Playlist
Show Playlist
Hide Playlist
Asthma: Treatment
-
Slides ObstructiveLungDisease Asthma RespiratoryPathology.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
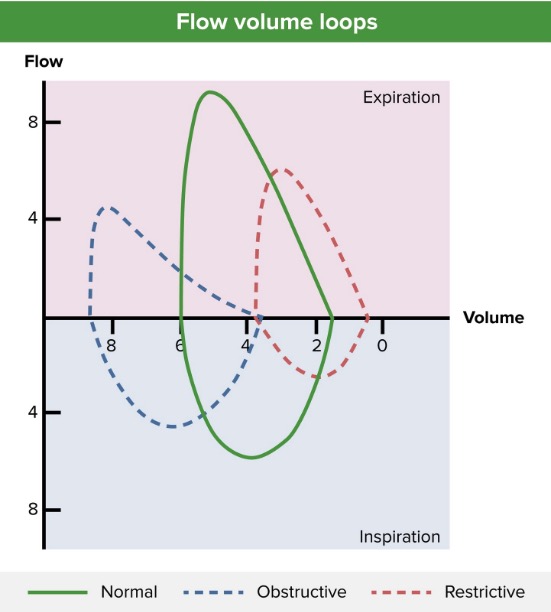
00:01 Now, the asthma treatment therapy. 00:03 We'll go from what's known as relatively mild to severe. 00:07 First and foremost you always take history and with the history you're looking for, what's the most common type of asthma? Extrinsic. 00:14 Go step by step. Exposure to the external world and that's called atopy, right? Atopy. 00:20 So, maybe your patient needs to then remove himself or herself from that environment. 00:25 That's your first step of management if that's the case. 00:29 Next, short-acting bronchodilator. 00:32 So what does that do? Albuterol as needed, puff-puff-puff-puff, whenever they're having an attack or bronchospasm. 00:41 And so therefore, relieves that obstruction. 00:45 Next, what about inhaled steroids? ICS, corticosteroids low to mid. 00:52 Remember, inhaled corticosteroids is it going to do what? It's going to then help you with some of that bronchoconstriction perhaps, and whenever you deal with your corticosteroids, you tell me what enzyme is it knocking out? Is it LOX? Is it COX? Or is it phospholipase A2? Good, it's phospholipase A2. 01:17 You've knocked out the leukotriene and prostaglandin pathway, haven't you? And by knocking out some of that leukotriene pathways especially C4,D4,E4, then you may then avoid bronchoconstriction. 01:32 Are you clear about that pharmacology? Management is important. 01:35 The 2020 GINA Guidelines recommend inhaled corticosteroid, as the preferred reliever for patients who present with symptoms less than twice a month and for the prevention of exacerbations. 01:46 Short acting beta-2 agonist can be used in addition if needed. 01:51 Let's continue. Long-acting beta agonist, leukotriene modifier. 01:56 Give me some. Well, what if you knock out the LOX? Zileuton. 02:02 What if you knock out the receptors for leukotrienes? -kast. 02:07 Montelukast, Zafirlukast, things you've looked at, is that clear? Which leukotrienes are you trying to avoid in asthma, in bronchospasms? C4,D4,E4. 02:17 About theophylline. Theophylline will help you, well this goes back to biochemistry, you should be liking this. 02:24 This beta-2 that's a receptor on the bronchial smooth muscle, what does it work through? What second messenger from biochemistry? Good, GS. What's GS mean to you? A-A-A-A-A, what does that? What do I mean A-A-A? Well, that's your adenylyl cyclase, that's your ATP to cyclic AMP. 02:43 That means protein kinase A. What does that mean? I am knocking out my myosin light-chain kinase because I phosphorylated. 02:53 Remember all this? If you don't, then this would be a good time to go back and take a look at your biochemistry with smooth muscle mechanics. 03:00 So, if you knock out the myosin light-chain kinase, guess what happens to the bronchi? Relaxation. 03:08 So, what do you think theophylline might do? Theophylline, well how do cyclic AMP break down? Phosphodiesterase. 03:14 What if you inhibit some of that phosphodiesterase? Voila! You knock out the phosphodiestrase, your cyclic can't be forevermore. 03:22 Isn't that what you want with beta-2? Yes you do. 03:26 Now, I'll tell you right now the two major approaches for smooth muscle relaxation especially for the bronchi. 03:32 Either beta-2, you look for that mechanism in pharmacology and biochem and you take a look at NO, okay? Nitric oxide, please. 03:41 Those are two that you want to pay attention to. 03:43 Let's continue. You have anti-IgE therapy. 03:45 Alright, so with IgE therapy you're thinking about, well some of those drugs that inhibit, what? Your breakdown of your mast cell. 03:55 So anything that then inhibits the degranulation of your mast cell is always important. 04:01 Hence, you're looking at things like this, anti-IgE therapy. 04:04 Alright now in terms of severity, we're just going to move from top to bottom which is just the severity in the beginning will be quite minimal and then as you go through your severity and it gets worse then obviously as far as management, things become a little bit more complicated. 04:22 Prevention in all. So how do you educate your patient? Important. 04:26 If you can avoid giving medication to your patient that is your answer. 04:30 So therefore, educate your patient. "Oh, hey doc, my child is having coughs, episodically." "Oh, okay, and?" "Well, I can hear kind of wheezes and such." "Okay" "And he goes and plays - he plays in this particular park and every time he comes back after he plays, oh, he doesn't seem so well." Okay, so, you want to try to figure out as to what was the child exposed to in that park that makes him feel like this? Prevention, prevention, prevention. 05:00 Now, after this, mild-intermittent, mild-persistent, moderate persistent and severe. 05:06 Remember we start getting to severe and such and even at night if there's coughs, not a good sign, you need to make sure that you're intervened ASAP. 05:15 Let's talk about that acute flare, so during the acute flare in your head, you should be thinking about, is that loop spirometry which we saw a scalloped portion. 05:25 Here, when you have an acute flare what are you trying to do? Immediately try to bronchodilate. Nebulizer. 05:33 So, what does that mean? That means that you have a gas mask. I call it as such. 05:37 Which is then attached to a machine which is then exerting or expressing what? Albuterol. 05:43 Ipratropium, keep in mind, there are two ways you can approach this, right? Either you could stimulate the beta-2 receptors. 05:51 I just walked you through that in great detail, or you could block your parasympathetic. 05:57 Two methods, Albuterol much more so. 06:00 What else? Oral or IV steroids? IV steroids. What's my problem? Acute flare. 06:06 Oxygen if hypoxia is present. Acute flare, well, the magnesium just keep that in mind. 06:12 Magnesium is a big deal for your medicine though, okay? Remember with magnesium two major things, number one, seizures, if it's hypomagnesemia, also if it's hypomagnesemia, you're thinking about long QT syndrome. 06:26 So those are major things you want to think about when dealing with magnesium. 06:30 Close monitoring, make sure chronic treatment are being used correctly. 06:34 By chronic we're talking about, well, is the patient on the right bronchodilator? Is it a beta-2 agonist? Is it a leukotriene inhibitor of the right type or maybe it's even a type of corticosteroids. So those are things you want to keep in mind. 06:50 Now, what I wish to bring to your attention that you will be asked, is if there is such an acute flare especially when you have a child that has an asthma attack, not only is this child breathing really quick and the diaphragm obviously is being used but then the accessory muscles are breathing are also being used, do you remember this conversation? So, look for this and don't forget. 07:12 If you find a patient come in and they're breathing, the sternocleidomastoid is working and the intercostal muscles are working, this is a child who, at some point, those muscles are going to fatigue and tire. 07:24 And the child starts quieting down and maybe it's an intern who didn't know any better and feels as though that he or she has treated the child and the child is quieting down, thinks that he or she is managing the child properly. But why is the child quieting down? The muscles are getting tired, the child's not breathing anymore. 07:47 Wow. What's your next step of management? Intubate. 07:51 Break a few teeth rather than have your child die on the table. Is that clear? That is a big deal. 07:57 So, what are you going to measure? You tell me, use common sense. 08:00 What are you going to measure in the blood? This will tell you that the child's acute flare is actually getting worse? The pH, of course. 08:10 Because if the child's muscles are tiring and the child's not breathing, what's the child retaining? Carbon dioxide, good. What will happen to your pH? Decreased. 08:19 Welcome to respiratory acidosis and that is no joke.
About the Lecture
The lecture Asthma: Treatment by Carlo Raj, MD is from the course Obstructive Lung Disease.
Included Quiz Questions
Which of the following is the initial drug of choice in the management of a patient with asthma who presents with symptoms less than twice a month?
- Inhaled corticosteroid
- Nebulized anticholinergics
- Oral albuterol
- IV salmeterol
- IV steroids
Which of the following is NOT used in the treatment of MODERATE PERSISTENT asthma?
- IgE therapy
- Leukotriene modifier
- Theophylline
- High dose ICS
- Long-acting beta agonist
What is the most common type of asthma?
- Extrinsic asthma
- Intrinsic asthma
- Exercise-induced asthma
- Anaphylactic asthma
- Obesity-associated asthma
Which of the following is the most effective initial step in the management of asthma?
- Avoid triggers
- IgE therapy
- Oral steroids
- Long-acting bronchodilator
- Inhaled steroids
Which of the following causes bronchodilation by inhibiting phosphodiesterase, leading to an increase in cyclic AMP (cAMP) within cells?
- Theophylline
- Albuterol
- Fluticasone
- Montelukast
- Ipratropium bromide
Which of the following enzymes is blocked when corticosteroids are administered in a patient with asthma?
- Phospholipase A2
- Phospholipase C
- Phospholipase B
- Phospholipase A1
- Phospholipase D
Which of the following is used to inhibit the degranulation of mast cells?
- IgE therapy
- IgA therapy
- IgD therapy
- IgM therapy
- IgG therapy
What is the primary function of leukotriene modifiers in the treatment of asthma?
- Block the action of leukotrienes to reduce bronchoconstriction.
- Stimulate the production of leukotrienes to enhance immune response.
- Inhibit the action of beta-2 agonists in the bronchial smooth muscle.
- Activate phosphodiesterase to decrease cyclic AMP levels.
- Increase the breakdown of mast cells to release histamines.
Customer reviews
3,7 of 5 stars
| 5 Stars |
|
4 |
| 4 Stars |
|
1 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
2 |
You are the best teacher in the world ,thanks for exist
This professor does not explain. I've been trying to dissect all his asthma lectures and it's very hard. it's very incoherent; he jumps concepts and doesn't finish explaining them.
I know his teaching style does not suit some people, but I find that he makes references to a lot of previous learning which keeps it fresh and relevant in my mind! Thank you v. much Dr Raj
You guys have to read the articles and study some things before getting to Dr Carlos videos. He is very fast and dont explain certain terms because you have to know this stuff before watching the video.
1 user review without text