Playlist
Show Playlist
Hide Playlist
Varicose Veins: Pathophysiology and Clinical Manifestations
-
06 CVP Vein and Lymphatic Pathology.pdf
-
Reference List Pathology.pdf
-
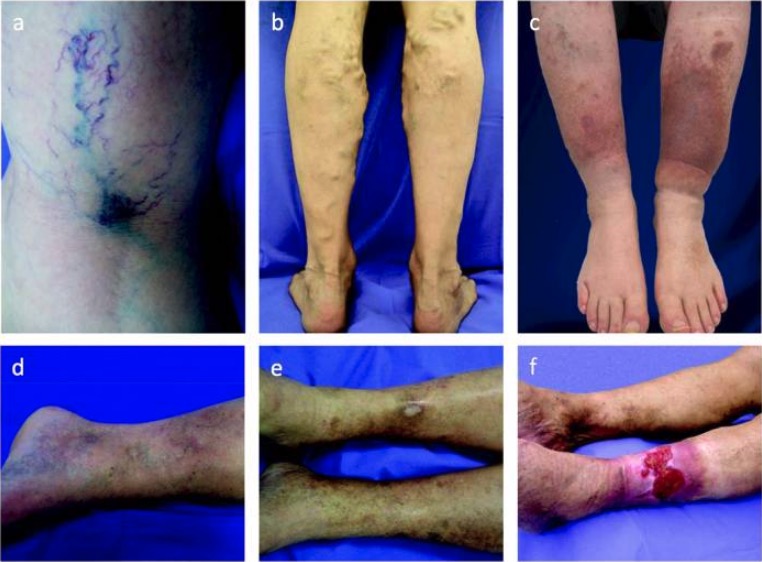
Download Lecture Overview
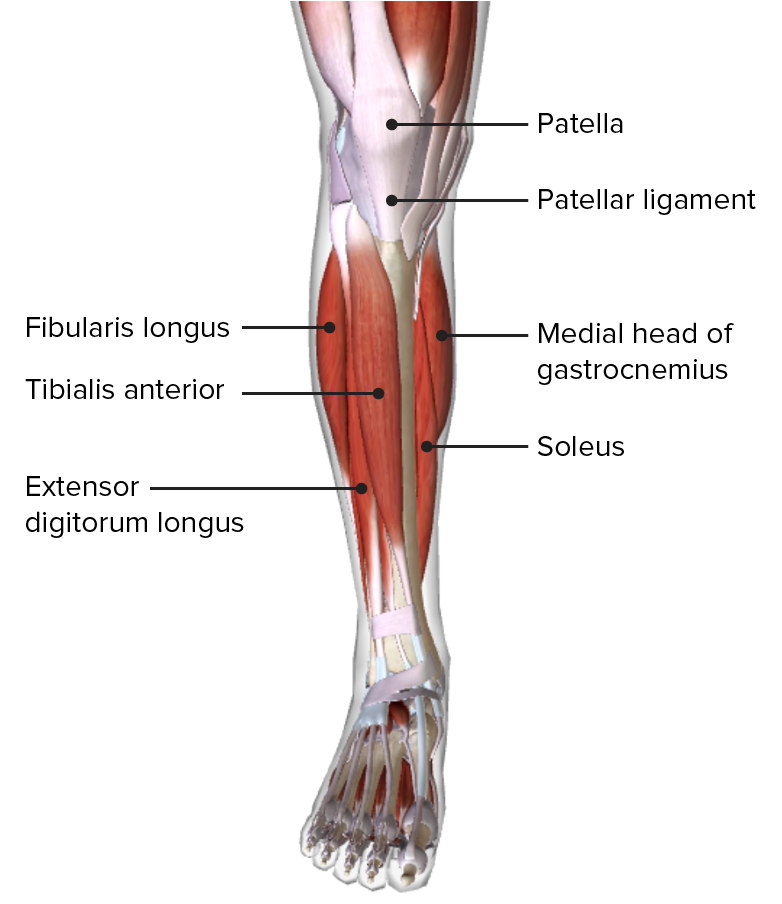
00:01 Welcome back. 00:03 We are now going to talk about vein and lymphatic pathology. 00:06 We kind of lump them together, they are different entities they have different kind of manifestations and different importance, but we're going to put them together to make one very nice package for you. 00:19 So, here's the roadmap we're going to talk about vein pathology first and then lymphatic pathology second and we're off and running. 00:26 By way of a very quick review, remember that the vein, still has the same three-layered or three-tunica architecture, as any vessel in the body. 00:35 An endothelium, that sits on a basement membrane, that is surrounded by relatively less organized smooth muscle media, and then the adventitia around it. 00:46 When we talk about, injury to the venous wall, all three of these layers can come into the equation. 00:55 So, things that will affect venous return and the first kind of topic we're going to talk about, is, varicose veins. 01:02 So, relating to poor venous return of blood and relative stasis. 01:09 If we're talking about getting blood back to the heart, through the venous circulation, recall that there's not a lot of pumping action that's happening, at the level of the capillaries and into the veins, there's relatively little pulsatile activity, there's a little tiny bit, but left to its own devices, especially pumping against one gravity, 1G, up from a person who is standing upright, from the feet into the heart, you need additional kind of factors to help blood return. 01:41 If any of those are messed up, very scientific term, “Messed up.” If any of those are messed up then you're going to have “Venous stasis.” So, intrinsic factors in terms of this venous return to the heart, particularly when you're standing upright, includes, the venous gradient, so, the pressure differential between the heart and the other structure below. 02:03 The valve integrity, so again, in our extremities, o we have valves, that allow unidirectional flow most of the time, and prevent regurgitant flow especially when we're standing against gravity. 02:18 There's a muscular venous pump. 02:20 What's meant by that? Well in fact, the skeletal muscle as I’m standing here now, flexing my calves, so that I don't get a deep venous thrombosis. 02:29 I’m actually, moving the muscle which is squeezing or milking the veins, to return the blood back. 02:34 And then there's an abdominal thoracic pump, same deal. 02:38 I bend over, I lean back. 02:40 I bend over, I lean back. 02:42 That muscular activity, is also helpful, in terms of improving return flow. 02:48 The cardiac pump does have a degree a role in this, because it's pumping, it's got to pump forward. 02:56 That means that it's basically sucking blood from the back end, from the venous circulation, and then there is some degree of sympathetic tone. 03:04 Tone is not as great an issue in the in the venous bed, as it is in the arterial bed. 03:10 But nevertheless, we can affect, whatever smooth muscle is there in the media and squeeze it or relax it, as necessary. 03:18 There are other extrinsic factors, I've already talked about gravity a couple times. 03:22 I’m standing here before you there's 1G, forcing the blood to stay down. 03:28 Clearly if I’m in a space capsule, going into space, there's going to be more, but for most of us, it's just having to fight against 1G of gravity. 03:36 There's atmospheric pressure which also has an influence, and then external compression. 03:42 So, if I am wearing a very tight rubber suit, for whatever reason, then that's going to also affect the venous return. 03:52 Okay, the most important structure, besides the muscles and the other things that we talked about, are the valves. 03:59 And so, this is a normal valve and you can see that when blood is flowing, from foot to heart, that the valves are open and then when there is not flow, the valves close, preventing regurgitation. 04:14 So, this normally keeps the blood moving in one direction, from the veins in the extremities—arms and legs. 04:24 Now, in the case of a varicose vein, when you have a dilated vein, that is tortuous, the vessel wall has been spread apart, for a variety of reasons, then the valves can't close, and we get regurgitant flow. 04:41 And that's basically all a varicose vein is, it has become lax, it has lost the normal wall tone, to maintain the patency of those valves. 04:55 So, how does this happen? How do we get varicose veins, incredibly common entity? It's produced by chronically increased intraluminal pressures and weakened vessel wall support. 05:04 So, any variety of things, that will increase the pressure, regurgitant into the vein or will weaken the wall, will lead to varicose veins. 05:14 So, the ones the veins that are most commonly affected, are those that are superficial, the ones that are deep are not typically affected by varicosities, because they are surrounded by muscle and get constantly milked, but the peripheral ones don't have a lot of muscle around them, so, they will be more prone to develop the varicosities. 05:34 It's really important, I already said, it's a very common entity, a fifth of men and a third or even more of women, will develop varicose veins over the course of their lifetime, so, this is a very common and, in some cases, very important entity. 05:49 So, what puts you at risk for doing this? You have things that are non-modifiable, so, things you're stuck with like advanced age. 05:59 If you're a woman, if you've been pregnant, if there's a family history of venous disease, if there's prior thrombosis, prior trauma to the extremity, congenital abnormalities, or just laxity of the various structures of the venous wall. 06:15 Things you can modify theoretically, there's obesity, smoking, sedentary lifestyle. 06:21 In fact, the more you get up and exercise, not only will you improve the obesity, but you're also doing that muscular milking, of the venous circulation. 06:31 So, again pathophysiology, it's already kind of clear from the discussion that we've already had, but let's spell it out in detail. 06:39 Venous hypertension, so increased pressure, within the venous circulation, will cause obviously the walls to stretch, there's not much media there, so, a little bit of pressure a little bit of volume, will go a very long way to causing stretching of the wall. 06:55 As part of that stretching, we can also compromise the vasa vasorum of the larger veins, that can lead to venous wall hypoxia and that will lead to inflammation and then subsequent remodeling. 07:11 Is the venous wall relaxes, because of hypoxia and this stretching, then we have relative blood stasis and as blood becomes more static and the vein valves no longer coapt to close, then we get increased volume and it becomes a very vicious circle. 07:33 Signs and symptoms. 07:34 So, most of you have had relatives, grandparents certainly, who have varicosities. 07:42 They demonstrate stasis, so, if you actually palpate them, there is kind of dilated bubbles of venous blood that are present within them. 07:52 That congestion will actually then permeate into the additional tissue, so that you can get edema, and you can get pain. 08:01 As a result of the kind of stasis, you can have relative hypoxia, that will then trigger acidosis and will trigger nervous inputs, that will be manifested as pain. 08:14 If we thrombose a vein and then we are causing no flow through that, because of the blood clot the tissues more distal, may also become relatively ischemic, and also, painful. 08:26 And I've already mentioned thrombosis is a real risk in this setting. 08:32 If you do not have good venous outflow from a tissue, that can be a cause of infarction to the almost the same extent, as if you'd have poor arterial inflow into the tissue. 08:44 We get stasis dermatitis, kind of a brawny induration of the skin, and as the tissue becomes ischemic, then you can get secondary ulceration.
About the Lecture
The lecture Varicose Veins: Pathophysiology and Clinical Manifestations by Richard Mitchell, MD, PhD is from the course Vein and Lymphatic Pathology.
Included Quiz Questions
Which of the following is an intrinsic factor that affects venous return to the heart?
- Musculovenous pump
- Gravity
- Atmospheric pressure
- External compression
- High altitude
Which of the following is a modifiable factor in the development of varicose veins?
- Obesity
- Female sex
- Pregnancy
- Ligamentous laxity
- Prior extremity trauma
Which of the following is an extrinsic factor that affects venous return to the heart?
- Gravity
- Valve integrity
- Sympathetic tone
- Venous gradient
- Abdominothoracic pump
Which statement is correct concerning the risk factors in the development of varicose veins?
- Pregnancy increases the risk.
- Smoking is a non-modifiable risk factor.
- Advanced age decreases the risk.
- Congenital abnormalities are modifiable risk factors.
- Prolonged standing decreases the risk.
Which of the following could be a complication of varicose veins?
- Stasis dermatitis
- Diminished lower extremity pulses
- Ecthyma gangrenosum
- Erythema nodosum
- Erythema marginatum
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
1 customer review without text
1 user review without text