Playlist
Show Playlist
Hide Playlist
Special Analgesics – Pathophysiology of Pain
-
15 -The Pathophysiology of pain.pdf
-
Download Lecture Overview
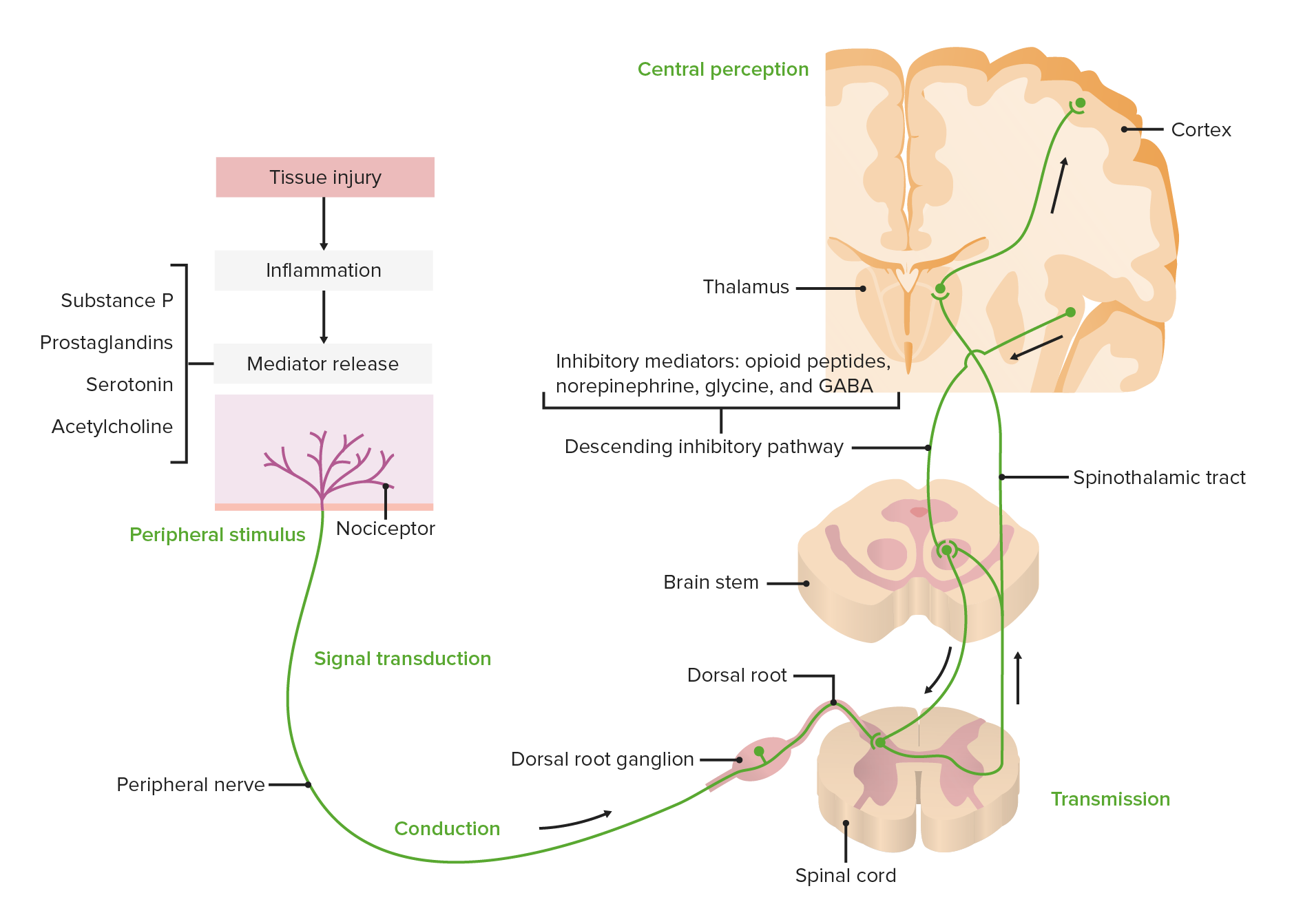
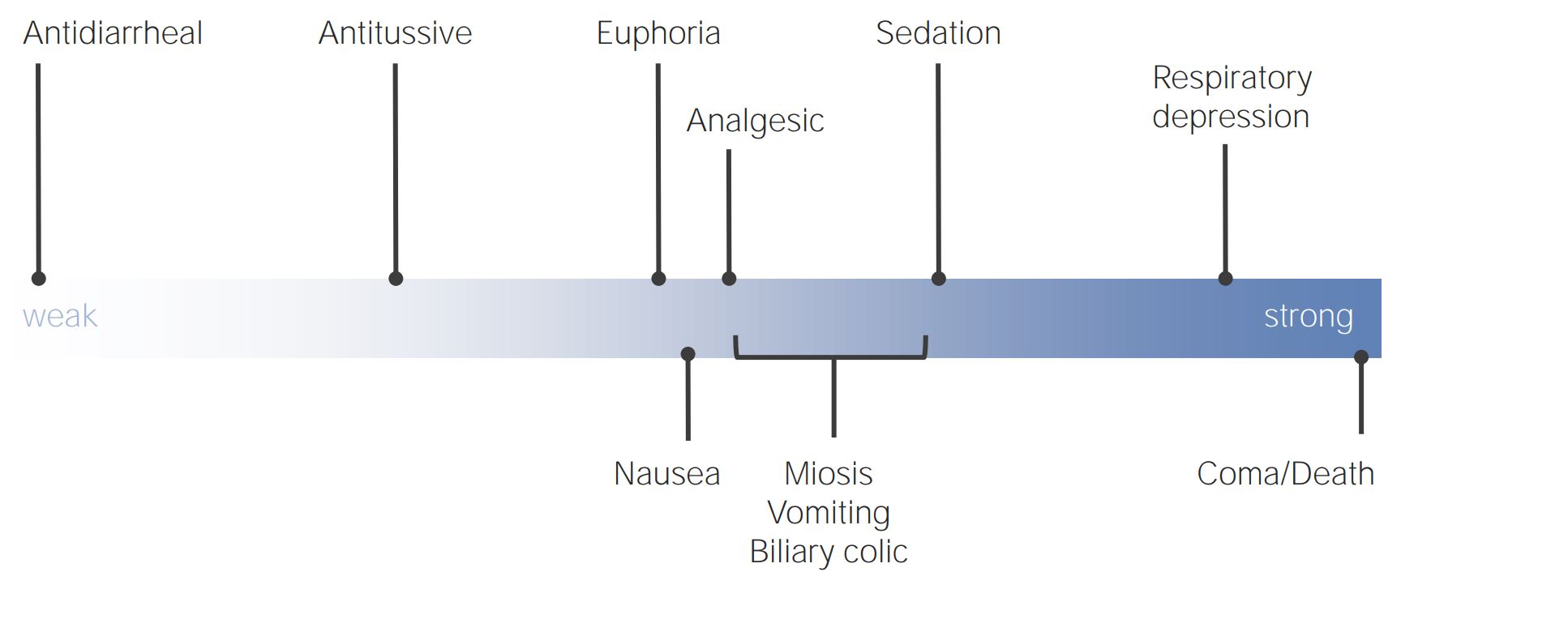
00:00 effect on pain perception, and we'll get to that in a few minutes. There are a great number of analgesics that are used in the management of chronic pain. 00:06 We've talked already at some length about the opiates, and they're basically either drugs from natural sources such as from opium plant, from the opium poppy, or they're opioids themselves, are manufactured drugs. It doesn't matter which they are, they act exactly the same way and I'm going to use the two words interchangeably as I already have in this lecture series, but I'll continue to do so because, quite honestly, I can never remember which is an opiate and which is an opioid, and it makes no difference in terms of the patient's condition in any case. Our brain has opioid receptors, as does the spinal cord. These are mu receptors, delta receptors, and kappa receptors. But the most important one is the mu receptor. And the mu receptor is both responsible for moderation of pain and response to pain, but it's also the receptor that creates all the side effects that we see with opiates. 01:06 So, what opioids and opiates do, is they change the brain's response to pain. And it's interesting, if you talk to somebody who takes opiates, they often still feel the pain, but it doesn't bother them very much. And that's because their brain's been told to ignore the pain. 01:24 So the pain in terms of transmission traffic may continue to be a very high volume situation, but the brain doesn't respond as much. So it starts to ignore the pain and that's what opioids do. In the brainstem, opioids stimulate release of inhibitory signals, so this is part of that modulation process I mentioned. And this occurs also in the spinal cord and through what's called the primary afferent nerve, which is that first nerve that goes up to the brain, there are actually synapses along its route, where inhibitory signals come in and kind of tune down the excitement. 02:06 Opioids also work to some degree at peripheral sites and reduce the response to pain. So, I classified pain in three ways. And that's not the typical way of doing it. Most textbooks and the pain societies classify pain as either acute or chronic. And we've already talked about acute pain, this is severe but usually managed with opioids, non-steroidals, over-the-counter medications from your local pharmacy, local anesthetics. This is what surgical pain is generally all about. Usually doesn't last for extended periods of time, certainly less than three months in most cases. And it's usually effectively managed by an anesthesiologist acute pain service. Chronic pain is longer lasting, greater than 3 to 6 months. It's difficult to treat. It's very difficult to treat! And it's associated with personality changes in patients and sometimes associated with drug seeking in patients. 03:06 The other category that I've kind of created for myself doesn't have a clear definition, but I think it's a very real situation. 03:18 And this is the Transitional Pain, which occurs when acute pain isn't fully managed and it remains for a fairly extended period of time and it transitions into chronic pain. And we know this actually exists and we know that if patients are in this phase, and this phase can be days, hours, or perhaps even minutes, if we treat aggressively at that stage, we may be able to prevent the patient developing chronic pain. 03:48 One of the worst forms of chronic pain is
About the Lecture
The lecture Special Analgesics – Pathophysiology of Pain by Brian Warriner, MD, FRCPC is from the course Pathophysiology of Pain.
Included Quiz Questions
Which description applies to opioids/opiates?
- Act upon nervous tissue in the brain, brainstem, spinal cord, and periphery
- Always produce addiction if used for extended periods
- Are the first-line treatment for chronic pain
- Produce dependence in 10% of patients who receive them for extended periods
Which receptor is responsible for the moderation of pain?
- Mu
- Delta
- Kappa
- Alpha
- Beta
What is the effect of opiates/opioids in the brainstem in the management of pain?
- They stimulate the release of inhibitory signals.
- They alter mood in response to pain.
- They inhibit primary afferent activity.
- They inhibit afferent response.
- They counteract noxious stimuli.
What is the duration for pain that is defined as acute pain?
- Less than 3 months
- Less than 2 weeks
- Less than 1 month
- Less than 6 weeks
- 3–6 months
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
This lecture was informative and engaging. The speaker did an excellent job of presenting the material in a clear and concise manner, making it easy to understand.