Playlist
Show Playlist
Hide Playlist
Seizures: Pathophysiology
-
Emergency Medicine Bord Seizure.pdf
-
Download Lecture Overview
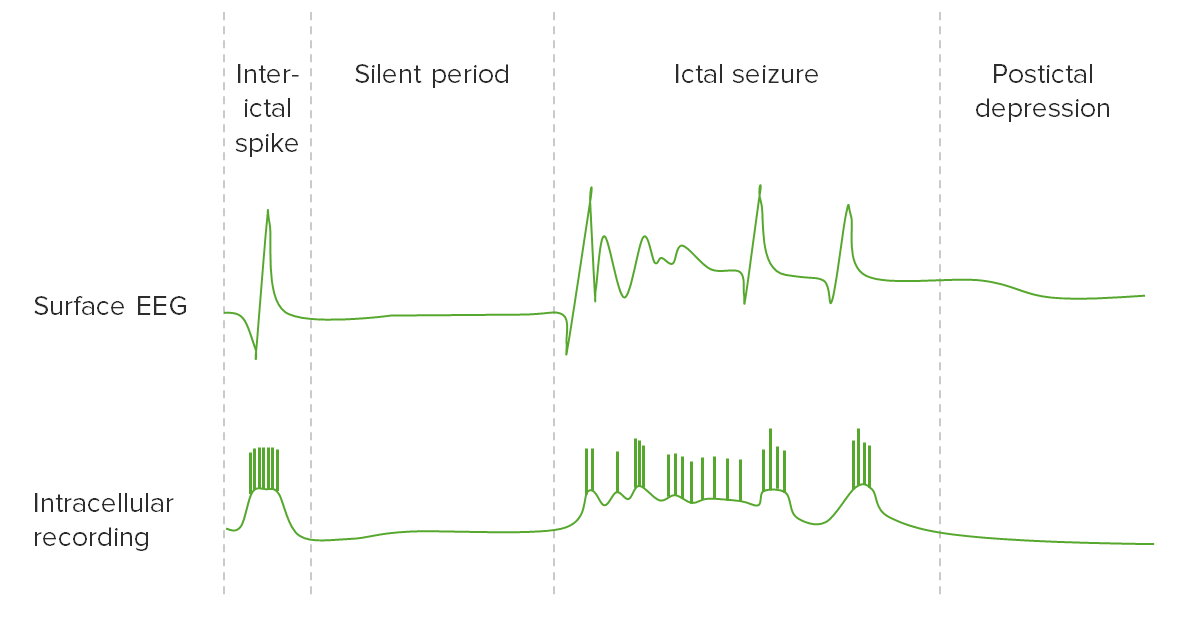
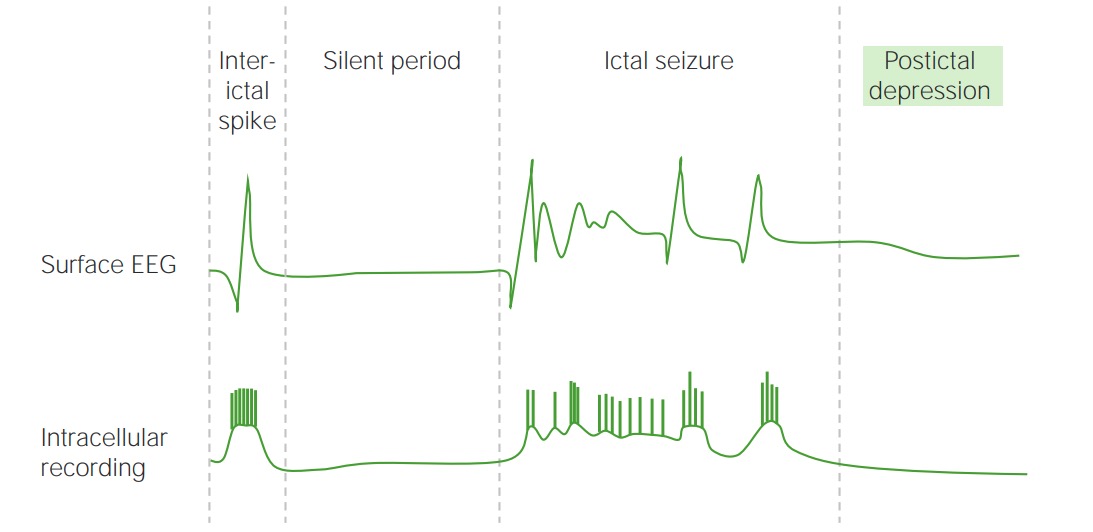
00:02 Now, why do patients get seizures? It’s multifactorial. 00:05 Part of it is that there’s disruption of the neurotransmitters so there’s increased excitatory neurotransmitters. 00:12 Increased neurotransmitters that are gonna cause this motor activity. 00:16 Among those are acetylcholine and glutamate. 00:20 There’s also increased sympathetic stimulation and with that increased sympathetic stimulation does is it increases the temperature. 00:27 So often times patients who have had a seizure when they come into the Emergency Department will have an elevated temperature, an elevated lactic acid level often times also this will be reflected in blood work if it’s checked on patients right after they arrive, an increased heart rate and an increased respiratory rate. 00:48 So when someone is having a seizure if they’re on the cardiac monitor you’ll definitely be able to observe that the heart rate is faster as well as the respiratory rate. 00:57 There’s also increased autonomic stimulation and what this leads to is it leads to incontinence of urine and stool, can lead to biting of the tongue or oral trauma which can in turn potentially lead to an airway issues. 01:11 So when you have this tongue biting and the clenching of the jaw that can in turn occlude the patient’s airway and lead to a possible airway issues. 01:20 So for patients who are having seizures, you always wanna make sure that you’re monitoring their airway status and potentially definitely being cautious or looking out for the patient to get hypoxic or not have effective breathing anymore. 01:35 When taking the history, one of the first things that you wanna try and figure out is if the patient has had a seizure before. 01:41 So is this the first time ever that they’ve had a seizure or have they had prior seizures? And if they’ve had prior seizures, you wanna figure out what medication they’re supposed to be taking. 01:52 Now one of the big reasons that people have seizures or come to the Emergency Department for a seizure is because they have a known seizure disorder but they are not being compliant with their medication. 02:02 So they’re not taking their medication like they’re supposed to and this can be for a variety of reasons. 02:07 It can be because they can’t afford their medication, it can be just because they don’t know how they’re supposed to take their medication. 02:13 So a variety of reasons can cause people to not take it but definitely trying to figure out what they’re on can be helpful for a couple of reasons. 02:21 So one reason is if you figure out what medication they’re on and they haven’t been taking it like they’re supposed to, you can administer that medication to them in the Emergency Department. 02:31 The other reason is you can check the level of some of the medications. 02:36 So medications that you can check levels of are phenytoin is one of them, levetiracetam is another medication that you can check the level of. 02:46 Other important historical points are figuring out if there’s been a recent illness. 02:50 So has that individual been sick recently? Have they had a fever or any other kind of issues and were there any other seizure precipitants? So anything else that can cause a seizure among those things would be substances. 03:05 Tramadol is a classic one that can sometimes lead to seizures. 03:10 There’s a handful of drug use, illicit substances that can lead to seizure disorder. 03:15 Another important seizure precipitant that you wanna think about are withdrawal states. 03:20 So benzodiazepine medications as well as alcohol related withdrawal can cause seizures so that’s the other big category that you wanna make sure you’re thinking about and asking about on history. 03:33 So drugs and medications, what drugs is the patient supposed to be on? What medications are they supposed to be taking whether or not they’re taking them effectively? Also asking about those illicit substances so did someone abused cocaine is a classic one that can cause seizures or any other substances that may lead to that. 03:57 Was it a witnessed seizure? Did anyone see it? This is one of the big things that we try and figure out in the Emergency Department especially if someone doesn’t have a history of seizures. 04:07 We try and figure out what it looked like. 04:09 The classic thing with seizures is that your patient should not be able to tell you what happened for the most part especially in those generalized seizures. 04:17 Now in a partial seizure, they may be able to tell you. 04:20 For the most part here we're talking about that generalized tonic-clonic seizure. 04:24 So did someone see it? And if so, try and talk to that person. 04:29 Try and figure out what they saw because there are some seizure mimics and we’ll talk about those in a few moments but there are some things that may look like a seizure but that aren’t a seizure so trying to find a witness or someone who saw that event is very important. 04:43 Other things that can clue you in are incontinence. 04:47 So did your patient were they incontinent of urine or stool? And sometimes we don’t have the most glamorous job in the Emergency Department and seeing if someone, you know, urinated or defecated on themselves is part of our job. 04:59 Was there any oral trauma? This is one of those situations you wanna have the patient open their mouth, take a look inside, see if they have any blood around their mouth or any trauma to their mouth and this goes into the physical exam as well. 05:12 A patient may also be able to tell you like “Yes, I in fact bit my tongue.” Or a family member may be able to tell you that they saw blood coming from their mouth. 05:20 The other thing is confusion following the event. 05:24 We talk about the post-ictal period. 05:27 That’s the period following the seizure where someone is to be confused. 05:31 Now, that is the classic thing with the generalized tonic-clonic seizure. 05:35 Patients by definition have to have that post-ictal period. 05:40 If they don’t have that post-ictal period, they don’t have that period of confusion, you wanna potentially start thinking about other things. 05:47 So talking to whoever saw the event or possibly the medics who got there after the event and finding out was the person confused or they’re totally with it. 05:56 Someone who’s totally with it following an event might not necessarily have had a seizure or most likely did not actually have a seizure.
About the Lecture
The lecture Seizures: Pathophysiology by Sharon Bord, MD is from the course Neurologic and Psychiatric Emergencies.
Included Quiz Questions
Which of the following are NOT seen in patients having seizures?
- Hypothermia
- Increased lactic acid
- Tachycardia
- Tachypnea
- Increased glutamate
Which of the following is a sympathetic nervous stimulation that can be seen during a seizure?
- Tachyarrhythmia
- Tongue biting
- Urinary incontinence
- Hypotension
- Hypothermia
Which of the following drugs is most strongly associated with seizure occurrence?
- Cocaine
- Alcohol
- Caffeine
- Lysergic acid diethylamide (LSD)
- Methadone
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |