Playlist
Show Playlist
Hide Playlist
Secondary Hyperparathyroidism (SHPT) and Tertiary Hyperparathyroidism (THPT)
-
Slides Hypercalcemia.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
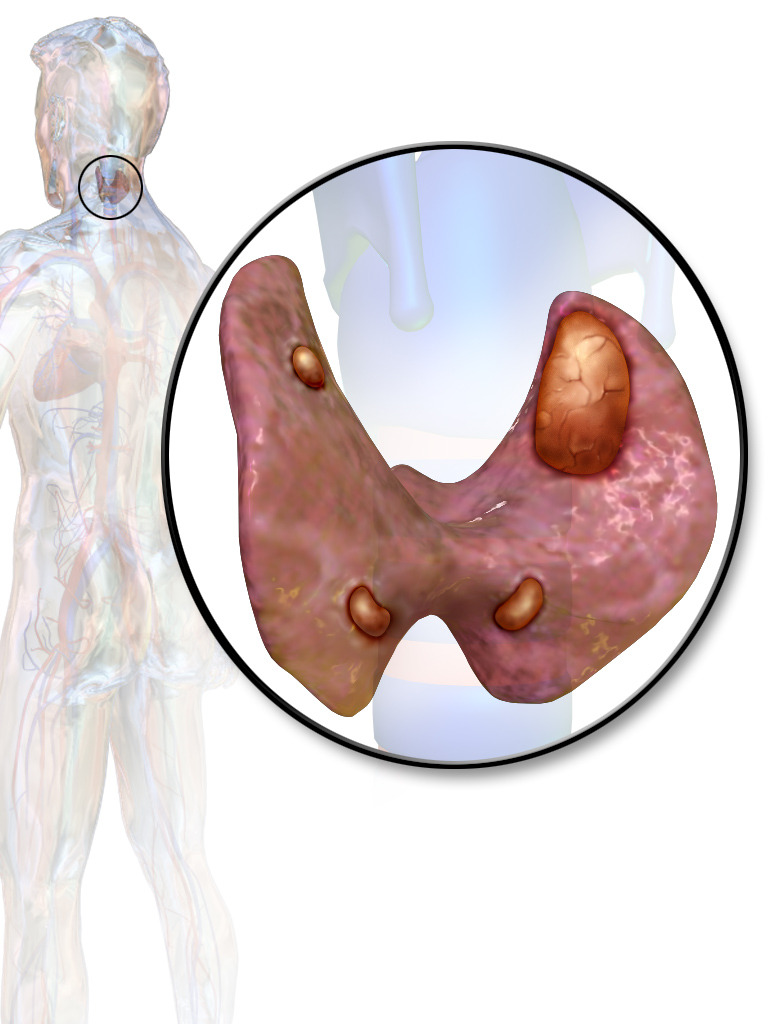
00:01 Let’s talk about secondary hyperparathyroidism. 00:03 What does this mean to you? It means that the parathyroid glands are responding to decreased calcium. 00:10 So, what happened first? A decrease in calcium. 00:13 The decrease in calcium will then trigger the parathyroid from releasing the parathyroid versus primary. 00:20 The main causes include… well, most common would be, let’s say your patient has diabetic nephropathy, may result in chronic renal failure. 00:28 So, therefore, you walk into a dialysis clinic and each one of those patients is experiencing renal failure. 00:38 When renal failure is taking place, each one of those patients sitting on their thrones, you know for a fact, is Vitamin D deficient because the kidneys aren’t working properly, don’t have 1-alpha hydroxylase activation, Vitamin D is not properly formed or active Vitamin D is not formed; the calcitriol not being present may result in osteomalacia or decreased calcium. 01:01 That decrease in calcium may then trigger secondary hyperparathyroidism. 01:05 Our discussion in nephrology took us through what may then happen when there is renal failure. 01:11 Now, because the kidneys aren’t working properly and you have too much PTH, the PTH does not work on the kidney whatsoever because the kidney’s dead. 01:20 It’s going to go to the bone and start destroying it, but we do not call this osteitis fibrosa cystica, do we? What do we call this? Renal osteodystrophy. 01:32 Every single patient in a dialysis clinic is receiving some form of calcium because for a fact you know that with chronic renal failure, the patient will be deficient of Vitamin D or calcium. 01:47 Increased serum phosphorus binds with calcium. 01:49 Why is phosphate even elevated in a patient with renal failure? Important beyond belief, right? Because the kidneys are dead. 01:55 If the kidneys are dead... remember normally, what does PTH do with the phosphate in the kidney? It flushes it out, it inhibits the reabsorption of phosphate. 02:04 If the kidney is not working, understand that your patient is in a state of hyperphosphataemia. 02:10 Now, if there is hyperphosphataemia, it will then bind to the calcium exacerbating the effect of decreased calcium activity. 02:22 Vitamin D deficiency… For whatever reason, meaning maybe from the diet, but that’s rather difficult in developed country; maybe there’s liver damage. 02:31 Remember, what’s a major circulating form of Vitamin D? 25 hydroxylation of your Vitamin D. What if you don’t have the liver? Then you don’t even have the first step of activation, so you become Vitamin D deficient. 02:43 So, think of all the different reasons as to why a patient might have cirrhosis, right? NASH, maybe autoimmune disease or alcoholism, hepatitis, whatever it may be. 02:54 Clinical features, if the kidneys aren’t working properly may result in renal osteodystrophy and something called metastatic calcification. 03:04 Nothing to do with cancer and what that basically means is that with all these calcium, it is then depositing upon normal tissue, isn’t it? Metastatic calcification. 03:14 You’ve heard of metastatic calcification, you’ve heard of dystrophic calcification. 03:20 Metastatic calcification, secondary hyperparathyroidism, may result or deposit a normal tissue and cause damage. 03:26 Nothing to do with cancer; be careful with the name. 03:30 Biochemical findings… with secondary hyperparathyroidism, well, the initial event was the low calcium. 03:35 Look for that. 03:38 This then causes secondary. 03:40 The phosphate levels are variable depending on the etiology. 03:42 What does that mean? Take a look. 03:44 It’s… What’s the most common cause of hypocalcemia initially? It’s the chronic renal failure. 03:54 If there’s chronic renal failure, if the kidneys aren’t working, you can’t flush out the phosphate, your phosphate levels will be high… incredibly important. 04:05 You need to chelate that phosphate in a renal failure patient. 04:09 If there is Vitamin D deficiency for, by any other cause, what does that mean? For example, liver damage or maybe industrialized nation. 04:18 I don’t spend a lot of time outside in the sun. 04:22 So, if I have lack of UV exposure from the skin, I don’t release Vitamin D. I may then become Vitamin D deficient. 04:29 It has nothing to do with the kidney. 04:32 So, when there is deficiency of Vitamin D due to other causes, then you trigger secondary hyperparathyroidism, it turns to the kidney, waste away the phosphate. 04:44 The phosphate will be low. 04:46 And understand that the PTH may then turn to the bone and when you start resorbing your calcium and such from the bone, you’ll find an increase in… what are you-what are you going to use as a marker for bone destruction? Any time there’s bone issue, alkaline phosphatase. 05:06 ALK Phos will be elevated, if you’re thinking about PTH activity on your bone or any type of issue with the bone. 05:12 But, here, you should understand as to why. 05:16 Tertiary hyperparathyroidism, what the heck is causing tertiary hyperparathyroidism? Well, step by step. 05:23 Who controls your PTH? The calcium. 05:27 When parathyroid activity becomes autonomous from a pre-existing secondary hyperplasia, that’s tertiary hyperparathyroidism, has nothing to do with primary hyperparathyroidism. 05:38 Secondary hyperparathyroidism was-was caused by the inciting event of hypocalcemia whereas tertiary would be a pre-existing secondary hyperplasia.
About the Lecture
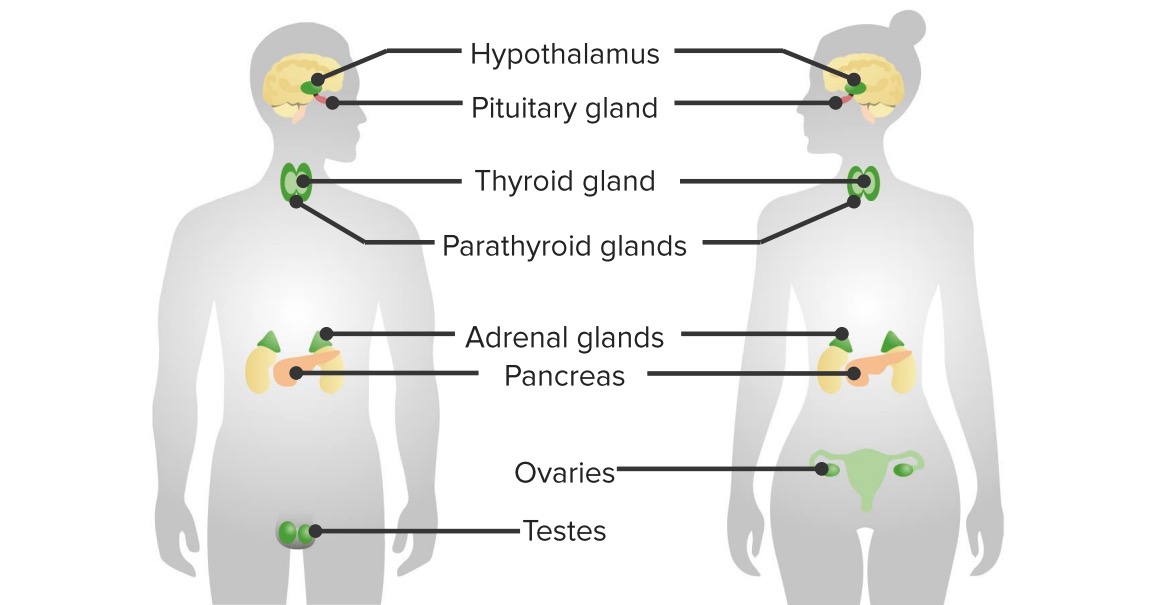
The lecture Secondary Hyperparathyroidism (SHPT) and Tertiary Hyperparathyroidism (THPT) by Carlo Raj, MD is from the course Parathyroid Gland Disorders.
Included Quiz Questions
A patient with liver disease presents with a deficiency in active vitamin D. What would NOT be an expected lab value?
- Increased phosphate
- Increased PTH
- Decreased or normal phosphate
- Increased alkaline phosphatase
- Decreased serum calcium
Which sentence best describes tertiary hyperparathyroidism?
- Autonomously increased PTH secretion due to secondary hyperplasia
- PTH secretion is dependent on levels of calcium but unresponsive to vitamin D
- Parathyroid hormones that increase PTH secretion before becoming quiescent
- PTH secretion that responds to negative feedback from bound instead of free serum calcium
- PTH secretion that responds to signals from the kidney but not to serum electrolyte levels
Customer reviews
1,0 of 5 stars
| 5 Stars |
|
0 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
5 |
5 customer reviews without text
5 user review without text