Playlist
Show Playlist
Hide Playlist
Toxic Myopathies with Case
-
Slides Toxic Myopathies.pdf
-
Download Lecture Overview
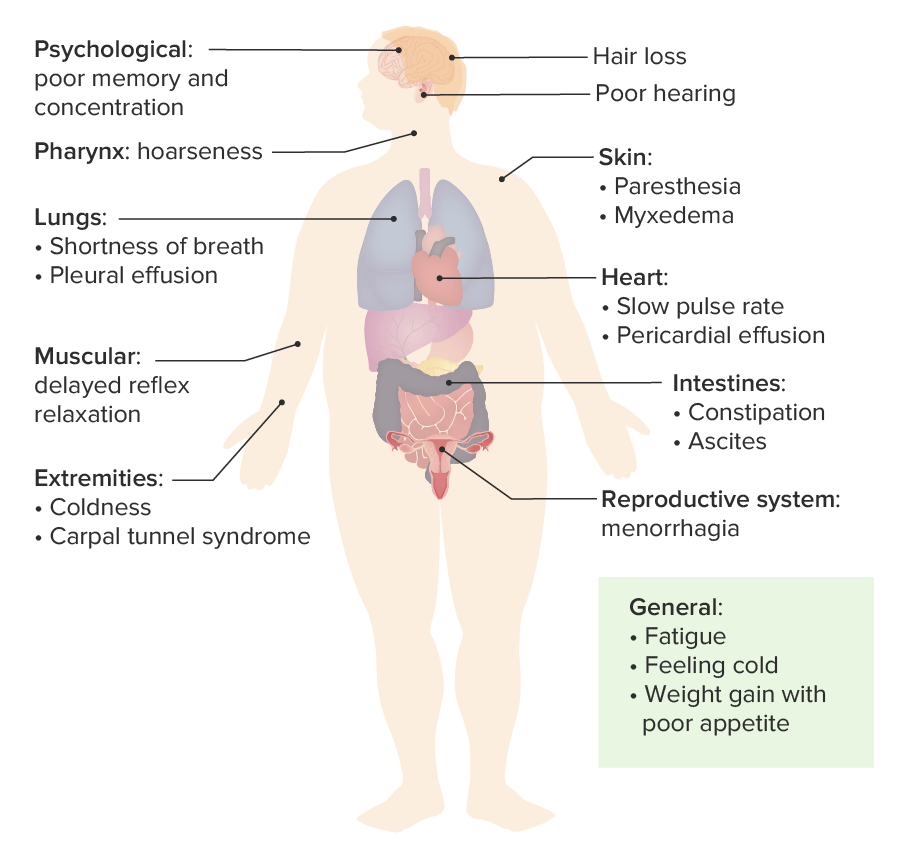
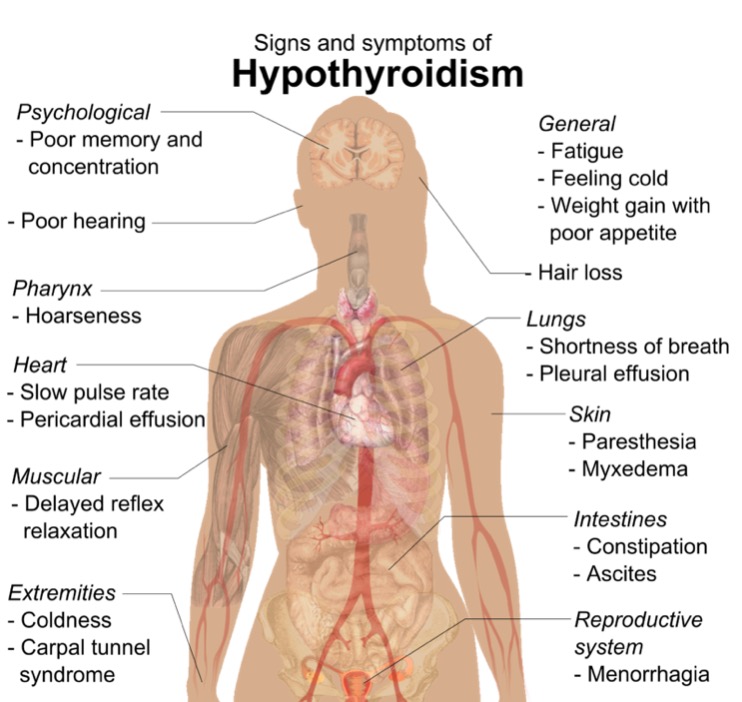
00:00 In this lecture, we're going to talk about toxic myopathies; toxic, metabolic or nutritional conditions that affect the muscle. This is one of the most vast and complex muscle disorder topics, but we're going to break it down to about 5 toxic myopathies that I'd like for you to know. So let's start with a case. And this is the same case that we have seen with some of the other muscle disorder lectures. As you recall, this is a 54-year-old female who presents with weakness, new onset evaluation of weakness. This person has been a long-time patient and has a history of thyroid disease treated with levothyroxine, hyperlipidemia managed with atorvastatin. For the past 2 months, the patient has noticed progressive weakness. This is most prominent in the legs where the patient now has difficulty arising out of the chair in the morning after breakfast and has had to use arms to help walk up the stairs at times. More recently, the patient has noticed difficulty with arm strength as well. There are no sensory complaints and the patient denies bulbar symptoms. No ptosis, diplopia, dysarthia, or dysphasia. On exam, we see proximal weakness in the legs, that proximal distribution that points towards muscle, and normal deep tendon reflexes. So we've asked before "What's the diagnosis?" And we focused on distribution, sensory findings, and the reflex exam. As you recall, the distribution here is proximal. Proximal symptoms, proximal exam, this proximal pattern points us to a muscle disorder. There are no sensory findings and the reflexes are normal, and this is the signature that points towards muscle pathology. Furthermore, we have this wild card. The patient has no bulbar symptoms. There is not ptosis, diplopia, dysarthria, or dysphasia and those things would point us towards a neuromuscular junction pathology. 01:54 There are also some other important clinical features that we'll talk about in this lecture. This is a 54-year-old female. She has a history of thyroid disease. She is on a statin medicine, and this is progressive weakness over the course of 2 months. So let's go back to the workup. 02:10 And this is a different workup than we have seen in this case previously. Here, we see that this patient has a mildly elevated CK at 400 with normal being 50 to 160. Thyroid testing is performed to evaluate the status of the thyroid disease and we see the TSH is dramatically elevated, 117 when the upper limit of normal is 4.5. And we also look at the free T4 which is low, 0.3, the normal is 0.6 to 1.4. This signature of elevated TSH and low free T4 indicates prominent hypothyroidism. And remember this is different from the case that we saw in the inflammatory myopathy lecture. There we saw significantly elevated CK in the thousands, and here it's only in the hundreds. And we didn't see thyroid studies abnormality. So what's the diagnosis? Is this dermatomyositis, hypothyroid myopathy, inclusion body myositis, or polymyositis? Well, we don't like dermatomyositis, there is no rash and we learned that rash is a characteristic finding in dermatomyositis and we don't see that here. We don't like inclusion body myositis. Inclusion body myositis presents with proximal lower extremity weakness but distal upper extremity weakness, and we don't have that pattern for this patient. What about polymyositis? We don't like polymyositis. In PM, we learned that the CK is substantially elevated into the thousands and we shouldn't see another cause of myopathy like abnormal thyroid function studies. So this is a classic presentation of hypothyroid myopathy. The patient has active hypothyroidism which strongly favors hypothyroid myopathy or the potential for that, the CK is mildly elevated and we learned that with most toxic myopathies, CKs are not elevated. There is not inflammation. But hypothyroidism is an exemption and we see mildly elevated CKs which is an important caveat to recognize in this case. And the patient has no rash to suggest dermatomyositis. So let's focus on some of the toxic myopathies. And again, this is a large group of conditions that we're going to break down to 5 key diagnoses that I'd like for you to know. The first is thyroid myopathy, like the case that we just reviewed and we'll talk more about hypo- and hyperthyroid myopathy. Steroid myopathy is common and you got to know this one. We'll see it in patients, we'll learn it on vignettes. This is a critical type of toxic myopathy. Statin myopathy is important. It's a cause of a toxin-mediated myopathy and can precipitate an autoimmune necrotizing myopathy and so something we should focus on in greater detail. And then lastly, critical illness myopathy and myopathies caused by medication. And there is going to be a big list of medicines that can cause problems with the muscle and we'll review that.
About the Lecture
The lecture Toxic Myopathies with Case by Roy Strowd, MD is from the course Acquired Neuromuscular Diseases.
Included Quiz Questions
With the exception of hypothyroid myopathy, a toxic myopathy typically has ..?
- ...a normal creatine kinase level.
- ...an abrupt onset.
- ...bulbar involvement.
- ...asymmetric muscle weakness.
- ...a high erythrocyte sedimentation rate.
Which of the following clinical manifestations is consistent with hypothyroid myopathy?
- Proximal muscle weakness
- Burning sensation in a “stocking and glove” distribution
- Exaggerated knee reflex
- Skin rash
- Inflammatory arthritis
Which of the following may be a trigger for autoimmune necrotizing myositis?
- Statin medications
- Corticosteroids
- Hyperthyroidism
- Critical illness
- Trichinellosis
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
I like how you emphasize the key points; it makes it easy to learn.