Playlist
Show Playlist
Hide Playlist
Sinus, Atrial and Ventricular Rhythm – Cardiac Dysrhythmia
-
13 Lecturio Cardiac dysrhythmias.pdf
-
Reference List Cardiology.pdf
-
Download Lecture Overview
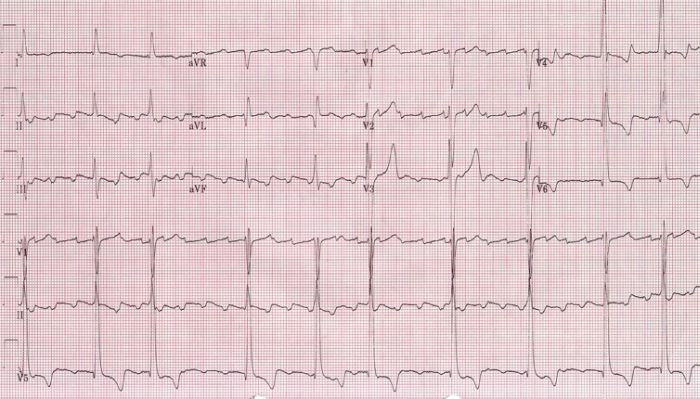
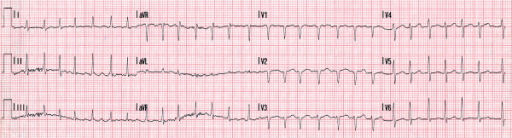
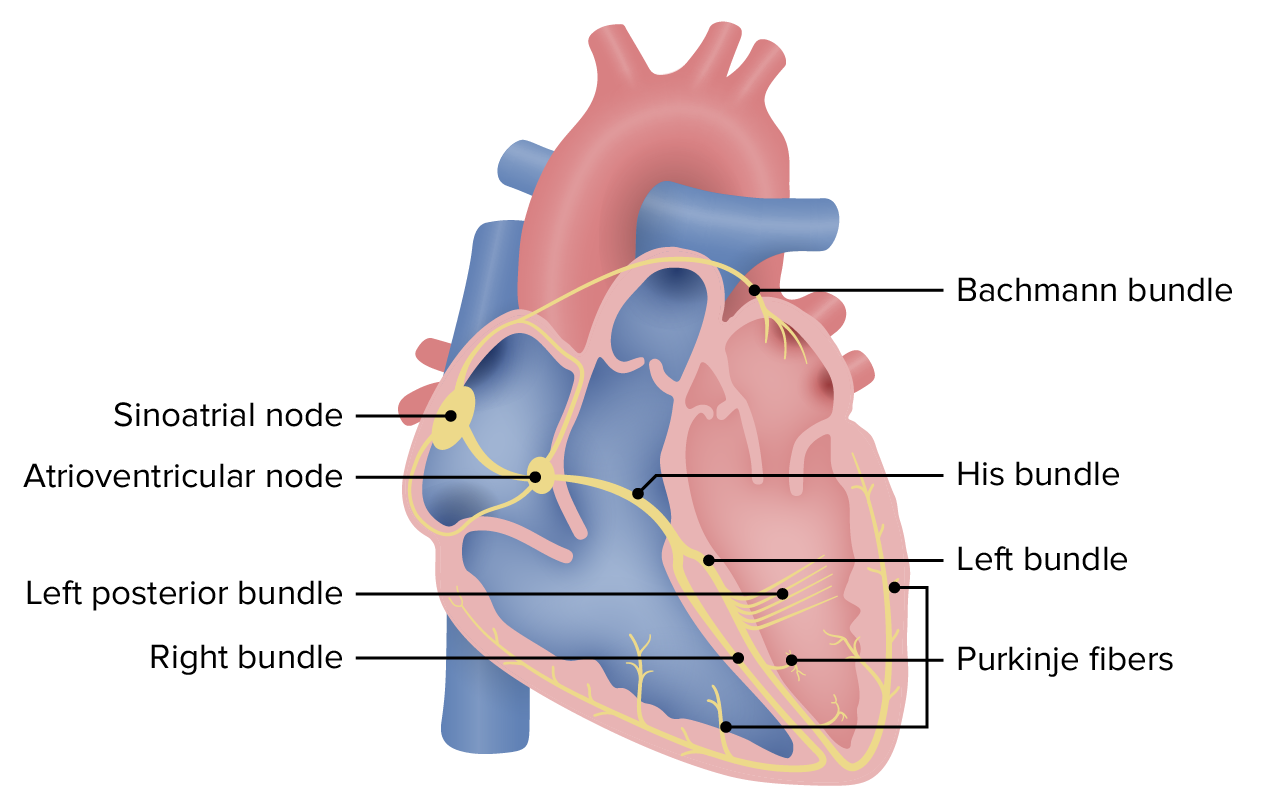
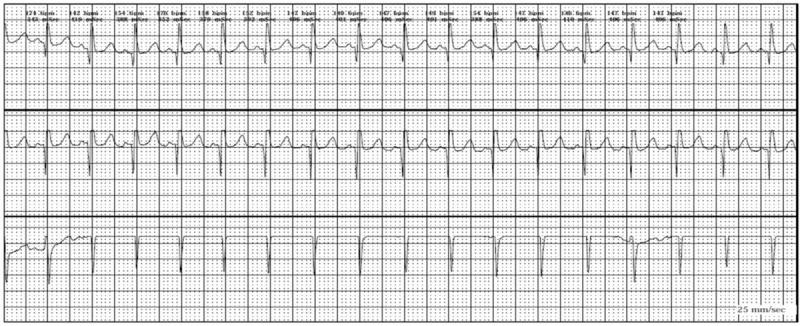
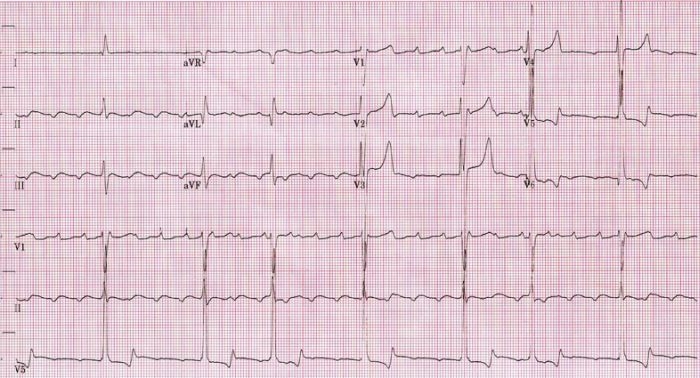
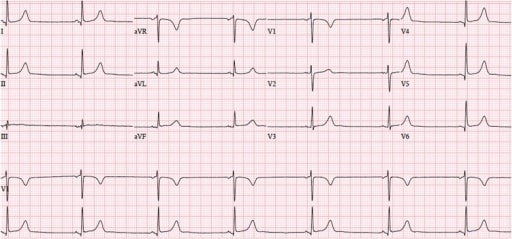
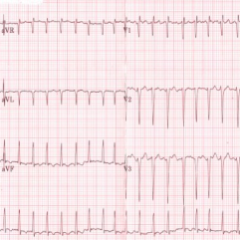
00:00 Right. Let’s look at each part of these in greater detail, particularly with respect to arrhythmias or dysrhythmias. Here is normal sinus rhythm. This is the normal rhythm. Let’s take a look at it in greater detail. You can see a small P wave - atrial depolarization, followed by a normal QRS, followed by a normal upright T wave. The P wave is upright, the T wave is upright and the QRS is upright. This is a typical monitor lead of a patient in normal sinus rhythm. Normal sinus rhythm consists of a rate between 60 and 100 beats per minute. 00:37 So, this is normal sinus rhythm. Okay! Here is sinus bradycardia. Remember from a previous lecture, “bradycardia” means slow, “brady” means “slow” in Greek. So, what we're seeing here is a sinus rhythm P wave QRS T wave, P wave QRS T wave, but the rate is slow. 00:59 The rate here is down in the 50s and in fact, it’s less than 60, so we call this sinus bradycardia. This is very common in athletes. Trained athletes frequently demonstrate sinus bradycardia at rest so that this can be a totally normal rhythm. Here's sinus tachycardia. 01:19 Notice it’s a little harder to see the P wave, but you can see a P wave in front of each QRS followed by a T wave and the rate here is quite fast, it’s about 120. Well, when does this occur? Well, when we put people on a treadmill and exercise them, when you run up a flight of stairs, you're going to have sinus tachycardia. The autonomic nervous system in the brain is saying to the heart, “Speed up, we need to pump a little more blood, we're running up the stairs.” And so, sinus tachycardia occurs. It is normal when it is in response to an increase in activity where there is a need for increased cardiac output. Anything over a heart rate of 100 per minute is considered sinus tachycardia, when we see the P waves when the sinus node is there and abnormal P waves are there. Now, occasionally, the sinus node falls asleep, often in older individuals where there's been a little scarring in the node or sometimes it goes completely to sleep. There's not just a pause, but there's a complete absence of sinus node activity. Well, you can see here's an example. Notice the first beat on the left T wave, QRS and T, next beat P wave, QRS and T, next, ooh, where is the next beat? Suddenly, there's a pause and then suddenly, the rhythm picks up again in the final two beats, P QRS and T, P QRS and T. There was a pause here. If we see long periods like this, like the pause in the middle then it’s a sinus arrest means a deceased sinus node and if it sometimes caused by drugs, we take away the offending drug. If not, the patient often needs a pacemaker. Why? Because the slow heart rate is associated with low cardiac output, which will lower blood pressure and make people feel badly. They'll be fatigued, they may even be lightheaded and might even faint. Here's another arrhythmia, these are extra beats. What we saw on the last strip was an absent beat. What we're seeing on this strip is extra beats. Youll notice that the rhythm is in twos. The first beat is a normal P QRS and T followed by what looks like might be a funny looking P wave and an early beat and then we go back to the normal beat P QRS and T, oh, and another funny looking beat and then we go back to the normal beat, oh, and another funny looking beat. So, these are atrial premature beats. This is also called bigeminy, bigeminy meaning two. That means every other beat is abnormal. These are atrial premature beats. How do I know they're atrial premature beats? Because the QRS is in the normal direction and I see what looks like a funny looking P wave in front. There's an abnormal focus in the atria that’s firing off every other beat. What this tells me is that there were some electrical instability in the atrium and these patients are at high risk for developing further electrical arrhythmias in the atrium. For example, atrial fibrillation, which we talked about when we talked about its tendency to form clots and the need for anticoagulant drugs. I'm going to show you some examples of atrial fibrillation in a moment. 04:24 Now, what we have here is exactly that - atrial fibrillation. First of all, look at the rhythm strip and see if you can see any P waves. I don’t see any P waves and then look at the QRSs, the QRSs look normal, but in fact, they're quite irregular. There's longer periods and shorter periods, it’s complete random. Remember I gave you an example of normal sinus rhythm? It goes “pom, pom, pom, pom, pom,” but atrial fibrillation goes “pom pubb, pom pubb, pubba pubba pom pom, pom pubba pubba pubba pom”. It’s completely random. Why is that? There are 600 impulses per second bombarding the atrio- ventricular node, the AV node and obviously, they keep bumping into one another. It’s like too many cars trying to get through a tunnel through the mountain, lot of them crash into each other and never make it through the tunnel, but the ones that get through the tunnel, get through randomly. So, atrial fibrillation is chaotic atrial activity in the atria bombarding the AV node with 600 impulses per minute and only a certain number get through. In fact, often quite a few get through and patients may have heart rates of 140, 150, 160. 05:40 This often makes them feel quite uncomfortable, particularly if they have heart disease, this rapid heart rate may stress the heart frequently. Patients like this come to the emergency room, this is the commonest arrhythmia that leads to hospitalization, we see it every single day. 10% of people over age 80 have atrial fibrillation, I mentioned that in an earlier lecture. And in fact, there is excellent treatment both in terms of drugs and also, in terms of electrical ablation or destruction of the area of the atrium with a burning catheter that initiates the atrial fib and often we can control this arrhythmia quite well. We'll talk a little more about that later on as we talk more about atrial fib. 06:27 Here's a first cousin of atrial fib. This is atrial flutter and you can see the sawtooth movement there, we call that sawtoothing atrial flutter. What’s happening there is instead of chaotic atrial activity going on in the atrium, there is actually, what we call a circus movement, in which the electrical impulses zooming around the atrium at a rate of about 300 per minute with every... often every other beat getting through. The first 1 2 3 4 5 6 beats, it’s every other beat getting through and then you see a period where it’s every 5th beat gets through when the period slows down and we're able to see the flutter waves in the background. Look, when a pa-… when somebody shows you electrocardiogram and the rate is fast, always look for that sawtoothing because that says atrial flutter. It’s a first cousin of atrial fib, often this degenerates into atrial fibrillation. 07:22 This slide shows a first cousin of atrial flutter. This is atrial tachycardia. Why is it called the first cousin of atrial flutter? Because the same thing is happening in the atrium. There's a circus movement. Just like the horse at the circus going around and around in a ring, you have an electrical activity going in the atria around and around and around. 07:42 The difference from atrial flutter is that an atrial flutter rate is usually very clearly determined, the flutter waves move around the atria in a rate of 150 per minute and usually every 1st or 2nd or 3rd beat gets through. If every 1st beat gets through, the ventricular rate is 300. That’s actually a very dangerous situation because ventricular fibrillation can occur. The most common situation is when every other flutter wave gets a beat into the ventricle, that’s a rate of 150 because the flutter is going 300 and the rate is 150 when every other beat gets through. If every 3rd beat gets through, the heart rate is 100, if every 4th beat gets through, the heart rate is 75. With atrial tachycardia, it’s often due to a little subsidiary pacemaker in the atrium and the rate can be anything, but again, you have a circus movement. So, the rate could be 150, but it could be 180, could be 140, could be 190. It’s variable, it’s not like atrial flutter where there's usually a very clearly determined rate in multiples of 300. You can see it’s atrial because the QRS is narrow and it looks like there is a funny looking P wave in front of each one, although sometimes, you can’t see the P wave in atrial tachycardia. 08:59 So, here is an electrocardiogram. So, what’s the rhythm here? If you look you'll see, first of all, the rhythm is quite regular, the rate is about 150 and if you look carefully, you'll see the sawtoothing. This is a patient with atrial flutter, the flutter waves are going 300 a minute, around the atrium 300 a minute and every other one is getting through the AV node, so the ventricular rate is 150. Notice that the QRS is narrow, that tells you that this is a supraventricular or an atrial arrhythmia. 09:30 All right. Let’s go on and talk about ventricular arrhythmias. Now, the ventricular arrhythmias have a different morphology, a different shape from the normal beat. Why? Because they're often coming from down in the ventricle and they're often going backwards. So, you can see here, the first three beats are sinus beats, P wave followed by QRS, P wave followed by QRS, P wave followed by QRS, oh, suddenly the 4th beat is abnormal. It’s completely different in its shape from the normal sinus beat. The QRS can be upright or it can be down, but almost always the T wave is going in the opposite direction from the QRS; you'll notice that the T wave is inverted there, it’s going downward. So, and often the QRS, in a ventricular premature beat, is slightly widened, wider than the normal beat. And you see now, sinus rhythm is then restored in the next three beats, oh, and there's another premature ventricular contraction, finally known as a PVC or a VPB, ventricular premature contraction. These are exceedingly common as we get older. Almost all of us will have some of these and they're usually benign. They're not benign when they come in a long string called ventricular tachycardia that is a ventricular rapid heartbeat because that can degenerate into ventricular fibrillation. And here is an example of ventricular tachycardia. 11:04 You'll notice that the QRS is wide, you don’t see any P waves and there's one P wave there in the middle that is not doing anything because the rhythm is being carried by the ventricular tachycardia. The rate is very fast, it’s about 180-200 and this can degenerate into ventricular fibrillation which is cardiac arrest. I think it’s time for a little quiz. So, what is the rhythm here? Do you see a P wave in front of each QRS? I do. Do you see a narrow QRS? I do. Do you see a normal upright T wave after each QRS? Again, I do. What’s the rate? The rate is about 65. This is normal sinus rhythm at a rate of 65. Remember, I showed you this right in the very beginning. 11:55 All right. Let’s look at a very abnormal rhythm. This is ventricular fibrillation. 12:00 This is cardiac arrest. You'll notice there's no organization here, the rhythm is all over the place. Remember that atrial fibrillation is the same thing, but it’s relatively benign. 12:12 On the other hand, ventricular fibrillation is not benign. Why? Because when the ventricle fibrillates, it doesn’t contract, the blood pressure goes to zero, the brain is deprived of its blood supply and brain cells start to die within 4 to 5 minutes and if a longer period of time goes, a lot of brain cells die and the situation can become irreversible. 12:35 The heart can be resuscitated within 10 or 15 minutes of even no heart activity, but often during that period of time, the brain is so damaged that the patient doesn’t survive. 12:46 That’s the reason why if you see somebody go down, you need to think, “Is this person having a cardiac arrest or did they just faint? Can you feel a pulse? Can you listen with your head to the chest? Can you hear a heartbeat?” If you can't, you need to start compression, CPR, cardiopulmonary resuscitation and if there's an automatic external defibrillator around, you need to get that and shock the patient. If there isn’t one, you need to call for emergency technical ambulance service to come with a defibrillator and defibrillate the patient. In the meanwhile, you have to continue cardiac compression. That’s a whole other topic that we could cover at another time, but resuscitation is very important. 13:33 As the community has geared up, many of these patients survive because there are automatic external defibrillators in sports arenas, in schools and so forth. And also, many people know how to do CPR so they can maintain the heart function until the emergency medical technicians arrive with a device to shock the heart back to sinus rhythm. 13:55 There are a variety of conditions where the electrical impulse starting in the atria fails to get through to the ventricle. This is because the AV node is subject particularly at advanced stages to fibrosis to scarring and even to calcification. And as that condition develops, fewer and fewer beats get through to the ventricle. Now, the ventricle has its own pacemakers that takeover, but they takeover at a very very slow rate. In the beginning, there may be just a little lengthening of the PR interval and we call that First-degree AV block, but as time goes along, you can see the pauses get bigger. We have Second-degree AV block of two types, a milder form and a more serious form and then finally, we get the Third-degree AV block where the ventricle is using its own pacemaker at a very slow rate and none of the atrial impulses are getting through. You can imagine with a ventricular rate of 20 or 30, you don’t have much cardiac output, your blood pressure is low and people usually faint or if they don’t faint, they have to lie down because the blood pressure won’t sustain them standing up. The treatment for 3rd degree heart block, of course, is a pacemaker. 15:09 We put in a mechanical box that recognizes when there's no ventricular beat and puts one in through a wire - stimulates the heart so that the heart contracts. 15:20 In the old days, people used to die from this before pacemakers. And at autopsy, the heart muscle look good, the valves were good, the coronary arteries were good. We used to call this, “heart's too good to die”. Once pacemakers came along, of course, patients didn’t die. They did extremely well with the pacemaker implanted, we gave them an artificial electrical system. Sometimes we put up wire in the atrium as well as the ventricle so we cause a P wave and we also cause a QRS. It depends, this is the purview of the cardiac electrophysiologist to decide exactly which device is best for you in a particular setting and in a particular form of heart block. Now, this slide is entitled, “All that glitters is not gold”. In other words, sometimes it looks like gold, but guess what? It’s not gold. So, when you look at the rhythm strip at the top, it looks like ventricular fibrillation, right? Except this patient was actually brushing their teeth. Don’t rush in and shock this patient because they were doing tooth brushing. If you look carefully, you can see the beats going up and down, but up on top, you can see the regular beat coming through. I can see 1 2 3 4 regular beats coming through and of course, when you go into the room expecting to see ventricular fibrillation, the patient is in there brushing their teeth. 16:46 The one down below, how many P waves are there down there? Looks like lots of P wave. Actually, that’s a patient with a tremor, a benign, essential tremor, so of course, theres artefact introduced on the electrocardiogram. When the electrocardiogram is taken, the patient has to be absolutely still and there has to be no electrical machinery going in the room so that we see the actual electrocardiogram and not artefacts, not false images that occur from the electrical activity or from patient bodily movement as well. So, as I've said down there, the bottom one is due to a tremor in the patient.
About the Lecture
The lecture Sinus, Atrial and Ventricular Rhythm – Cardiac Dysrhythmia by Joseph Alpert, MD is from the course Cardiac Diseases.
Included Quiz Questions
Which of the following can appear as bigeminy on the ECG?
- Premature atrial contractions
- Left bundle branch block
- Atrioventricular re-entry tachycardia
- Atrial fibrillation
- Sinus bradycardia
Approximately what percentage of people over the age of 80 have atrial fibrillation?
- 10%
- 20%
- 30%
- 40%
- 50%
A saw-tooth appearance on the ECG is typically seen in which of the following cardiac arrhythmias?
- Atrial flutter
- Sinus tachycardia
- Ventricular fibrillation
- Atrial fibrillation
- Premature atrial contraction
Atrial flutter can often degenerate into which of the following cardiac arrhythmias?
- Atrial fibrillation
- Ventricular fibrillation
- Premature atrial contraction
- Ventricular tachycardia
- Sinus tachycardia
In the case of ventricular fibrillation, blood is no longer pumped out of the heart. In such a case, how long does it take for cell death to begin within brain neurons?
- 4-5 minutes
- < 1 minute
- 8-10 minutes
- 15-20 minutes
- > 30 minutes
Which of the following findings on an ECG is characteristic of a sinus rhythm?
- One upright, uniform P wave before every QRS
- Wide QRS complexes
- Tall peaked T waves after every QRS
- A baseline of indiscernible P waves
- "Sawtooth" appearance of the P waves preceding every QRS
Why is there a grossly irregular ventricular rhythm seen in atrial fibrillation?
- Random transduction through the AV node
- Rapid circular conduction of electrical signals around the atrium
- Electrical signals originate below the AV node
- Premature depolarization of cardiac cells
- Conduction of electrical signals through accessory tracts
What finding on ECG may help a clinician identify electrical activity originating from the ventricles?
- Wide QRS complex
- Narrow QRS complex
- Long PR interval
- Rate >100
- Dropped QRS complex
Customer reviews
3,7 of 5 stars
| 5 Stars |
|
2 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
1 |
Easy to understand, well explained, very high yield. thank you
This review was better than an entire course I took at work regarding EKGs. Thank you!
ECGs are still ambiguous. there should atleast be a pointer on the screen to indicate what and where he is talking about. I am lost in his coordinates. Its like teaching map skills without a map legend