Playlist
Show Playlist
Hide Playlist
First-line Agents to Treat Tuberculosis – Antimycobacterial Agents
-
Slides First-line Agents to Treat Tuberculosis Antimycobacterial Agents.pdf
-
Reference List Pharmacology.pdf
-
Download Lecture Overview
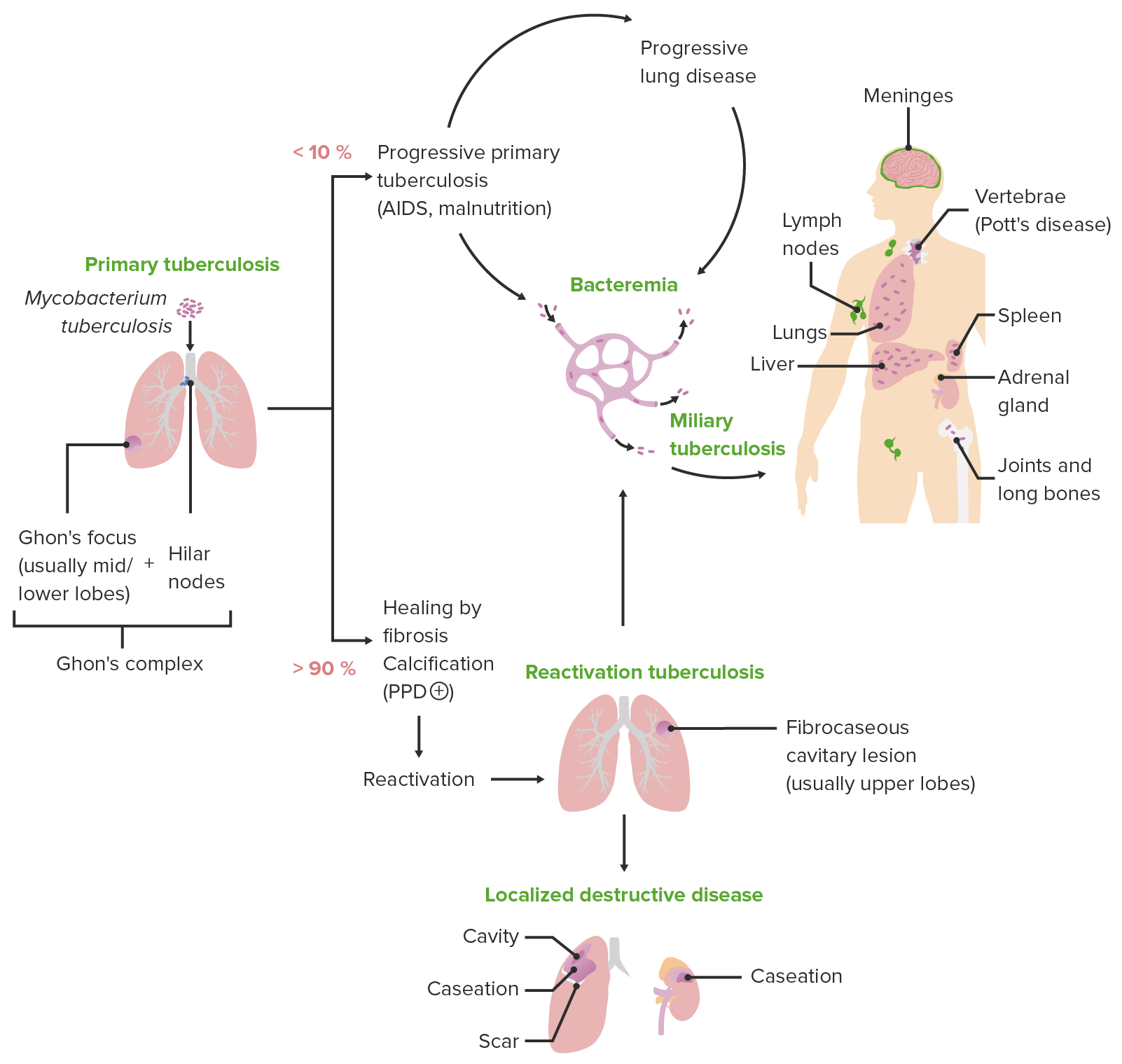
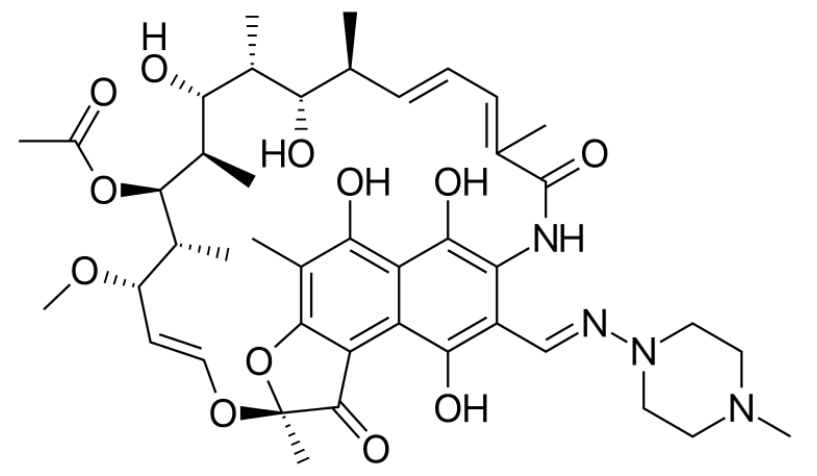
00:01 We have many agents used to treat Mycobacterium tuberculosis. 00:06 We have the first line agents, and we have other TB agents that are used in specific circumstances. 00:11 We'll go over them in some detail. 00:13 Now, let's start with isoniazid, and you'll see that we have letter designations or codes that we use. 00:20 And they were very popular probably a few years ago. 00:24 They're falling out of favor now because there's so many drugs. 00:27 There's so many abbreviations and there's a tendency to get them mixed up. 00:32 Isoniazid is similar to pyridoxine or vitamin B6. 00:37 It is a prodrug which means that the bacteria itself converts it into the active drug. 00:44 Now, what we want to do with isoniazid is we wanna inhibit cell wall production of the Mycobacterium species. 00:51 So just like a penicillin will and other bacteria, isoniazid works this way in a Mycobacterium. 00:59 In fact we sometimes call isoniazid, the penicillin of the anti-TB drugs. 01:05 It is bacteriocidal. 01:06 Now, when we have bacteriocidal medications and we give it to organisms that are slow-growing, they may not be as effective in terms of therapy. 01:17 So we have to add other agents to really improve the effectiveness of the therapy. 01:24 Therapeutic concentrations have to be achieved in multiple tissues, so we need to have blood levels that reach therapeutic concentrations in the serum, in the cerebrospinal fluid, and even in things like caseating granuloma in the lung. 01:38 So, you can see how using a medication isn't just about achieving good blood levels, it's about getting to where the disease is at. 01:47 If a person has central TB or if a person has TB and a caseating granuloma, just giving drugs to a certain therapeutic level in the blood isn't enough. 01:57 Now, the metabolism of isoniazid is actually quite interesting. 02:01 Isoniazid needs to be acetylated and it's acetylated into its active form. 02:07 There are two forms of the enzyme in any given population. 02:12 So when we look at the EC50 of a population, there - it actually has a bimodal distribution on the effectiveness curve. 02:19 So there are people who are fast metabolizers. 02:23 They fit under that first bump on the curved there. They're fast metabolizers. 02:27 Their serum concentrations peak at an hour. 02:30 There's another group of people who are slow metabolizers of this drug and they will actually peak at three hours. 02:37 If you wanna go over that concepts between fast and slow metabolizers, go back to the original pharmacology lectures looking at pharmacokinetics and you'll see what we're talking about. 02:48 Isoniazid resistance is a real problem, in fact it's a problem with all of the anti-TB drugs. 02:54 Resistance can be very rapid if you don't use isoniazid in combination with other medications. 02:59 This is why we use multidrug regiments. 03:02 Now, how resistance occurs, it's due to a point mutation in the genome of the bacteria that code for those critical enzymes that make isoniazid an active drug. 03:16 So if you think about it, if the bacteria is dormant, this drug isn't going to work because it's not going to become activated. 03:24 So this is an important consideration that we have to have when you're using INH. 03:29 Toxicity is very common with this drug. 03:32 Up to 20% or one in five people will have some sort of neurotoxicity associated with the symptoms with this drug. 03:39 I've often seen patients complain of paresthesia which is a fairly mild form of neurotoxicity. 03:45 Hepatotoxicity is common. You can have psychiatric problems. 03:50 You can have vitamin B6 related problems and G6PD issues as well. 03:55 So let's go into each of those a little bit more detail. 03:58 In terms of neurotoxicity, they can manifest in many different ways. 04:02 You can have a restless leg. You can have a peripheral neuritis which is actually quite painful. 04:07 And you treat these with pyridoxine which is actually vitamin B6. 04:12 The hepatotoxicity can be quite problematic and in fact, we've actually seen rare cases of fulminant hepatitis where people are running the risk of actually dying from the hepatitis due to the drug. 04:24 Often, we'll see abnormal liver function tests. 04:27 10 to 20% of all of our patients are going to have some kind of an abnormality to this drug with - in terms of their liver function. 04:37 We often will see jaundice in patients and we'll sometimes see a hepatomegaly in long-term treatment of patients. 04:44 Psychiatric problems are also common. 04:46 Patients who are on isoniazid often have a suicidal risk, and depression can be particularly harmful to these individuals. 04:56 We also see other kinds of psychiatric issues like a poor memory, poor mental function, poor mental concentration and sometimes, even just the idea of taking part in a drug regimen is quite off putting to these patients. 05:11 So the actual drug reduces the patients desire to be compliant with their therapy. 05:20 You can see where the problem comes from that. 05:23 Vitamin B6 depletion is a concern in patients around INH, so of course we need to replete vitamin B6. 05:30 The vitamin B6 maybe the cause of the suicide risk that we were talking about before and maybe a cause of the poor memory. 05:39 But also the vitamin B6 is important because of the peripheral neurological function as well. 05:44 So when I put vitamin B6 as a different category, it kind of matches up with the neurotoxicity and the psychiatric toxicity of this medication. 05:55 But I put it separately because we're not entirely sure that all of the neurological or psychiatric side effects of this drug are necessarily due to vitamin B6 depletion. 06:07 I wanna talk now about G6PD deficiency. 06:10 Glucose-6-phosphate deficiency is a disease that you will read about and you will come across. 06:16 And in some areas of the world like in India, it's actually quite common. 06:21 It is the most common enzymopathy with over 400 million people around the world affected by this particular problem. 06:29 Now the issue is with these G6PD patients is that isoniazid can actually trigger hemolysis. 06:36 And what we want to be aware of is the particular interaction between isoniazid and that particular disease. 06:43 Patients with a severe form called non-spherocytic hemolytic anemia are particularly prone to this problem with INH. 06:54 The most well-known of the micro bacterial agents is rifampin. 06:58 Rifampin is an inhibitor of DNA -dependent RNA polymerases. 07:04 But we can also remember rifampin from our earlier lectures as being the prototypical Cytochrome inducer. 07:10 So obviously, this drug is responsible for a lot of drug interactions. 07:15 I spoke briefly about the resistance to this particular medication and it's important in using multiple drug therapies. 07:22 In terms of how that resistance occurs, it's usually because the polymerase itself somehow doesn't bind to the drug. 07:28 Or there's changing in the drug binding pharmacokinetics of the polymerase and the rifampin. 07:35 Toxicity. Toxicity is always a concern with rifampin mostly it's due to drug interactions but also, the drug itself can be associated with light chain proteinuria that can be associated with skin rash, it can be associated with thrombocytopenias, it can be associated with nephritis and it can also be associated with certain types of liver dysfunction. 07:58 Let's move on to ethambutol. Ethambutol is a bacteriostatic drug, so remember that this is a drug that is going to stop the division and growth of this medication - of this bacteria. 08:10 It is not going to kill the bacteria that are already alive. 08:14 And it does so by cell wall production inhibition. 08:18 Now specifically in the cell wall, it inhibits this enzyme. 08:22 Now, arabinogalactan is a component of all cell walls. 08:27 If you inhibit the transferase, you have increased permeability of that cell wall, of the bacteria. 08:34 And so it becomes very brittle and you end up having depolarization of the cell or you're gonna have breakup of the cell. It this very well absorbed. 08:42 As a drug, it's excreted in the urine. 08:44 We're always giving it in combination with other anti-TB agents just like rifampin and others. 08:53 In terms of the toxicity of this medication; neurological, you get visual disturbances and it's a kind of an interesting visual disturbance. 09:02 Specifically, you will get a red/green color blindness. 09:06 So your ability to distinguish between red and green is impaired and you can only really pick it up in rare instances without doing a detailed red/green vision test. 09:18 Sometimes you can get an optic neuritis and you can actually get retinal damage. 09:23 So it's important to look in the eyes of every patient that is on ethambutol. 09:27 Now, a very common side effect of this medication is headache. 09:30 I see patients with this all the time. Sometimes patients can also be quite confused by it. 09:35 A metabolic issue that we sometimes see is hyperuricemia. 09:39 And finally, you can also get a peripheral neuritis with ethambutol which is very simple - similar to the peripheral neuritis you get with other TB drugs. 09:49 Finally, we can talk about pyrazinamide. 09:52 Now it's always, again given in combination with other medications. 09:57 It's well absorbed. It crosses inflamed tissues as well. 10:03 So if you have a meningitis, you can still give pyrazinamide, it will cross that inflamed meninges which is very handle - handy for a TB meningitis. 10:14 It's an essential part of treating bacterial tuberculosis meningitis. 10:19 So this is going to be an important exam question. 10:22 If you have a TB patient on your exam and they have bacterial - pardon me, tuberculosis meningitis, really think about making sure that this drug is in part - is in your armamentarium. 10:34 Again, like the previous drug, it's excreted in urine. It's removed by hemodialysis. 10:40 The half-life is really changed, it's increased in patients who have renal failures. 10:47 So remember that this is a renally excreted drug, it's excreted through hemodialysis. 10:52 Now, liver failure can also increase the half-life of this medication, so you have to keep that in mind in people who have any kind of hepatitis. 11:02 How does this drug work? It's kind of a unique mechanism of action. 11:06 Now inside the Mycobacterium organism, there's an enzyme that converts pyrazinamide into pyrazinoic acid. 11:15 Okay. Now, at low pHs, at a pH of say, five or six that pyrazinoic acid leaks out of the organism and it gets protonated. Okay? So go back to your old lectures on pH and PKA and just try and understand what's going on here. 11:33 It crosses the membrane back into the bacterium at this acid pH. 11:41 Now, the more acidic the tissue, the more concentrated the intracellular amount of pyrazinoic acid becomes. 11:51 So the agent is actually more effective against bacteria that are existing in an acidic environment. 11:58 Now in terms of your toxicity, one of the common problems that we see with this drug is non-gauty polyarthralgist. 12:07 Patients will complain of joint pains. 12:08 It seems like - initially, you think that it's kind of a gout kind of sensation because a lot of people will complain of ankle and toe pain. 12:16 But you'll start to realize that it is migratory. 12:19 Sometimes you'll get enlarged joints, sometimes you'll get it in the hands. 12:23 People will also have an asymptomatic hyperuricemia. 12:26 This makes it very hard to diagnose what is going on because if you assume that the toe pain that they're complaining of is gout in this situation, you could be quite wrong. Myalgias and rashes can occur. 12:40 Hepatic dysfunction with porphyria can occur with this drug. 12:45 And finally, this medication is not safe in pregnancy. 12:49 Remember, because it's interfering with normal metabolism of a growing fetus and because it's crossing barriers so well, you have avoid this medication because it can cause fetal abnormalities. 13:02 How do bacteria become resistant to the pyrazinimide? If the bacteria has a change in this particular gene mentioned here, there are changes in the enzymatic activity within the bacterial cell. 13:16 And that reduces the conversion into that pyrazinoic acid, and therefore you don't have as much active drug. This happens in about 16% of all cases. 13:28 And in patients who have multidrug-resistant TB or MDR-TB, 60% of people are resistant to pyrazinimide. 13:37 Moxifloxacin has become increasingly important in TB treatment as a key component of the new four-month regimen. 13:44 MFX works by inhibiting bacterial DNA gyrase and topoisomerase IV, essentially preventing DNA replication in TB bacteria. 13:54 What makes MFX particularly notable is its role as a replacement for ethambutol in the shortened regimen. 14:01 However, this comes with important caveats. 14:04 First, resistance can develop through mutations in the GIR-AB genes and if this occurs, you'll typically see cross-resistance with other fluoroquinolones. 14:15 The toxicity profile is distinct from other TB drugs and requires specific monitoring. 14:21 The most significant concern is QT prolongation, which necessitates regular cardiovascular monitoring. 14:29 Other important adverse effects include tendon problems and CNS effects. 14:34 A critical point for clinical practice, you cannot substitute other fluoroquinolones for MFX in the four-month regimen. 14:42 This is a common question that comes up, but the evidence base specifically supports MFX in this context.
About the Lecture
The lecture First-line Agents to Treat Tuberculosis – Antimycobacterial Agents by Pravin Shukle, MD is from the course Antimicrobial Pharmacology. It contains the following chapters:
- Tubercolosis Agents - First Line Drugs
- Tubercolosis Agents - Second Line Drugs
Included Quiz Questions
What is a first-line agent used to treat M. tuberculosis?
- Ethambutol
- Streptomycin
- Ethionamide
- Rifabutin
- Ciprofloxacin
A patient being treated for tuberculosis develops restless leg syndrome. What CORRECTLY describes the management of this scenario?
- Start pyridoxine and continue isoniazid.
- Discontinue isoniazid immediately, but maintain the other drugs in the regimen.
- Observe the patient only, as it is usually a self-limiting side effect.
- Switch to the 2nd line regimen of antituberculosis drugs.
- Start probenecid and decrease the dose of isoniazid.
Which antituberculosis drug works by inhibiting the DNA-dependent RNA polymerase?
- Rifampin
- Isoniazid
- Streptomycin
- Pyrazinamide
- Ethambutol
What may be found in up to 40% of patients taking pyrazinamide?
- Non-gouty polyarthralgia
- Gout
- Visual disturbances
- Orange discoloration of urine and feces
- Myalgia
Which medication may cause vitamin B6 deficiency?
- Isoniazid
- Ethambutol
- Clarithromycin
- Streptomycin
- Rifampin
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Good explanation of the drugs side effects, also very complete