Playlist
Show Playlist
Hide Playlist
Types of Ovarian Tumors: Sex Cord-Stromal Tumors & Granulosa-Theca Tumor
-
Slides Ovary Female Repro.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
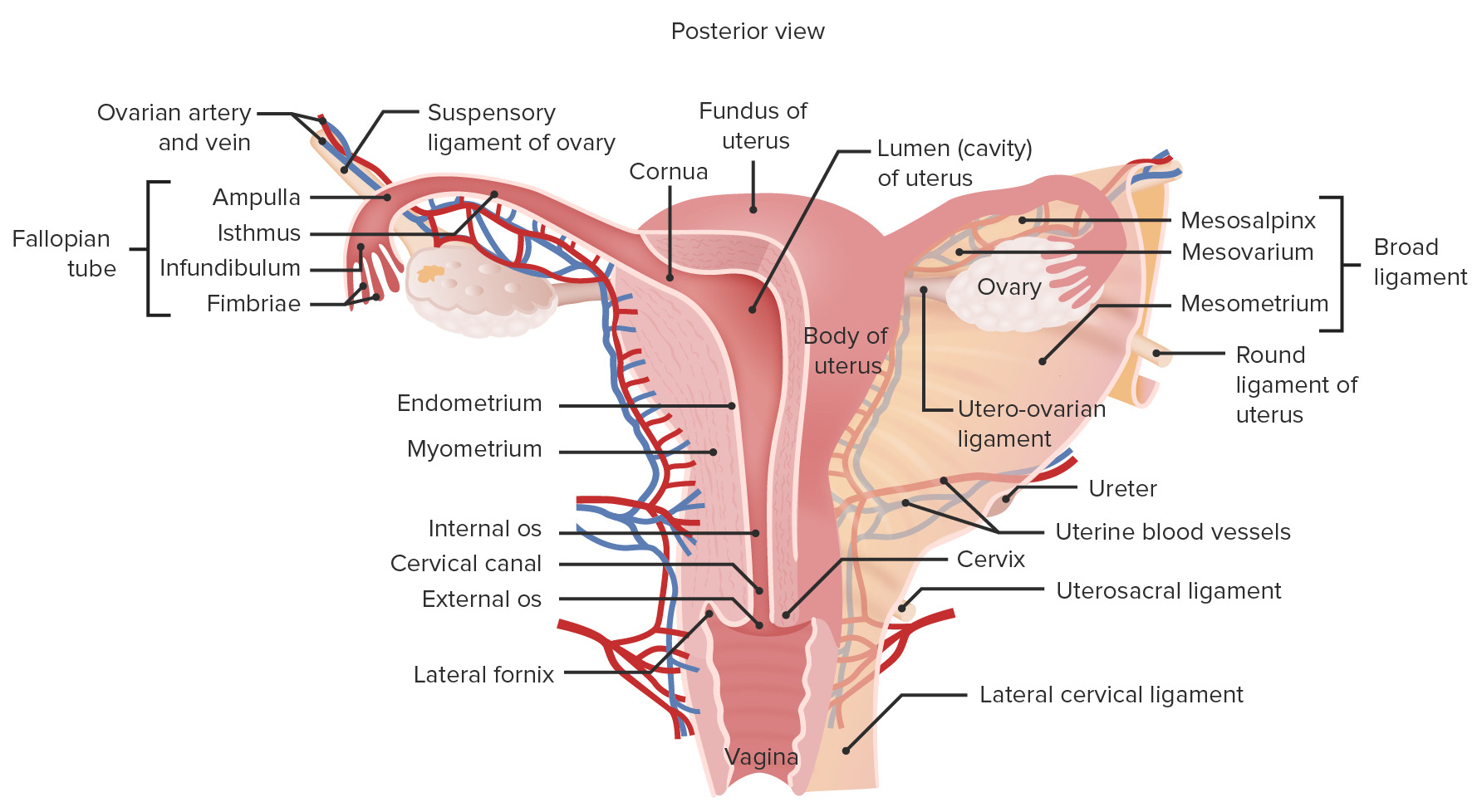
00:02 Our next topic here is sex cord-stromal tumor. 00:04 Obviously, a percentage of ovarian tumors are dropping, so therefore I’m going to be much more specific as to what you need to know for these specific tumors. 00:12 Let’s take a look. 00:14 Overall frequency, take a look at a measly 5 to 10%, the proportion of malignant ovarian tumors overall only 2 to 3%. 00:21 The age group will be all over the place and the types include fibroma, granulosa and Sertoli. 00:27 Let me stop here and make sure that you understand the significance of some of these histologic cells. 00:34 Fibroma. 00:35 Okay, we’ll talk about that. 00:37 Granulosa theca, this is a female. Ovary, follicle. 00:41 Tell me about the histologic appearance in a normal follicle. 00:44 Inner granulosa, outer theca. 00:46 So far, so good. 00:47 You focus upon the granulosa. 00:50 Then we have the next type. 00:51 "Dr. Raj, are you sure that’s not a typo?" I’m positive. It’s not a typo. 00:56 This is a Sertoli–Leydig cell tumor. 00:59 "I know for certain in physiology, Dr. Raj, that Leydig cells are found in a male and LH works upon it. 01:05 And then in a male, it produces testosterone." Absolutely. 01:09 So what business does this have doing in an ovary? It’s a cancer. 01:14 Okay? It can do whatever it wants. 01:16 It can turn into whatever it wants. 01:19 Your focus is going to be on Leydig of an ovarian tumor. 01:23 She – genotype XX. 01:28 She is going to be producing excess testosterone. 01:33 What do you think is going to happen to her? Masculinization. 01:39 Let’s see the opposite. 01:41 If you have a testicular tumor, a male, XY, in which a testicular tumor is a granulosa type. 01:50 A male should not have normal granulosa cells. 01:54 We have outer Leydig, inner Sertoli. 01:57 Right? Our blood test's barrier. 01:59 But if it’s a granulosa cell tumor in a male, then what is he going to – How is he going to present? That granulosa is going to produce a lot more estrogen. 02:10 Correct? This estrogen in male, what is going to happen to him? How is he going to present? Feminization. 02:18 Use your normal anatomy and physiology so that you can truly understand our pathologies. 02:24 I’ve done this, too, numerous times, yet here’s another example. 02:29 Granulosa theca cell tumor. 02:31 Now it becomes easy. 02:34 So make sure you have granulosa and theca cell. 02:36 This is tumor though. 02:37 So therefore this is going to be rather chaotic. 02:40 It may produce large amounts of estrogen, but we already predicted that. 02:43 The granulosa cell, responsible for producing your estrogen. 02:46 Now stop here. 02:48 What’s my topic and who’s my gender? My topic is ovarian tumor. 02:51 My gender is female. 02:53 She is genotypically XX. 02:56 So she’s already feminized. 02:57 So what then happens to her or in terms of how is she presenting that makes her more feminine? Well, it’s not so much that. 03:05 She's -- She’s experiencing precocious puberty. 03:08 Early, early puberty. 03:10 So precocious sexual development. 03:12 Look for breast being developed maybe much earlier, 12 or 13 years of age. 03:17 Her clitoris is well-developed, so on and so forth. 03:21 Endometrial hyperplasia and carcinoma post menopausal, that’s dangerous. 03:25 Isn’t it? Why? I asked you earlier for endometrial hyperplasia and carcinoma, to group them together and the risk factors will be the same. 03:36 The major risk factor? Good. 03:38 Estrogen. 03:40 That’s what you’re producing too much of in this tumor. 03:44 Potentially malignant especially granulosa type, that’s the one you to pay attention to. 03:48 And here, we have an interesting, interesting histologic feature. 03:53 The small follicle, granulosa theca cell tumor. 03:56 It’s a small follicle with eosinophilic material. 04:01 That’s what you’d expect to find upon your histologic examination. 04:05 You will refer to this as being your Call-Exner body. 04:08 Call-Exner body. 04:09 At least know the description. 04:12 Eosinophilic material within your small follicle. 04:15 You do not find cyst per se, huh? So whenever we talk about follicles that have fluid in them, cyst. 04:23 Then you go back to surface-derived. 04:25 With surface derived, you have serous, mucinous and so on and so forth. 04:29 Here, we have our Sertoli-Leydig cell tumor. 04:32 Once again, quickly tell me the gender. 04:36 Female. 04:38 Genotypically XX. 04:40 She’s producing a male-like cell known as a Sertoli cell. 04:46 Responsible for producing androgen. 04:48 Hence, andro -, androblastoma. 04:53 Commonly produces masculinization of your female. 04:55 Blocks normal sexual development in children, and virilization in women. 04:59 What does that mean to you? It means because of this androgen, she has -- They will describe this being ambiguous genitalia. 05:07 Look at the clitoris, it looks like a penis. 05:09 Virilization. 05:10 That’s your most important. 05:12 Leydig. 05:13 Exhibit tubules composed of Sertoli cells or Leydig cells interspersed with stroma. 05:18 If you take a look at the histologic picture, it looks like seminiferous tubules. 05:25 Our topic, Sertoli-Leydig cell tumor of the ovary.
About the Lecture
The lecture Types of Ovarian Tumors: Sex Cord-Stromal Tumors & Granulosa-Theca Tumor by Carlo Raj, MD is from the course Ovarian Diseases.
Included Quiz Questions
What type of ovarian tumor is most likely to cause precocious sexual development in females?
- Granulosa-theca cell tumor
- Sertoli-Leydig cell tumor
- Endodermal sinus tumor
- Ovarian choriocarcinoma
- Ovarian stromal fibroma
What type of ovarian tumor is most likely to cause masculinization/virilization in females?
- Sertoli-Leydig cell tumor
- Granulosa-theca cell tumor
- Endodermal sinus tumor
- Ovarian choriocarcinoma
- Ovarian stromal fibroma
What age group is most affected by ovarian sex cord-stromal tumors?
- All ages are affected
- Girls under age 5 years
- Prepubescent girls
- Women of childbearing age
- Postmenopausal women
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |