Playlist
Show Playlist
Hide Playlist
Acute Bacterial Diarrhea: Food-bacteria Associations
-
Slides InfectiousDiarrhea InfectiousDiseases.pdf
-
Reference List Infectious Diseases.pdf
-
Download Lecture Overview
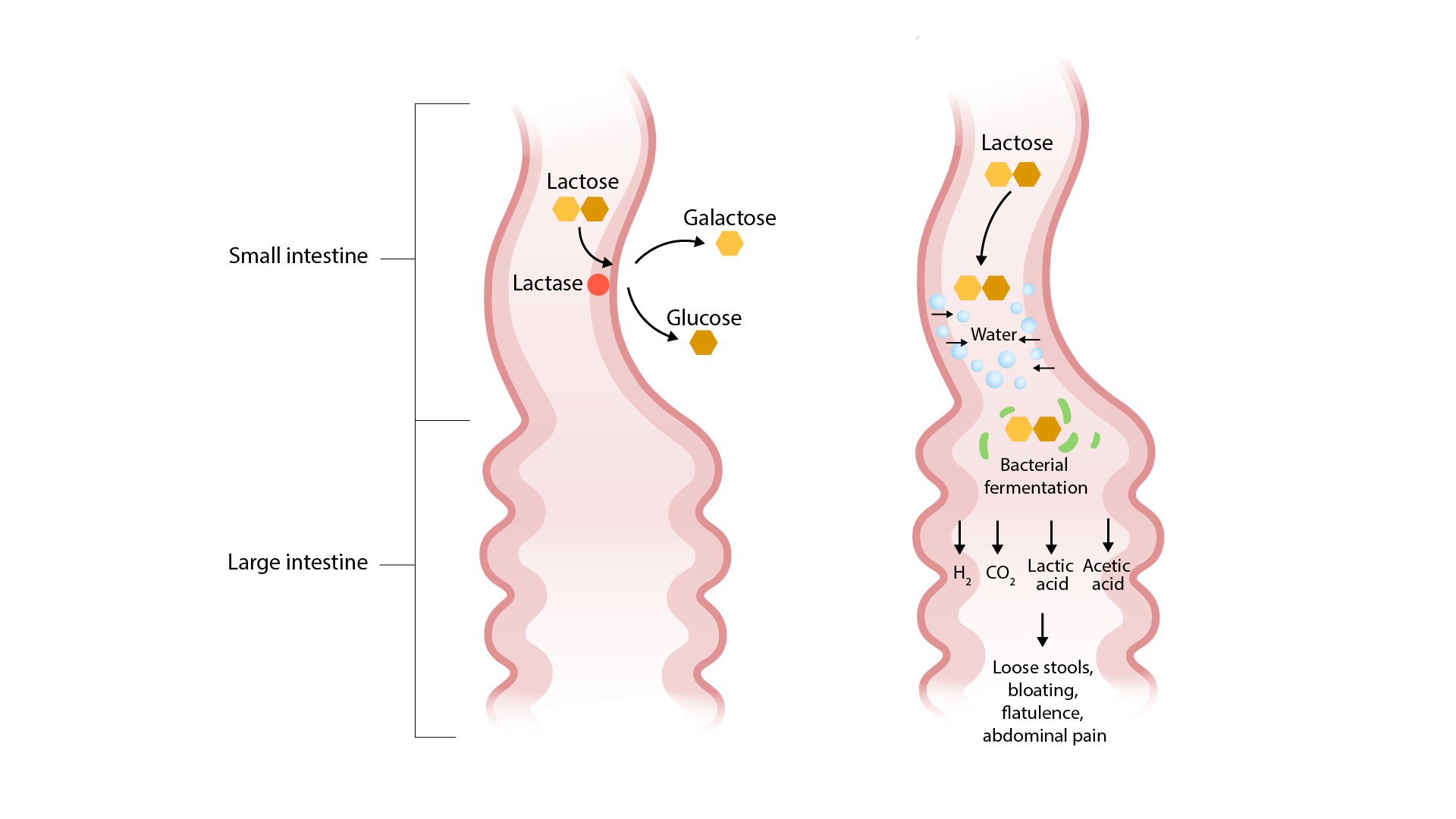
00:01 So I want to just go over some brief associations with various types of food and the types of diarrhea that you can get from it. 00:12 If you're talking about meat and dairy products. 00:16 Look for Campylobacter Jejuni, Salmonella, E. coli O157:87 and Listeria Monocytogenes. 00:27 On the other hand, if it's Seafood, you should have a clue. 00:30 It could be Vibrio Cholerae, Vibrio Parahaemolyticus or Vulnificus, and if it's freshwater, seafood, Aeromonas Hydrophila. 00:43 And it's interesting that Listeria is also associated with this. 00:50 Vegetables. 00:52 Here's listeria again. 00:55 Green onions for some reason that I'm not certain about, Shigella, Leaf Lettuce, E.coli O157 and this sometimes comes up on board exams Bacillus Cereus and fried rice, bacillus cereus, fried rice. 01:21 So when you're trying to treat somebody who's got bad diarrhea, what do you do? Well, you've got to replenish their water their salt and their sugar, and this is obviously for more of the large volume types of diarrhea the small bowel. 01:38 The World Health Organization recommends 3 1/2 grams of sodium chloride, 2 grams of trisodium citrate or 2 1/2 grams of sodium bicarbonate, 1.5 grams of potassium chloride, 2 grams of glucose or 40 grams of sucrose. 01:58 You can make a homemade version by using a teaspoon of sodium chloride, half a teaspoon of baking soda, 4 tablespoons of sugar and a liter of water. 02:10 But I wanted to make this one point, Gatorade is not a substitute for the oral hydration solutions that you need, it doesn't have enough of the electrolytes. 02:20 So after that kind of homemade mixture, you've actually got a fairly reasonable way to hydrate patients. 02:29 You've got 990 milliliters of water, 10 grams of protein, 60 grams of carbohydrate, 3.4 grams per deciliter of sodium, and 0.9 grams per deciliter of potassium. 02:44 What about anti-diarrheal agents. 02:47 A lot of people use Bismuth Subsalicylate and there's no question that it has some efficacy not only in the treatment but in the prevention of diarrhea, especially for Turista and a lot of people take the oral pill forms with them if they travel to a place like Mexico. 03:12 And they can actually with Bismuth Subsalicylate, decrease the incidence of travelers diarrhea by 40 to 60 percent. 03:21 On the down side of things their stools will be black and their tongue maybe black which is maybe aesthetically not pleasing. 03:31 Loperamide is also pretty effective. 03:35 But I just want to make one caution if somebody has diarrhea due to invasive pathogens. 03:45 One of the body's defense mechanisms is diarrhea. 03:50 Diarrhea enables the body to get rid of pathogens. 03:55 So if you use something like loperamide or other agents to slow down... 04:01 diarrhea, you may actually slow down the normal clearance of the pathogen in the intestine and things like this have rarely been associated with megacolon. 04:16 So you need to use it sparingly and probably not try to use it in invasive diarrhea. 04:26 Combinations of Kaolyn and Pectin that are available over-the-counter are probably not very effective. 04:33 They may increase the bulk of a diarrheal stool, but they really don't do much. 04:42 Now, what about antibiotics? I think you need to realize that antibiotics are only of modest benefit and that would be in severely ill patients. 04:54 So in general, you wouldn't use antibiotics for like non-typhoidal Salmonella. 05:04 As a matter of fact if you use antibiotics for that hemolytic-uremic syndrome, you may actually increase the toxin production. 05:16 And so we would stay away from antibiotics, If you thought you were treating the hemolytic uremic syndrome. 05:24 And the other reason that we try to stay away, diarrhea is very common, especially in the developing worm. 05:32 Antibiotics can be obtained in many countries over the counter. 05:36 And so it's small wonder that we're starting to see lots of antimicrobial resistance and I'm sure you've read in your local papers about the problem of bad bugs. 05:48 Furthermore the antibiotics have side effects of their own, sometimes diarrhea. 05:54 And then we've already mentioned about Clostridium Difficile Colitis, which we don't want to produce on top of whatever the patient already as it cause of their diarrhea. 06:08 So empirical antibiotics should be given only to patients who have moderate to severe travelers diarrhea and you can reduce the prevalence of diarrhea from 3-5 days to 1-2 days. 06:26 Probably wouldn't use it, unless the patient's having more than eight stools a day or evidence of volume depletion and had symptoms for more than a week hospitalized patient or patients who are immunocompromised. 06:41 But if you decide to use antibiotics by all means, stool cultures should be sent first so that you know what you're dealing with. 06:51 The treatment for adults would be a fluoroquinolone, 3-5 days worth, but remember not if E.coli o157 807 is suspected and not in areas where there's high prevalence of resistance. 07:09 So for children, we cannot give them fluoroquinolones because of the negative effect on growing connective tissue. 07:17 So we use trimethoprim sulfa for kids. 07:21 Or alternatively we would use a azithromycin, but because we've gotten stool cultures hopefully in all of these patients, we would then adjust our antibiotics based upon cultures and susceptibilities. 07:37 And that concludes my discussion of infectious diarrhea. 07:41 I hope it was helpful.
About the Lecture
The lecture Acute Bacterial Diarrhea: Food-bacteria Associations by John Fisher, MD is from the course Gastrointestinal Infections. It contains the following chapters:
- Acute Bacterial Diarrhea (Food-bacteria Associations) – Signs/Symptoms
- Non-inflammatory Enteric Infection Rx (Anti-diarrheals)
- Bacterial Diarrhea (Cautions About Antibiotic Rx)
- Bacterial Diarrhea (Empirical Antibiotics)
Included Quiz Questions
Which of the following is NOT included in the recommendations by the World Health Organization for oral rehydration solutions?
- Magnesium sulfate
- Sodium chloride
- Sodium bicarbonate
- Glucose
- Potassium chloride
Which of the following is an antidiarrheal agent used for non-antibiotic symptomatic management of mild to moderate travelers' diarrhea?
- Bismuth
- Azithromycin
- Rifaximin
- Ibuprofen
- Sorbitol
In a patient with acute diarrhea, empirical antibiotic treatment is most appropriate with which of the following indications?
- Eight stools per day
- Hemolytic uremic syndrome
- History of prior clostridium difficile colitis
- Absence of fever
- Fifty-four years of age
In a patient with a flare of ulcerative colitis due to a bacterial infection, which of the following medications is MOST likely to increase the risk of toxic megacolon?
- Oral antidiarrheal agents
- Intravenous antibiotics
- Intravenous infusion of isotonic saline
- Intravenous glucocorticoids
- Infliximab
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
It is a pleasure listening to such an experienced and passionate professor. Thank you! I just wish there was also a part talking about non-bacterial pathogens causing gastroenteritis (viral and parasitic in particular). Thanks again.