Playlist
Show Playlist
Hide Playlist
Case Studies – Antimycobacterial Agents
-
Slides Case Studies Antimycobacterial Agents.pdf
-
Reference List Pharmacology.pdf
-
Download Lecture Overview
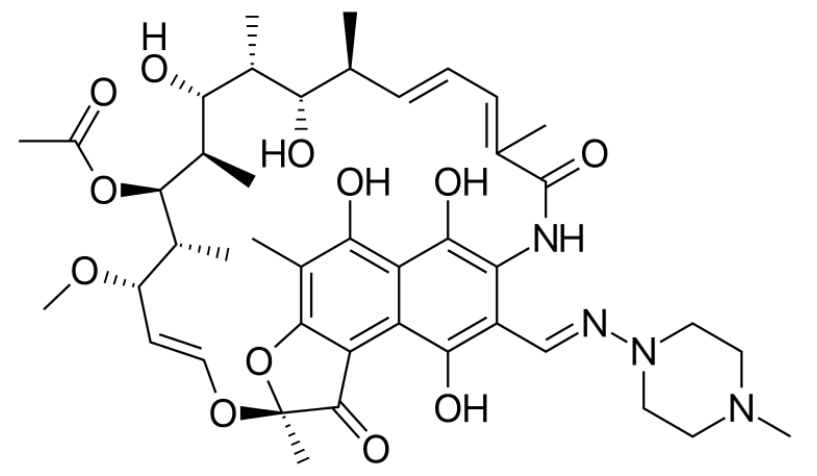
00:00 Let's move on to a question. 00:03 A woman from a first nations reserve in western Alaska presents with cough with flecks of blood in her green sputum. 00:10 She has a three month history of fatigue, weight loss and poor appetite. 00:15 Her sputum is identified with Mycobacterium tuberculosis. 00:19 She is not pregnant and tests negative for HIV. 00:21 There has been one historical case from her reserve without resistance patterns. 00:26 The appropriate course of action would be A. Initiate isoniazid, rifampin, pyrazinamide and streptomycin. 00:35 B. Initiate rifampin to treat for 9 months. 00:39 C. Initiate isoniazid for 18 months. 00:44 D. Initiate rifampin, INH, pyrazinamide, and ethambutol. 00:49 Or E. Initiate pyrazinamide for 18 months. 00:55 Okay you chose D and that's correct. 00:58 The American Thoracic Society (ATS), Centers for Disease Control and Prevention (CDC), and Infectious Diseases Society of America (IDSA) recommend an initial four-drug regimen consisting of isoniazid (INH), rifampin (RIF), pyrazinamide (PZA), and ethambutol (EMB) for the treatment of drug-susceptible tuberculosis This regimen is advised due to the global prevalence of isoniazid resistance, which necessitates the inclusion of ethambutol until drug susceptibility results are available. 01:31 The management of TB for drug-susceptible pulmonary tuberculosis in nonpregnant adults who do not have HIV is structured into two main phases: an intensive phase and a continuation phase. 01:44 The intensive phase is the first line of attack against the TB bacteria. 01:48 It lasts for two months and involves a combination of four drugs: isoniazid, rifampin, ethambutol, and pyrazinamide. 01:57 This combination, often referred to as the "RIPE" regimen, is designed to rapidly decrease the bacterial load in the patient's body. The primary objective during this phase is to make the patient less contagious and to lay the groundwork for the subsequent continuation phase. 02:14 Following the intensive phase, patients transition to the continuation phase, which typically lasts for four and a half months. During this period, the treatment regimen is simplified to just two drugs: isoniazid and rifampin. 02:28 The goal of the continuation phase is to completely eradicate any remaining TB bacteria and to prevent a relapse of the disease. However, the continuation phase duration might extend beyond the standard 4 and one-half months under certain conditions. 02:46 For example, if the patient's sputum cultures remain positive after the intensive phase, this indicates that the bacteria have not been fully eradicated, necessitating a longer continuation phase. Similarly, patients who exhibit cavitary disease on their initial chest radiographs often require an extended treatment period due to the more complex nature of their infection. Additionally, any complications such as drug resistance or interruptions in treatment would also require extending the therapy to ensure complete bacterial clearance. 03:21 For some patients, a shortened treatment regimen of four months might be appropriate. 03:25 This regimen begins with an intensive phase of eight weeks using rifapentine, isoniazid, pyrazinamide, and moxifloxacin. It is followed by a continuation phase of nine weeks with rifapentine, isoniazid, and moxifloxacin. This shorter regimen is an option for select patients who meet specific clinical criteria and prefer a quicker course of treatment. 03:52 Throughout the treatment process, decisions are guided by sputum culture results and chest radiograph findings. These tools are essential in assessing the patient’s response to treatment and determining whether any adjustments to the treatment plan are necessary. 04:11 The other multidrug answer in option A is not recommended, and single drug treatment of active TB is never a reasonable choice on exams or in the TB clinic. 04:21 Now let's go on to the next question. 04:23 The woman from question one received the appropriate treatment as part of the regimen, the CDC consultant also added pyridoxine or vitamin B6 to her regimen. 04:34 What was the purpose of pyridoxine? Now if you're not sure what the first question was, it's just dealing with a woman from a reserve in Alaska who is found to have TB in the sputum. 04:48 Let's take a look at our choices. 04:50 A. Pyridoxine will reduce the risk of pulmonary scarring during treatment. 04:54 B. Pyridoxine will reduce the risk of hepatotoxicity during treatment. 04:59 C. Pyridoxine will reduce the risk of dental erosions during treatment. 05:05 D. Pyridoxine will reduce the risk of arrhythmia during treatment. 05:10 or E. Pyridoxine will reduce the risk of neurotoxicity during treatment. 05:16 And the answer of course is E. 05:18 Pyridoxine (vitamin B6, 25-50 mg/day) is given with isoniazid to individuals at risk for neuropathy (e.g., pregnant women and breastfeeding infants; and individuals with HIV infection, diabetes, alcoholism, malnutrition, chronic renal failure, or advanced age). It is also given in higher doses (100 mg/day) to patients who already have peripheral neuropathy.” This is a third question in the a string of two. 05:47 The woman from question 1 was on oral contraceptives. 05:50 If you've lost two questions, just be aware that she was started on a 4-drug regiment for TB and she lives on a reserve with no worrisome resistance patterns. 06:00 She does not wish to get pregnant. 06:02 Which drug is most likely to interfere with the oral contraceptive agent? Is it A. Ethambutol, B. Isoniazid, C. Rifampin, D. Pyridoxine or E. Pyrazinamide. 06:18 Good for you, you chose rifampin. 06:21 Now rifampin is an important thing to think about. 06:25 Because rifampin is the prototypical cytochrome inducer. 06:29 And it is the drug that we talk about, when we're talking about multidrug interactions. 06:34 So rifampin is going to be the answer in that case. 06:40 Let's go on to the next question. 06:43 A 36 year old HIV positive male is tachypneic and hypoxic. 06:48 His chest X-ray shows a right middle lobe consolidation. 06:52 He was diagnosed with microbaterium avium complex or MAC. 06:56 The appropriate treatment is one of the following. 06:58 Is it A) Clarithromycin with rifabutin. 07:02 Is it B) Azithromycin with rifabutin. 07:05 Is it C) Isoniazid with rifabutin. 07:09 Is it D) Azithromycin or Clarithromycin with ethambutol Or is it E) Ethambutol, streptomycin, rifampin, isoniazid and penicillin. 07:22 Good, you chose D. 07:24 A third agent, for example, rifabutin, is added in patients failing antiretroviral therapy or in patients with a high mycobacterial burden (for example, based on quantitation in the blood culture). 07:36 Microbaterium avium complex or MAC was actually first described as Lady Windermere syndrome. 07:44 Now who is Lady Windermere. 07:45 She was a character in Oscar Wilde's play. 07:48 She was one of these very proper people who wouldn't cough or wouldn't expectorate. 07:53 And actually it was surprisingly common in these women to see right middle lobe pneumonia. 07:57 MAC made a come back in the AIDS era. 08:00 It is treated with a 2-drug regimen that includes a macrolide with ethambutol; rifabutin is added in patients failing antiretroviral therapy or in patients with a high mycobacterial burden. That's it. 08:13 You completed a very tough section. 08:15 I'm really proud of you. 08:17 Now go up to that exam and show them what you know.
About the Lecture
The lecture Case Studies – Antimycobacterial Agents by Pravin Shukle, MD is from the course Antimicrobial Pharmacology.
Included Quiz Questions
Which vitamin is commonly used with antituberculosis drugs?
- B6 (pyridoxine)
- B1 (thiamine)
- B2 (riboflavin)
- B3 (niacin)
- B9 (folate)
What is an adverse effect of rifampin?
- Drug interactions (CYP-450 inducer)
- Hair loss
- Photosensitivity
- Enamel hypoplasia
- Tubulointerstitial nephritis
What statement is correct regarding tuberculosis?
- A 4-drug regimen should be used for most patients
- A 3-drug regimen is appropriate in an area with 8% resistance to INH.
- Ethambutol can be used as a monotherapy against tuberculosis.
- Pyridoxine supplementation increases hepatotoxicity risk.
- Azithromycin and rifabutin are both effective against M. tuberculosis.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |