Playlist
Show Playlist
Hide Playlist
Type 1 Diabetes (Juvenile Diabetes): Management
-
Slides Type1Diabetes Pediatrics.pdf
-
Download Lecture Overview
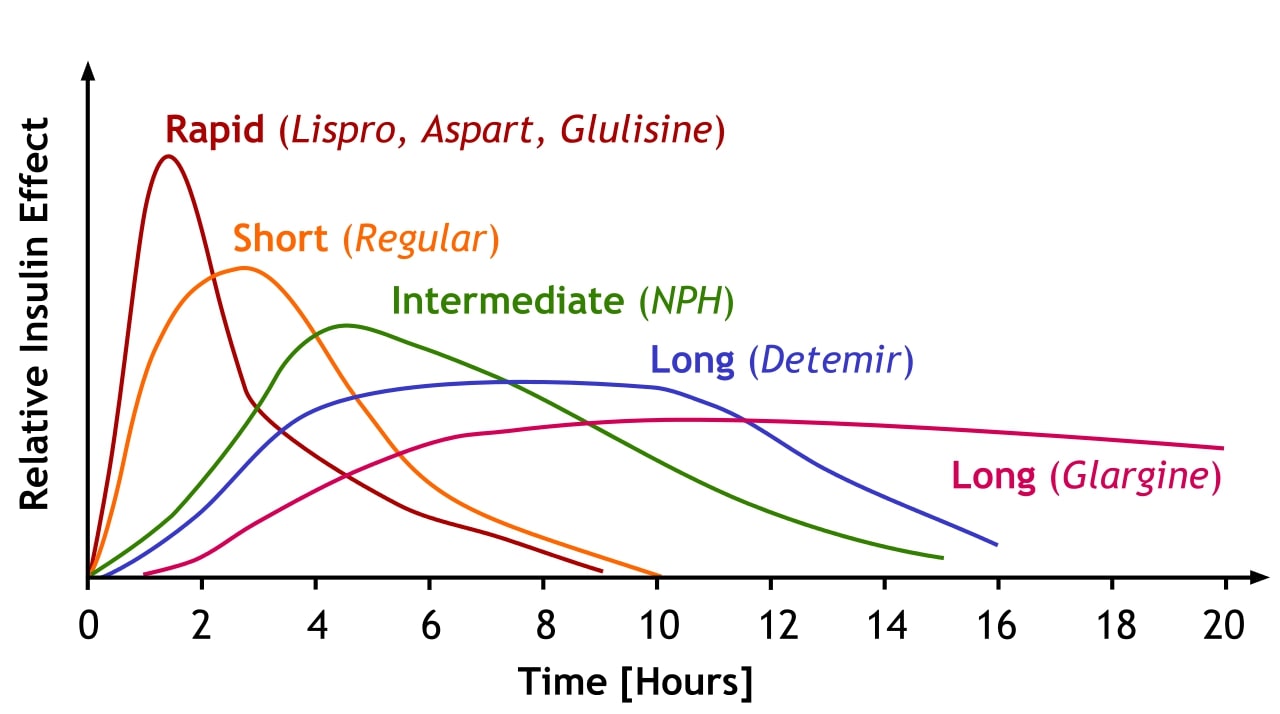
00:01 So, let's talk about management of diabetes. 00:05 DKA is a potentially life-threatening condition. 00:09 We need to worry about this. 00:12 Patients with DKA often require ICU level of care. 00:17 We're gonna admit these children to the ICU because we're gonna be needed to drawing their labs very frequently, hourly perhaps to make sure that we're correcting the sodium and the sugar and the potassium in the correct manner. 00:31 The key to the management of these patients is to provide insulin. 00:36 Typically, we'll start with an infusion of insulin at 0.1 units/kilo and we'll continue that infusion to drive down both glucose and to drive down ketones. 00:48 One area of confusion that happens often when we're first experiencing how we care for these patients is we encounter this circumstance where the ketones aren't gone but the glucose has come down. 01:00 You might be tempted to slow down the insulin because you're thinking, Oh no, this child is gonna develop hypoglycemia and it will seize, so we need to stop the insulin. 01:09 No, we're gonna continue the insulin no matter what because the problem is the ketones. 01:16 The hyperglycemia might be causing some additional dehydration but it's not typically causing horrible body wide problem like the ketones are. 01:26 So we continue the insulin but we increase the glucose that's going into this patient. 01:31 Sometimes, we'll have a 2-bag system where's there's D10 in one bag and D0 in another and then we can wire them together and thereby titrate exactly how much glucose is going in so that we can keep the glucose at a safe level while flooding this patient with the insulin necessary to get rid of their ketones. 01:53 So, when we manage this people, one problem is usually hydration. 01:59 Remember, these people, these children have had a lot of sugar in their blood and that sugar is spilling into the urine. 02:06 As a result, it's bringing fluid with it through osmotic forces and these children will become profoundly dehydrated. 02:16 So when we see them, we pretty much assume that they have 10% dehydration. 02:20 We assume profound dehydration. 02:23 We'll start off with normal saline and in particular, we're going to bolus them with normal saline 20 cc/kilo until they have stable vital signs. 02:34 That's key. We must first stabilize the vital signs. 02:38 Then we may notice, after they're stable that patients are often hyperosmolar. 02:45 A low osmolar fluid will result in rapid shifts into the brain and that can cause a sudden increase in cerebral pressures and your risk is worsening edema and death. 02:59 So we're gonna avoid hyperosmolar resuscitation fluid. 03:03 We're going to replace their deficit of their fluids slowly over 2 to 3 days to allow that brain to accommodate for their new, less osmolar situation. 03:17 They're gonna downregulate their idiogenic osmols in their cerebellum. 03:22 Again, when their sugar starts getting low, we'll start adding glucose to that infusion rather than reducing the insulin. 03:30 The insulin is the medicine they need to get rid of those ketones. 03:34 We sometimes add potassium when the levels are known to be safe and if the levels are less than 5. 03:41 Remember, it's a body deficit of potassium even if that potassium is high. 03:47 So, we wait but then we do often add potassium. 03:50 If the potassium falls below 2.5 as they're starting to recover from their acidosis, we're gonna treat it fairly aggressively. 03:59 Remember, acidosis causes a transient hyperkalemia through this cation exchange system but total potassium may be low. 04:09 We might also add phosphate because too much chloride isn't good either as it can contribute to acidosis. 04:16 Let's go over again how we adjust the sodium for hypoglycemia. 04:21 Remember, the body is going to maintain a particular osmol level that it likes. 04:27 So, if the sugar level is high, it's going to downregulate its sodium to adjust for an appropriate amount of osmols in the blood. 04:35 So we can expect that as we lower the sugar, that sodium is gonna come up essentially on its own. 04:42 We don't need to adjust fluid resuscitation for hyponatremia if a patient has a very high glucose and the sodium normally would be 140 which is the normal level for sodium. 04:56 Let's go through some examples. 04:57 We're going to add 1.6 to the sodium for every 100 that the glucose is above normal which is about a hundred. 05:05 So, if a patient has a measured glucose of 200, that's 100 above normal and we would expect their sodium to be 138.4 rather than 140. 05:16 We've adjusted it down 1.6. 05:19 So if you measure 138.4 and we add 1.6 to it, we get the actual sodium that we would expect to see once that sugar comes down. 05:28 Seems like not such a big deal perhaps for a measured glucose of 400. 05:33 We're now with 300 above normal, 3 times 1.6. 05:37 So if we measure something like 135.2, we would expect by adjusting for that, that their actual sodium once we fix the sugar will be 140 but let's say a child has a sugar of 1000. 05:53 We absolutely see this crazy high glucoses in patients with DKA. 05:58 Now, we're taking 9 times 1.6 so you can see, if I see patients with sodium with 125, I would say, wow, this kid has a really low sodium. 06:09 Not true, as that glucose is fixed, this child's sodium wil bounce right back up to the normal value of 140. 06:16 So, it's important to use that correction factor. 06:19 So, if we have a patient with DKA like I've said before, we're gonna start wih a continuous insulin infusion at 0.1 units/kilo/hour. 06:30 We're flooding this patient with insulin. 06:32 We're driving down those ketones because this is an emergency that can result in death. 06:37 If a patient doesn't have acidosis, but has high sugar levels and ketones, this is a milder form of the illness. 06:47 It does not require the insulin infusion because while they have ketones, there's not so many that they are in an acidotic state. 06:56 What we'll do is we'll provide insulin in regular, routine, every-couple-hour doses and once there's a resolution of the ketosis, we'll then switch to a standard typical system of taking care of them as they're healthy. 07:14 So, we start off in DKA. We're giving an infusion. Their acidosis improves. 07:20 Now, they probably can be transitioned to the general wards instead of the ICU setting and we're switching to every-2-hour insulin and frequent d-stick checks. 07:30 Then, as now both the dextrose and the ketones improve, where the ketones are gone from the urine, and the child's sugars are normal. 07:39 We're gonna put the child on a combination of short and long-acting forms of insulin and the regimens that people choose vary a lot from provider to provider. 07:50 So I won't go into a specific regimens, but often people use a long form acting of insulin like NPH as well as short-acting like Humalog, sometimes with large meals and you can adjust for the number of calories. 08:05 Keep in mind for a first-time-diagnosis patient, there is going to be this phenomenon called the 'Honeymoon'. 08:12 The 'honeymoon' happens as that pancreas is finally in its last gasp going to give a little bit more insulin. 08:21 This means that the patient may look like they're cured. 08:24 Their need for insulin will disappear. 08:27 This can happen for several months afterwards. 08:29 Families need to be warned about this because if they unpresume that this was a mistake on behalf of the health professional and they don't pay attention and continue to follow up with their endocrinologist, that child could go right back into DKA again the next time and the next time, the outcome might not be so good. 08:49 So, here's an example of our short-acting/long-acting regimen. 08:55 Here's a child who's getting 3 times a day short-acting boluses and then a long-acting one at night. 09:04 This would be a classic example. 09:06 We would say, take a dose just before breakfast, just before lunch and just before dinner. 09:11 Some people like a snack dose. 09:13 It doesn't matter so much which kind they're going to do. 09:16 Generally, we'll do the long-acting one in the evening to help them through their sleep so they're maintaining a basal level of insulin as they sleep. 09:24 Another alternative that's becoming more popular is the pump. 09:29 The basal pump is a pump that's implanted. 09:33 And has a reservoir of insulin in it. 09:36 Paitients can check their sugars and can actually dial up and down their pump. 09:41 This is usually reserved for patients who really sort of understand their diabetes and have figured out what's going on and again, there's a lot of variation among both practitioners and individuals as to what system works best for them. 09:54 The basal pump will provide a nice basal rate while they may use boluses for when they have a meal at breakfast, lunch, dinner or snack. 10:04 So, let's focus on the complications of diabetes. 10:10 Acutely, we can cause cerebral edema if we don't get on this DKA setting quickly and treat it aggressively. 10:20 Cerebral edema can cause brain damage and can result in chronic disability or death. 10:26 Patients can have hypokalemia from having body loss of potassium and acutely, if we're treating their diabetes and we use too much insulin, we can actually cause hypoglycemia. 10:39 Diabetics will tell you that when they take too much insulin, they feel like a craving for sugar. 10:45 They feel jittery and they take a quick beverage. 10:48 Chronically, patients can have complications as a result of being on insulin for long period of time. 10:57 We tend not to see this in children. 11:00 We tend to see this more commonly in adults. 11:03 This can happen because of repeated episodes of DKA so especially in adolescents, maintaining control of their diabetes and remembering to be responsible is very important. 11:15 Patients can develop diabetes nephritis and eventually can result in renal failure. 11:20 Patients may develop a retinopathy over a long period of time and develop blindness as adults. 11:27 Adults may get extremity infections especially with pseudomonas. 11:32 This can result in amputations of extremities and feet. 11:36 I'm sure you've all seen when taking care of adults, the diabetic foot. 11:41 It's a real problem. 11:42 None of these things, though, typically happen in children. 11:46 You won't expect to see it in you pediatric endocrine clinic and don't forget about peripheral neuropathy that can be a real problem as well. 11:55 So that's all I have to talk to you today about diabetes especially type 1 diabetes. 12:02 We'll talk about type 2 diabetes in another lecture. 12:06 Thanks for your attention.
About the Lecture
The lecture Type 1 Diabetes (Juvenile Diabetes): Management by Brian Alverson, MD is from the course Pediatric Endocrinology. It contains the following chapters:
- Management
- Fluids
- Insulin
- Complications of Diabetes
Included Quiz Questions
A 12-year-old girl is diagnosed with Type 1 Diabetes Mellitus and started on insulin. Two months later, her parents state they’ve stopped the insulin, and her sugars are normal. What is the most likely cause of her not needing any more insulin?
- Honeymoon period
- Incorrect diagnosis
- Medicine is long-acting
- Medicine is over-concentrated
- The patient is not clearing medicine from blood.
A patient with DKA was started on continuous intravenous insulin. The patient’s glucose fell from 1,000 mg/dl to 100 mg/dl. The child is still acidotic and is passing ketones in the urine. You are concerned that if you continue the same therapy the child may become hypoglycemic. What is the best next step?
- Add dextrose to the IV fluids
- Reduce the insulin infusion rate
- Stop the insulin and give dextrose immediately
- Start intravenous lipids
- Discontinue all care and wait and watch
A patient with diabetic ketoacidosis has a measured serum sodium level of 138.4 mEq/dl and a blood glucose level of 200. What is his corrected serum sodium level?
- 140 mEq/dl
- 138.4 mEq/dl
- 148.4 mEq/dl
- Can not be determined
- 158.5 mEq/dl
Which of the following is an indication to switch from intravenous insulin to subcutaneous insulin during the management of a patient with DKA?
- Resolution of ketosis
- Fall of blood glucose level below 180 mg/dl
- Serum pH < 7.4
- Once when Kussmaul breathing has resolved
- There is no specific indication for this switch
Patients with DKA are started on normal saline infusion even though they are hyperosmolar. Which of the following is a possible complication of starting these patients on hypoosmolar fluid?
- Cerebral edema and death
- Loss of excessive fluid via urine
- Pontine myelinolysis
- Both isotonic and hypotonic fluids can be used without complication
- Acidosis may worsen
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
3 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Best DM1 lecture I have ever seen! Thank you so much Dr Alverson!!
Excellent lecture, the features of the disease are well summarised. Thanks!
Nice lecture! It is actually helping me a lot! Best Regards from UFMT-Sinop Med School, Turma 5