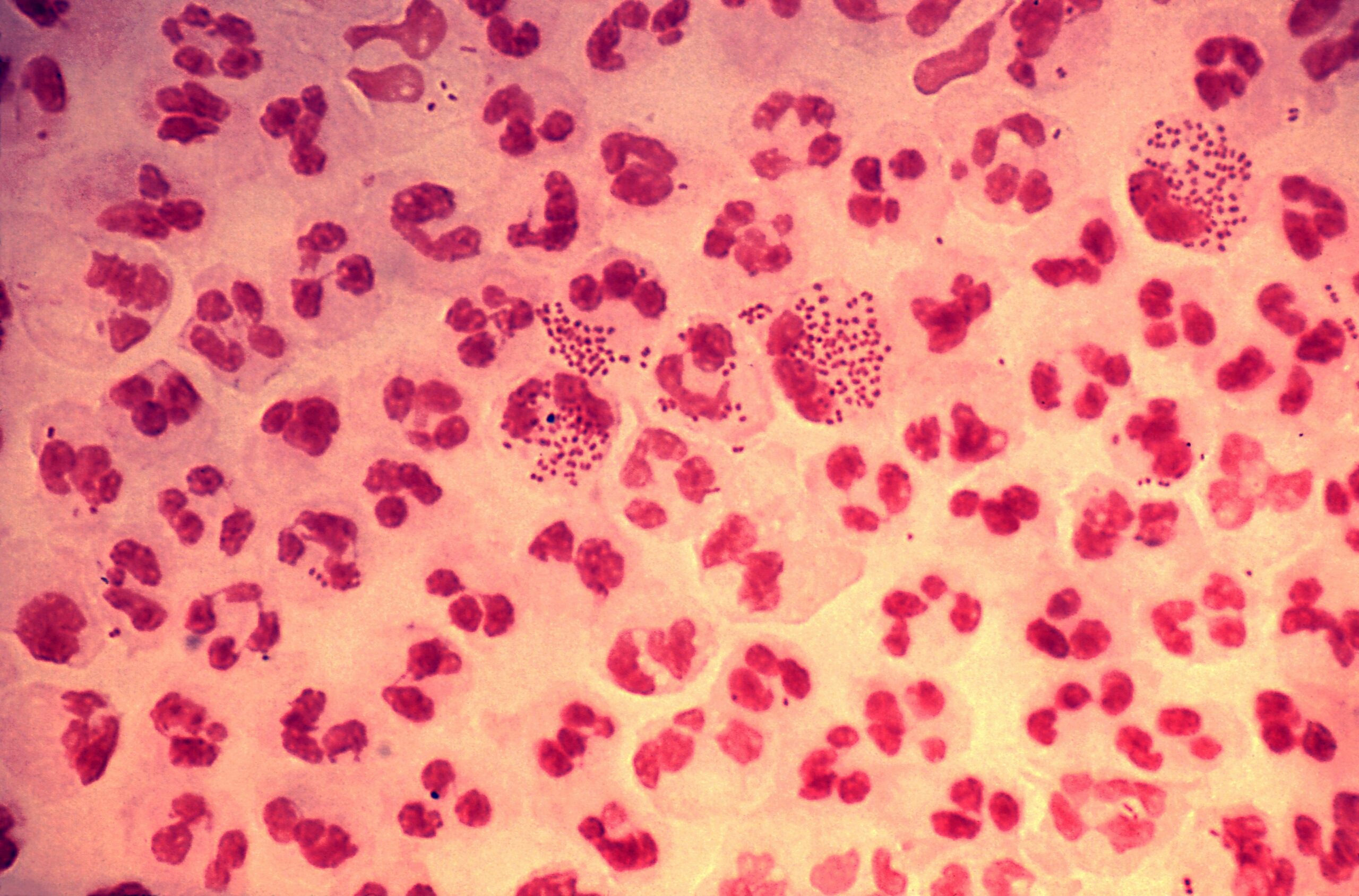
00:02 It's essential to get some spinal fluid in a patient who has meningitis. 00:10 And when you get some spinal fluid, during the lumbar puncture, you will note that the opening pressure is elevated. 00:20 When you microscopically examine the spinal fluid, you will find that there are too many white cells. 00:28 Now, normally, there should be no more than five white cells in spinal fluid and they should be all mononuclear, lymphocyte or round cells. 00:42 So, it's abnormal if a spinal tap shows even one white cell that’s a neutrophil. 00:49 So, neutrophils are abnormal in spinal fluid. 00:53 There are some exceptions. 00:55 Because of the pace of meningococcal meningitis, the patient may not have had time to develop much in the way of white cells. 01:04 This little girl that I told you about had just one or two neutrophils in her spinal fluid. 01:12 And in infants under four weeks of age, they may not have white cells in the spinal fluid of that magnitude. 01:23 Now, if they have white cells, there is a neutrophil predominance, more than 80% are neutrophils. 01:31 Once again, the exceptions to that would be a newborn where they had the cause being something like E. coli They may not have a neutrophil predominance. 01:43 And also with Listeria. 01:45 Now, if you remember the name of Listeria is Listeria monocytogenes. 01:51 And that implies that the organism can cause meningitis with mononuclear cells in the spinal fluid. 02:01 So, that's where it got that name. 02:02 Here is a last example: in tuberculous meningitis, you also find lymphocytosis rather than neutrophil predominance. 02:09 Now, obviously, when you get some spinal fluid, you’re going to culture it and you'll get a positive culture in about 80% of individuals unless they’ve been given antibiotics. 02:25 And think how many patients go to the physician and get empirical antibiotics for fever. 02:32 I wonder what's up with that. 02:35 But that may obscure the diagnosis of bacterial meningitis and the cultures may be negated or reduced to 60% or 70% positive if antibiotics had been given. 02:52 It's also important to measure the spinal fluid glucose. 02:58 You'll find that the spinal fluid glucose is lower than it’s supposed to be. 03:02 It'll be usually less than 40 mg/dL in at least 60% of individuals. 03:10 And if you compare the spinal fluid glucose to the serum glucose, it's less than 31% of the corresponding serum glucose. 03:23 And oftentimes, it's less than 18 mg/dL. 03:27 It's usually very low. 03:29 And if it's that low, it's going to be highly predictive of bacterial meningitis. 03:35 The protein is usually elevated, sometimes quite elevated to 500 mg/dL And a Gram stain of spinal fluid is essential. 03:48 And you'll find that it's positive. 03:50 It'll predict what you need to treat with in 60% to 90% of patients. 03:57 You can choose antibiotics on the basis of the Gram stain findings. 04:01 We also can test for bacterial antigens. 04:06 And the best use of it is when somebody's been given prior antibiotics. 04:11 The bacterial antigens may still be around, even though the bugs have been partially killed. 04:18 And so, it's used when the Gram stain is negative. 04:22 Unfortunately, it's not particularly helpful to do bacterial antigens in urine or serum in patients with bacterial meningitis. 04:33 Now if we compare these findings to viral meningities, in the later you would find normal glucose levels, not so high protein levels and lymphocytic predominence. 04:42 Now, I did mention that spinal fluid should be examined in everybody who's got a suspicion of meningitis, but there are certain physical findings that may have - make you delay doing a lumbar puncture because if the patient has evidence of increased intracranial pressure, you may kill them with a lumbar puncture. 05:07 Because if they have markedly elevated intracranial pressure, if you do a lumbar puncture and relieve some of that pressure below, they may actually herniate, and so the herniation can kill them. 05:23 So, what you need to do is, if you think there is clinical evidence of an increased intracranial pressure, you need to verify that with imaging. 05:34 And so, you have to delay therefore your examination of spinal fluid. 05:40 Where you find Gram-positive diplococci along with a lot of neutrophils? Is it Haemophilus influenzae, a very pleomorphic Gram-negative coccobacillus? Or is it that classic Neisseria meningitidis? Or is it Listeria monocytogenes, which are small Gram-positive rods? And the value of the Gram stain is that it suggests an etiology before your cultures come back. 06:12 The cultures may not come back for up to 72 hours, though time to positive blood and CSF cultures can be as quick as 24 hours. 06:19 So, if you've got an idea of what to treat with the Gram stain, you can design your antibiotic regimen. 06:26 Unfortunately, the Gram stain is less useful if the patient has received antibiotics and it may be negative. 06:35 One thing it doesn't change is the spinal fluid formula. 06:40 The protein still up, the white count is still up, the glucose is still low. 06:46 That doesn't usually change with antibiotics. 06:49 Blood cultures are positive in a large number of patients. 06:57 But as you could imagine, the blood cultures are often negative if antibiotics have been given. 07:03 So, blood cultures are useful when a spinal tap is contraindicated. 07:11 So, you have evidence that the patient has increased intracranial pressure. 07:15 You’ve got to get cultures from somewhere, and so getting them from the blood. 07:19 If you get an organism, you know what to treat. 07:22 There are some rapid tests that we can do on spinal fluid. 07:27 The one that was in vogue when I was training was the latex agglutination. 07:34 This is no longer used because of the number of false positives. 07:38 We now use immunochromatographic tests, which are rapid, they can be done in less than two minutes and give you an idea of what to treat. 07:50 For example, in a study showing 450 specimens of cerebral spinal fluid, 122 of them had Streptococcus pneumoniae in them. 08:04 And they were identified by culture in 87 individuals and 35 were identified by PCR. 08:16 But the bottom line was that all the patients that had Streptococcus pneumoniae were positive, so this immunochromatographic test had a sensitivity in this study of 100%. 08:29 It’s probably not quite that good, but it's pretty good. 08:33 And we can also do PCR, targeting the 16S ribosomal RNA gene, which is highly conserved among bacteria. 08:43 So, you can demonstrate that the patient has a bacterial meningitis with PCR. 08:49 It's a little more labor-intensive and it’s not available immediately. 08:54 But in a study of 206 CSF specimens tested, 17 pathogens were identified by either culture or PCR and three of them were culture negative, but PCR positive. 09:10 So, it's showing great promise. 09:12 So, the rapid tests ultimately have a sensitivity of about 100% and a specificity of more than 95%, but we still need more studies dealing with these rapid tests.
About the Lecture
The lecture Bacterial Meningitis: Diagnosis & CSF Findings by John Fisher, MD is from the course CNS Infection—Infectious Diseases. It contains the following chapters:
- Diagnosis – CSF Findings
- CSF Gram’s Stain
- CSF Rapid Tests
Included Quiz Questions
An 8-day-old boy is brought to a pediatrician for poor feeding over the past 24 hours, nausea, and vomiting. He is lethargic. On physical examination, his temperature is 38°C, respirations are 40/min and unlabored, the pulse is 120/min, and blood pressure is 75/50 mm Hg. Serum analysis reveals leukocytosis with a left shift. Blood chemistry and urinalysis are normal. Blood cultures are drawn. What is the most important next diagnostic step?
- Lumbar puncture
- Brain MRI
- Arterial blood gases
- Chest x-ray
Gram stain of cerebrospinal fluid from a 2-year-old child with clinical signs of meningitis shows gram-positive dipplococci with many neutrophils. What is the most likely pathogen?
- Streptococcus pneumonia
- Listeria monocytogenes
- Haemophilus influenzae
- Neisseria meningitidis
- Staphylococcus aureus
Cerebrospinal fluid analysis of a sick newborn who is 2 weeks old shows decreased glucose, increased proteins, and about >10 mononuclear lymphocytes, but no neutrophils. Which of the following bacterial etiologies is most likely?
- Listeria monocytogenes
- Streptococcus agalactiae
- Haemophilus influenzae
- Neisseria meningitidis
- Streptococcus pneumonia
Which of the following abnormalities is typically expected on cerebrospinal fluid analysis of a patient with bacterial meningitis?
- Decreased glucose concentration
- Increased spinal fluid glucose to serum glucose ratio
- Decreased protein concentration
- Increased mononuclear lymphocytes
- Decreased opening pressure
Which of the following is an absolute contraindication to performing a lumbar puncture?
- Clinical signs of increased intracranial pressure
- Fever greater than 103 degrees F
- History of prior lumbar discectomy
- Receipt of prior antibiotics
- Hypotension
Cerebrospinal fluid analysis shows increased white blood cells with neutrophillic predominance, decreased glucose concentration, increased protein concentration, negative Gram stain, and positive bacterial antigens. Which of the following is the most appropriate interpretation?
- Patient has been given antibiotics prior to lumbar puncture.
- Patient has a poor immune response.
- Patient does not have meningitis.
- Patient has viral meningitis.
- Not enough spinal fluid was collected for analysis.
Customer reviews
4,7 of 5 stars
| 5 Stars |
|
2 |
| 4 Stars |
|
1 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Good video .Well made. It'll help for my exam. Well done Lecturer!
it's a well prepared material and professional doctor thank you sir
First of all, love the option to choose the speed of the video clip. Secondly, it was smartly taught, no matter which type you are, from visual to auditory-learner, you are going to understand and learn it easily. I also loved Dr. Fisher's (the lecturer) teaching style, brief description for medical terms, mentioning important DDx, plus his tone and not having specific accent.