Playlist
Show Playlist
Hide Playlist
Type 2 Diabetes (Adult Onset Diabetes)
-
Slides Insulin Dependent Diabetes Mellitus Type 2.pdf
-
Download Lecture Overview
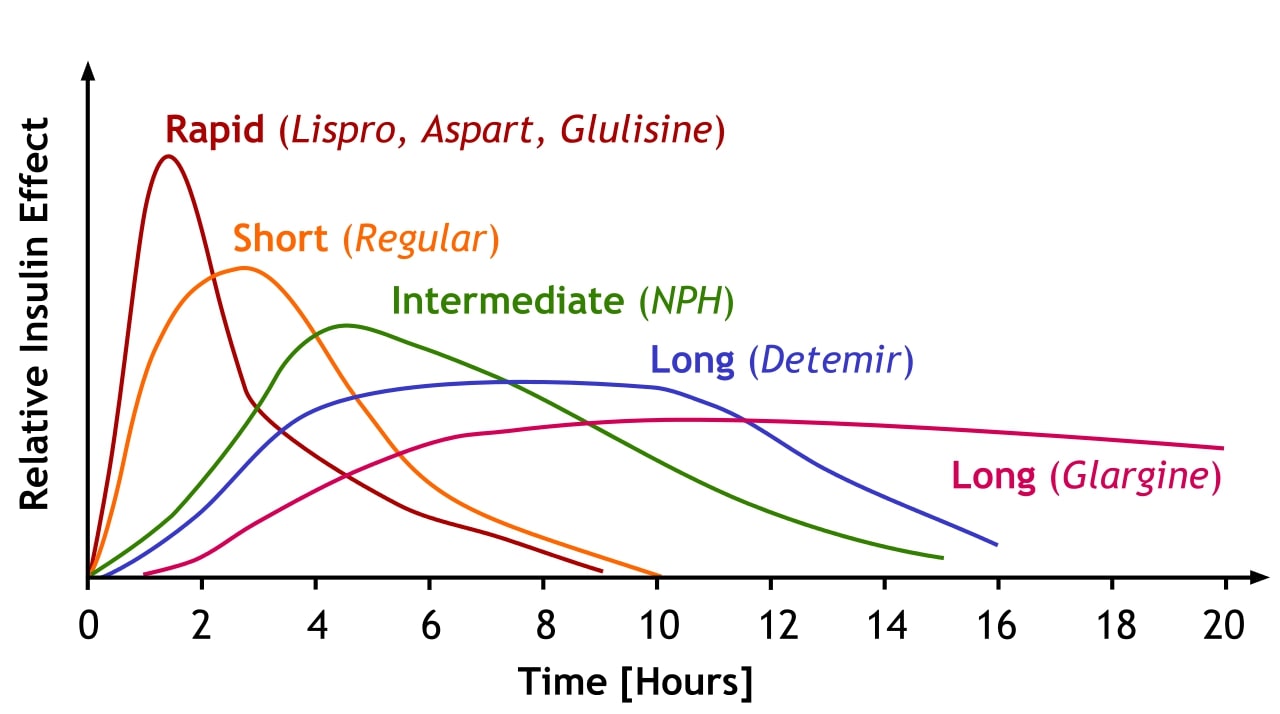
00:01 In this discussion, we'll talk about Insulin Dependent Diabetes Mellitus Type 2. 00:06 What we previously referred to as adult onset diabetes. 00:10 With the American obesity epidemic, we're seeing more and more of this in children. 00:15 So the definition of Type 2 Diabetes is a metabolic hyperglycemia resulting from increased insulin secretion and in the face of increased insulin resistance. 00:29 So two phenomenon: more secretion, more resistance. 00:33 The age of diagnosis of this problem is bimodal, where we're seeing more and more children between the age of 10 and 18 years developing the condition and then also we're seeing it in older people. 00:47 Generally, all of these people have a problem with excessive weight, although some do not. 00:54 So this has a prevalence of about currently 0.4% of children in the United States. 01:01 It is strongly associated with obesity. 01:04 All ethnicities have a rate of Type 2 Diabetes but some more than others. 01:10 So there is a genetic predisposition in addition to the environmental one that we see in this condition. 01:17 Females are 5 times more likely to have Type 2 Diabetes than males and 75% of diagnosed children have a first or second degree relative with Type 2 Diabetes. 01:32 So, the pathology of Type 2 Diabetes is complex and confusing and a little bit different than Type 1. 01:42 So I'd like to go through it carefully with you now. 01:44 The hallmark of this problem is a peripheral insulin resistance. 01:50 In other words, insulin at the level of the cell is not having a strong signal and telling that cell what to do as well. 01:58 This can be as a result of prolonged glucose exposure and high insulin exposure and these cells are downregulating their response or it can also be a result of training very early in life of how those insulin receptors will respond to the presence of insulin. 02:17 Nonetheless, what happens is with this decreased insulin response, one of those insulin receptors is found in the liver and so that liver is not seeing the negative feedback loop telling it to slow down in gluconeogenesis. 02:35 The liver continues to make more and more sugar and thus these patients will have a high glucose level. 02:43 There are other tissues involved, too, though. 02:46 The fat cells also will have less of an insulin response. 02:51 This causes less fat storage and more production of free floating fatty acids that are going through the blood. 02:59 These in turn, can cause damage and in particular, cause damage to the pancreas and as they damage the pancreas, they actually damage the pancreas's ability to secrete more insulin. 03:13 So you can see there's becoming a feedback loop where there's less insulin responsiveness but the damage is causing in the pancreas an inability to create more insulin to overcome that insulin resistance. 03:26 Simultaneously, muscle cells are also getting damaged and their less responsive nature to insulin is causing them to have more protein breakdown and more materials for which the liver can manufacture an inappropriate quantity of glucose. 03:43 So it's a combination of decreased insulin presence from the pancreas and a decreased insulin resistance. 03:50 All of these leads to hyperglycemia which is the hallmark of the disease. 03:55 So, risk factor for Type 2 Diabetes are obesity, ethnicity, a family history of Type 2 Diabetes. 04:04 Maternal gestational diabetes can cause a baby to be large for gestational age or LGA and those children are at risk for developing Type 2 Diabetes decades later. 04:18 So our children who have rapid weight gain in the first year of life and those typically are the premature infants or the small for gestational age babies. 04:28 This is really interesting because what it implies is that during that first year of life, children's insulin receptors are being somehow programmed in terms of how responsive they would be to insulin. 04:40 If they're exposed to excessive amounts of insulin, they're at increased risk for eventually developing Type 2 Diabetes far down the road. 04:48 So what are the signs and symptoms of a child who's presenting with early Type 2 Diabetes. 04:56 First off, because of the hyperglycemia, they will have the polys, an increased risk of urination because of the osmotic effect of the sugar and subsquently an increased thirst. 05:08 They may develop some weight loss. 05:11 This is from fat and protein catabolism that's happening. 05:15 These patients, remember, are overweight and they start experiencing some weight loss. 05:20 We may see acanthosis nigricans. 05:24 This is a heralding skin finding of the metabolic syndrome. 05:27 I'll show a picture a little bit later on in the talk. 05:30 If they present later in disease after a prolonged period of hyperglycemia, they have may have more substantial symptoms. 05:41 These can be irritability from the hypergylcemia. 05:44 Again, they can have polyuria but now in the phase of dehydration. 05:49 They may develop significant dehydration. 05:52 This can lead to altered mental status. 05:55 This can be confusing. 05:57 Remember, these are Type 2 Diabetes patients, not Type 1 Diabetes patients, but nonetheless, they can present in diabetic ketoacidosis. 06:07 This is because, remember, they're having pancreatic cell damage and they're making less insulin. 06:14 So they can totally present DKA and about a third of them will. 06:17 They also develop a problem that Type 1 Diabetes patients typically do not which is Hyperosmolar Hyperglycemic Syndrome or HHS. 06:28 This is a condition that's specific to Type 2 Diabetes. 06:34 Here's acanthosis nigricans. 06:36 This is a darkening of the skin that is seen typically over the back, in the armpits and perhaps between the two breasts which is commonly seen in patients with the metabolic syndrome or pre-diabetes. 06:50 How do we diagnose Type 2 Diabetes? First off, we can obtain a random glucose. 06:57 Any glucose level over 200 with signs or symptoms of Diabetes such as polyphagia and polyuria, you've made a diagnois. 07:06 If you wish, you could do a more formal glucose challenge with a fixed amount of glucose and then 2 hours later, obtain a glucose level. 07:14 If that glucose level is still high in patient where you're concerned about diabetes, it's entirely possible they have less insulin and less ability to take care of the glucose problem or alternatively, any glucose level in a fasting patient that's over 126 is abnormal especially if you find it on more than 2 samples. 07:36 Lastly, because these patients do present later on, you may simply measure a hemoglobin A1C and that will be already elevated, showing that this patient has for a long period of time been exposed to high levels of glucose in the blood. 07:50 How do we manage Type 2 Diabetes? First off and foremost, weight loss counseling and dietary help is indicated. 08:02 If patients can lose substantial amount of weight, their diabetes improves markedly. 08:08 The first choice in children is different than the first choice in adults. 08:14 Some of the medicines in adults aren't even certified for use in children. 08:19 So our first choice in children is metformin. 08:22 If patients aren't responsidng to metformin, we will move on to other therapies. 08:28 Metformin acts by increasing peripheral insulin sensitivity. 08:33 It also decreases hepatic glucose production again through improving the sensitivity of those insulin receptors. 08:41 If patients are more severe, we will move on to insulin as well especially if they are not producing enough insulin. 08:48 So, let's look carefully at the differences betweed diabetic ketoacidosis which we see in Type 1 Diabetes or Type 2 Diabetes and HHS which we see in Type 2 Diabetes. 09:04 Remember, both of these conditions can happen in these patients with Type 2. 09:08 In DKA, they have a shortage of insulin. 09:12 This causes an increase in their ketones and dehydration is common. 09:18 These patients need an insulin infusion 0.1 units/kilo/hour. 09:24 In HHS, they will develop severe dehydration and their high glucose levels will be very high often higher than in DKA. 09:34 However, these patients do not have ketones. Remember it's nonketotic. 09:40 This may be caused by an underlying infection or some other problem. 09:46 What's key to keep in mind with HHS is that it has a high mortality. 09:51 This is a very serious conditon and has to be maintained carefully. 09:55 So if you see a patient who has an altered mental status, is profoundly dehydrated and they have Type 2 Diabetes, it's the ketones or lack of ketones this is gonna driving how you're gonna manage this patient because you'll think of them as these two different presentations. 10:13 So let's review complications of Type 2 Diabetes. 10:18 We have acute complications, things that can happen right off the bat. 10:22 Examples are cerebral edema from diabetic ketoacidosis, HHS which can be life threatening or if they overtake their therapy, for instance, they start on their insulin and take too high of a dose, they may develop hypoglycemia and require resuscitation from that standpoint. 10:40 There are chronic complications that can happen as well and these typically don't happen until adulthood. 10:47 Examples include nephropathy or kidney damage, retinopathy or eye damage, extremity infections such as the diabetic foot and a peripheral neuropathy. 11:00 We don't need to track these children with this disease as carefully as adults do because these chronic complications usually happen over years of exposure to high sugar levels. 11:13 So we do not need to send a 12-year-old with diabetes to the eye doctor every year but certainly we would do that for the older patient. 11:23 So, management of Type 2 Diabetes. 11:27 There're several key things to remember. 11:29 Your prognosis depends directly on your glycemic control. 11:34 If you can get that patient on a weight loss diet and get their sugars under control, their long term prognosis is much better. 11:41 Follow their hemoglobin A1C to measure compliance to continue conversations with them about how they're doing. 11:49 We want to see a low hemoglobin A1C level at their check-up visits. 11:54 Weight loss is a huge part of therapy and should be encouraged. 11:59 Get them eating better and get them to the gym and in extreme cases, we may even consider weight loss surgery which is a newly developing field in adolescent medicine. 12:10 People are looking more and more towards bariatric surgery for certain categories of patients who fit very strict criteria for therapy. 12:19 That's all I have for you today about diabetes, Type 2 Diabetes in children. 12:24 There's another talk on Type 1 Diabetes which you can enjoy as well. 12:28 Thanks for your attention.
About the Lecture
The lecture Type 2 Diabetes (Adult Onset Diabetes) by Brian Alverson, MD is from the course Pediatric Endocrinology. It contains the following chapters:
- Pathology
- Signs & Symptoms
- Diagnosis
- Management - Part 1
- Differences between DKA (IDDM1) & HHNK (IDDM2)
- Complications of Type 2 Diabetes
- Management - Part 2
Included Quiz Questions
Which of the following is NOT true about hyperosmolar hyperglycemic syndrome?
- Patients are generally well hydrated
- Glucose levels can be over 1,000 mg/dl
- Ketone bodies are not produced
- The cause may be an underlying infection
- It has a high mortality rate
Which of the following is the hallmark of Type 2 diabetes?
- Peripheral insulin resistance
- Insulin deficiency
- Anti-insulin antibodies
- Weight loss
- Hyperlipidemia
Which of the following is NOT a risk factor for developing type 2 diabetes?
- Male gender
- Obesity
- Ethnicity
- Family history of type 2 Diabetes
- Rapid weight gain in the first year of life
Which of the following is the first line therapy for type 2 diabetes in children?
- Metformin
- Insulin
- Sulfonylureas
- Meglitinides
- Acarbose
Which of the following lab tests is most appropriate to monitor compliance with therapy in a patient with type 2 diabetes?
- HbA1c
- Monthly random blood glucose
- Home diary for everyday fasting glucose
- Biweekly Fasting glucose
- Oral glucose tolerance test every month
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
9 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Excellent lecture: complete, comprehensive, clear and highlights well the difference between: type 1 and type 2, DKA and HNNK and adult vs children
8 customer reviews without text
8 user review without text