Playlist
Show Playlist
Hide Playlist
Asthma: Diagnosis
-
Slides ObstructiveLungDisease Asthma RespiratoryPathology.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
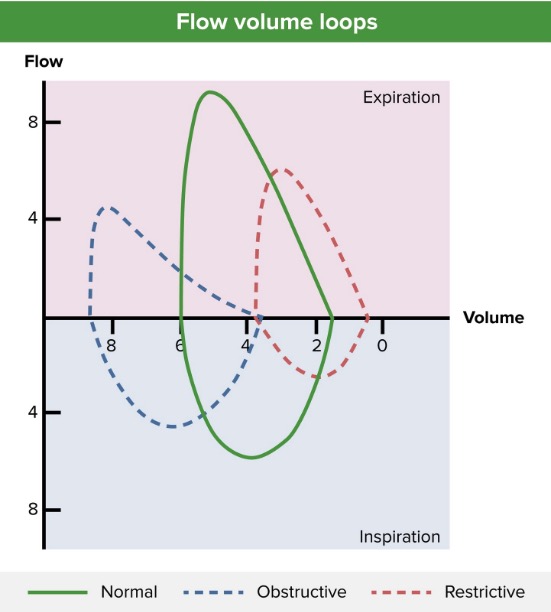
00:01 Diagnosis, history of course being the predominant theme. Is your patient exposed to whatever that we just walked through and we’re looking for wheezing that’s episodic and coughing. That’s the hallmark. Now, if you find this to be at night we talked about how that the patient that is untreated and that’s rather dangerous because you're always worried about this immediate type of reaction called status asthmaticus. Chest x-ray typically normal but could show hyperinflation but especially during a flare. 00:30 Obstructive by that we mean that you’re having a hard time getting your air out. Once again what I wish that we mean that you’re having a hard time getting your air out. Once again what I wish to show you at a later on discussion is the current day practice of asthma, chronic bronchitis and emphysema all sharing similar symptoms ultimately with your patient but keep in mind that it is an obstructive type of issue. Now, your pulmonary function test because we’re talking about this being obstructive, you can predict as to what you can find with laboratory. 00:57 Your FEV1/FVC ratio by definition has to be decreased, right? Okay, so if this obstructive you tell me as to what the TLC should be. An increase in TLC, an increase in residual volume. I’ll tell you when we have transitioned into restrictive lung disease topics. The reason I bring that up is, now as you move through this, I want you to compare and contrast always. In restrictive you’ll have a decrease in total lung capacity and you have a decrease in residual volume and FEV1/FVC ratio will never be decreased in restrictive. Now the obstructive pattern usually reverses after? Now you keep this in mind, very important for you to pay attention. The bronchodilator here, often times this type of obstructive disease is reversible. So, what was that receptor again that brings about bronchodilation? Good, Beta2 receptors. After doing this the pulmonary function test may be normal when the patient is not experiencing such a flare. 02:01 Patient will have a positive methacholine challenge, what does that even mean? Well, if Beta2 receptors then cause bronchodilation, well, what if you gave something that was a parasympathetic analogue? If it was a parasympathetic analogue, what does that then do to your bronchi? Bronchoconstriction. So, understand the concept that you already have spoken and discussed earlier. The patients will have a positive methacholine challenge. So, if your patient definitely has asthma they’re going to have a severe decrease in FEV1. 02:32 This is nearly 100 percent sensitive, but not necessarily specific. So with the methacholine challenge if it comes back to be negative, your patient most likely does not or is not experiencing asthma. Sensitivity, 100% big time important. 02:51 Let’s go ahead and take a look at this loop spirometry in the setting of bronchodilation. Take a look at the drug here in parenthesis. A Beta2 agonist such as your? Good, albuterol. You’ve heard of short-acting bronchodilators? So here, let’s take a look at the loop spirometry and I’m not going to go through detailed. You’re good here being able to identify your patient with an obstructive disease. Take a look at the red. The red is the disease isn’t it? How can you tell? You tell me about the depressed portion of your expiration. 03:28 Isn’t that, therefore, diagnostic of obstructive? Yes. So now, you’re given a bronchodilator. 03:35 Take a look at before in red, upon administration of a bronchodilator what happened with breathing? It got a lot better upon exhalation hence you find a increase in peak flow, is that clear? Whereas if you were to give metacholine or methacholine, what does that mean to you? Well, that's a parasympathetic analogue. So therefore, what would you then find? You’d find a patient who has a really hard time breathing out or exhalation in that one second. 04:05 So, look for that FEV1 to drop like crazy, what will then happen to your ratio? Good, decrease. Remember in asthma one of the few conditions in which if they’re not having a flare, loop spirometry will actually be normal. It’s only during those attacks episodically in which if you’re able to catch your patient during such a time you’d obviously find the obstructive type of pattern here. Now ultimately, the normal Now ultimately, the normal is going to be the dashed line. So, that’s what’s predicted.
About the Lecture
The lecture Asthma: Diagnosis by Carlo Raj, MD is from the course Obstructive Lung Disease: Basic Principles with Carlo Raj.
Included Quiz Questions
Which of the following statements is correct in the diagnosis of asthma?
- A decrease in FEV1 after exposure to methacholine.
- An increase in FEV1 after exposure to methacholine.
- No change in FEV1 after exposure to methacholine.
- A decrease in TLC after exposure to methacholine.
- A decrease in RV after exposure to methacholine.
Which of the following is not a finding in the diagnostic workup of asthma?
- Increase in FEV1/FVC.
- Increase in RV.
- Decrease in FEV1/FVC.
- Increase in TLC.
- A decrease in FEV1 after the administration of methacholine.
Which of the following is the correct set of PFTs in asthma?
- Decreased FEV1/FVC, increased TLC, increased RV
- Increased FEV1/FVC, decreased TLC, decreased RV
- Decreased FEV1/FVC, decreased TLC, increased RV
- Decreased FEV1/FVC, increased TLC, decreased RV
- Decreased FEV1/FVC, increased TLC, normal RV
Which of the following is most important in the diagnosis of asthma?
- History
- Chest x-ray
- Chest CT
- Chest ultrasound
- Carotid ultrasound
Customer reviews
3,0 of 5 stars
| 5 Stars |
|
2 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
2 |
Explanation is not logical ,needs improvement in teaching and to incorporate clinical features which hleps in differential diagnosis
to the point. One of my favourite lecturers. Really makes contents stick.
precise explanation given covering high yield facts about asthma diagnosis
Explanation is not coherent, does not use full sentences, connections between concepts are not logical. Does not articulate.