Playlist
Show Playlist
Hide Playlist
Ventricular Tachycardia: Treatment
-
Slides Tachyarrhythmia VentricularTachycardia CardiovascularPathology.pdf
-
Download Lecture Overview
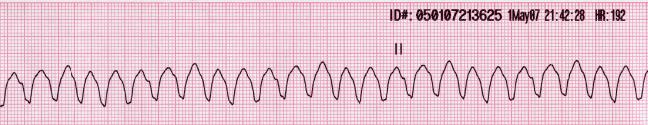
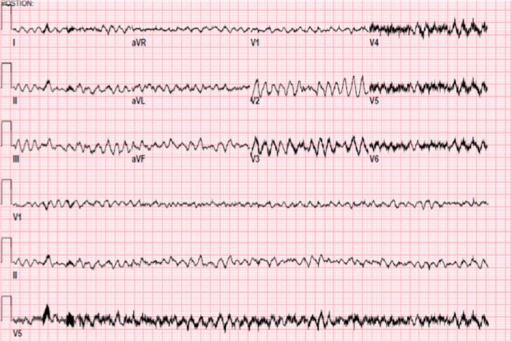
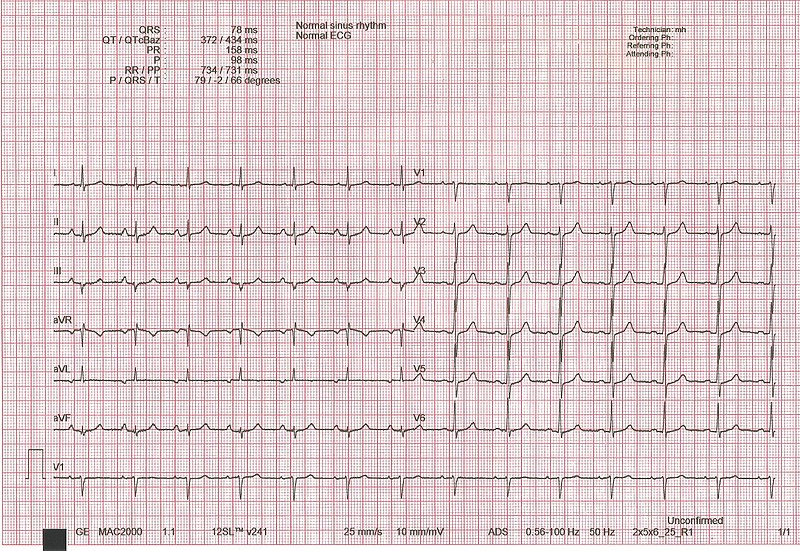
00:00 Now ventricular tachy. Sustained ventricular tachycardia requires immediate intervention, why? You are worried about v.fib and once v.fib kicks in, you are playing with death there and you do not want to do that. If it is hypertension, no pulse. Stop there. Why no pulse? If it is ventricular tachy, you do not have effective cardiac output. You don't have effective cardiac output because what have you done to the diastolic interval? Think about that. Don't you want just enough diastole so that your left ventricle shows up with blood. And you have ventricular tachy, real quick? So therefore, how in the world can you possibly fill that up with blood? You can't, it's moving too quick. So there is no cardiac output. 00:49 What happens to pulse? It decreases. So what is your next step of management. Cardiovert, what does that mean? It means that you are trying to slow things down so that you reestablish the time that is necessary to fill up your heart with blood to restore that hemodynamic instability. If asymptomatic, pay attention here now. Amiodarone, huge drug for you. 01:12 It is going to make come back for use now and amiodarone technically fine. People say that it is part of class III antiarrhythmics and class III to you should mean potassium channel blocker, but could it have sodium channel type of activity? Could it have beta-blocker type of activity? Could it have calcium channel blocking activity? Sure it can. So amiodarone is one of those drugs that kind of has all activities. Universal, but you can use it to cardiovert medically. Lidocaine is Ib, but failure to convert may then require sedation and cardioversion. 01:51 So there are times when you can use medical cardioversion, which I will pay attention to which drugs. And then at some point you must resort to sedation, electrical cardioversion. 02:00 It is important that you make sure that you are able to properly sustain heart rate in a regular fashion. 02:09 To differentiate between SVT and VT, beyond the scope to a certain extent, but I will still keep this in mind. Remember up until now, we have done SVTs and we looked at four major ones, know these four well, afib, atrial fibrillation, multifocal atrial tachycardia, and WPW. Know these four well, at least, and then you have VT. But what are some other clues that you are want to pay attention to? P waves are clearly present preceding each QRS narrow complex. So this would then favor what? SVT. Supraventricular tachycardia. For example, think of atrial fibrillation, atrial flutter, those P waves were clearly distinct to a certain extent. 02:50 But the QRS complex was definitely there as being a narrow complex and by distinct we don't necessarily mean it looks like normal sinus. The fact that maybe it was wave like, maybe it was sawtooth, or maybe there's 3 distinct P waves like we found in multifocal atrial tachycarrhythmia. If the patient has CAD stands for coronary arterial disease, ICMP stands for ischemic cardiomyopathy, then it is likely ventricular tachy. Is that clear? So diseases in which the blood vessels have been affected more likely would be VT. Keep that in mind. Most wide complex tachy will be VT. Most narrow complex VT, so WCT stands for wide complex tachycardia. And for board purposes, make sure you know that there most likely will be ventricular tachycardias. If the QRS complex are narrowed, think of it is being the P waves pushing the Q waves together, the narrow complex, and then most likely will be SVTs. Simple clues that will help you all tremendously and you don't want to sit there, wasting precious time and, more importantly, feeling frustrated. 04:08 AV dissociation. We talked about this where the P wave has no correlation with the QRS complex independent, favors ventricular tachy.
About the Lecture
The lecture Ventricular Tachycardia: Treatment by Carlo Raj, MD is from the course Arrhythmias: Basic Principles with Carlo Raj.
Included Quiz Questions
What life-threatening arrhythmia can result from sustained ventricular tachycardia?
- Ventricular fibrillation
- Atrial flutter
- Pulseless electrical activity
- Atrial fibrillation
- Supraventricular tachycardia
What causes insufficient cardiac output in pulseless ventricular tachycardia?
- Decreased filling of the heart in diastole
- Decreased afterload
- Delayed depolarization of the sinoatrial node
- Increased preload
- Increased contractility
What is the next step in the management of asymptomatic ventricular tachycardia that has failed to respond to amiodarone or lidocaine?
- Sedation and cardioversion
- Dobutamine
- Amlodipine
- Propranolol
- Diltiazem
Which of the following findings on ECG usually indicates a supraventricular tachycardia rather than a ventricular tachycardia?
- Narrow QRS complex (less than 0.12 seconds)
- T waves after each QRS complex
- P waves independent of the QRS complex
- AV dissociation
- Wide complex tachycardia ( > 0.12 seconds)
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |