Playlist
Show Playlist
Hide Playlist
Rheumatoid Arthritis (RA): Pathogenesis
-
Rheumatology I 03 Connective Tissue Diseases.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
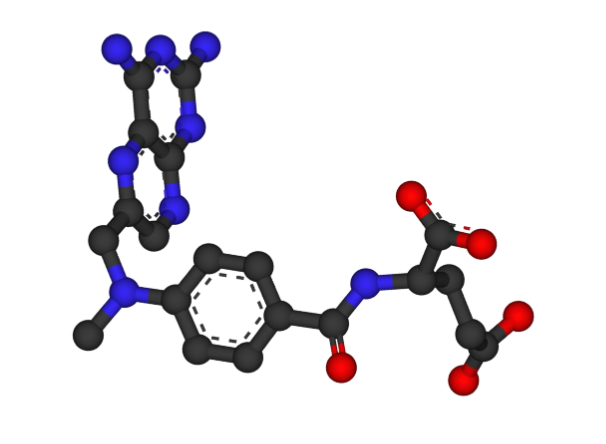
00:01 What you've been waiting for? Rheumatoid Arthritis. 00:04 Now, as we go through Rheumatoid Arthritis, you'll be comparing and contrasting it with osteoarthritis. 00:10 Let’s begin. 00:11 So what is Rheumatoid Arthritis? Now, as I walk you through this, I'm gonna give you immediate clinical significance, so that you're not wasting time tying things together, when this should have occurred to begin with. 00:23 For example, the chronicity is important for you, why? Let’s keep going. Polyarticular, Inflammatory, no doubt. 00:30 How do I know it’s inflammatory? Because that synovial fluid is gonna have a lot WBC’s, and that by definition is going to classify your arthritis into inflammatory or uninflammatory, that discussion we’ve had. 00:43 Unfortunately, Rheumatoid arthritis as I told you can be quite systemic. 00:47 You’re gonna have other parts of the body including the heart and such cardiovascular that will be affected. 00:52 It is an autoimmune disease and therefore that'll help us then understand the management of this. 00:58 And your focus is going to be on synovium of the joint. 01:02 Now, before we move on please picture the synovium. 01:05 I want you to think of maybe the elbow or I want you to think of the knee. 01:09 You have the joint capsule which it then covers the entire synovial joint. 01:14 On the inner aspect of the joint capsule we have the synovium, which are these little bitty cells. 01:20 Which then are responsible for secreting synovial fluid. 01:24 Which as you know one of the main constituent would be hyaluronic acid which then keeps the joint nice and lubricated, so that prevent any type of friction. Keep that in mind. 01:34 Causes a polyarticular, symmetrical arthritis that we talked about. 01:40 Extra articular manifestations is where we go next. 01:43 You’ll have these Rheumatoid nodules. What is a Rheumatoid nodule? It is fibrinoid necrosis. 01:49 Fibrinoid necrosis along with, what's known as your palisading pattern of histiocytes. 01:56 Where am I? Skin. 01:58 So you have fibrinoid narcosis taking place of the blood vessel, along with it though, you will have a pulsating pattern of histiocytes. 02:05 You could have Rheumatoid nodules, skin, lungs, then rheumatoid nodules. 02:12 In other words you could have involvement of the lung as well, resulting interstitial fibrosis. 02:17 Or you could have rheumatoid type of vasculitis. 02:20 Skin, nerve, internal organs maybe affected. 02:24 You could have involvement of the sclera, picture that. 02:28 You can have episcleritis. 02:30 We talk about what Felty’s syndrome is, not only could you have anemia of chronic disease, but the you could also have neutropenia. 02:38 But the neutropenia plus your splenomegaly, left upper quadrant fullness. 02:42 So if for example there’s rheumatoid arthritis. 02:45 And there is a description or there is a finding of left upper quadrant fullness. 02:51 You should be thinking about Felty’s syndrome, but combination of neutropenia and splenomegaly gives you Felty’s syndrome. 02:57 And then you could have involvement of serosa, so in other words, serositis. 03:03 You could have pericarditis, you could have pleuritis, and perhaps even peritonitis. 03:06 Pericarditis, in other words, leaning back upon inspiration, it hurts. 03:12 Leaning forward, expiration, separate my pericardium and the pain is relieved. 03:20 Pathogenesis, we’re not completely sure. 03:25 However, here’s something that you wanna keep in mind. 03:27 The antigen-presenting cells later be dendritic or the macrophages. 03:31 Maybe the T or B lymphocytes and neutrophils might be then involved. 03:35 These cells elaborate, in other words, you could have your cytokines, especially anti-TNF therapy is part of the regime, right? especially anti-TNF therapy is part of the regime, right? Your biologics because TNF-alpha will play a role with the inflammatory process. 03:49 The rheumatoid factor, we've talked about earlier is an IgM which is then targeting the FC region of the IgG. 03:57 I also told you the Rheumatoid factor will be more specific for rheumatoid arthritis. 04:01 Correct? And here it is. 04:03 But there’s something even more specific, it’s called Cyclic citrullinated peptide. 04:07 Talked about this earlier. 04:09 These are specific and/or aggressive forms of rheumatoid arthritis. 04:15 Also associated with the female gender. 04:19 In general, you know that if you referred to autoimmune diseases, you are dealing with or unfortunately the ladies are dealing with autoimmune diseases. 04:29 HLA-DR4 is another propensity. 04:31 Complex interaction take place in the synovium. 04:36 I told you earlier that you wanna focus upon the synovium. 04:39 Now with that synovium, it is then contributing to a pannus formation. 04:44 Now, that pannus formation, in other words, it's a granulation tissue which is proliferating. 04:49 What is pannus? Pannus is a granulation of tissue which is proliferating. 04:53 And that proliferating and granulation of tissue within the joint capsule, by the synovium is causing complete degradation of everything in sight. 05:04 In other words, you’re gonna have massive erosion of the bone and massive erosion of the cartilage. 05:10 What do you think happens to the amount of synovial fluid in rheumatoid arthritis? It’s increased obviously. 05:17 Synovial fluid is not found to be increased in osteoarthritis. 05:22 Now, if the patient goes on without treatment, an inflamed synovium can erode everything in sight. 05:30 And these erosions will then unfortunately may then become a permanent disability. 05:35 Therefore, the current therapy is to reverse the synovitis and the synovial thickening. 05:42 Are there actual agents? Well, yes, some of these biologics or maybe even some of these DMARDs that we’ll take a look at, but keep that in mind though, because if this occurs, erosion, it’s irreversible. 05:55 With rheumatoid arthritis, what are the joints that are commonly affected? You’ll notice here that the hand has been emphasized, you see that? The hand, and remember that ulnar deviation that I presented to you earlier on both sides? Symmetrical. 06:14 Well, not only could the wrist be involved but maybe the metacarpophalangeal joints. 06:19 Stop there for one second, ask yourself. 06:22 Are the metacarpal pharyngeal joints involved in osteoarthritis? Good. They are not. 06:29 Metacarpal pharyngeal joints are more commonly affected in Rheumatoid arthritis. 06:33 What about the PIP? Proximal interphalangeal joint. 06:37 Yes, those can be affected in both. 06:39 However, the PIP involvement in osteoarthritis. 06:42 What were they called, those nodes? I know you were already thinking that and you probably knew that I was gonna ask it. 06:48 And you got ahead and we’re thinking these are Bouchard. 06:52 That’s what it was in osteoarthritis. 06:55 That is not what these are called here. What are they? Just they are the involvement of your PIP, be careful. 07:01 So Bouchard and Heberden's nodes are only for osteoarthritis. 07:07 Rheumatoid arthritis involvement of the wrist, metacarpal pharyngeal and PIP, stop there. 07:12 DIP, rare if ever affected. 07:16 In osteoarthritis was the thumb affected? It was, remember the trapezium, carpal, metacarpal, joint. 07:27 That was affected of the thumb in osteoarthritis, not the case in rheumatoid arthritis. 07:33 Keep that in mind. Is that clear? If you take a look at the picture, what exactly are we looking at? Let’s have you immediately go to the synovial fluid please. 07:41 Lots of synovium, so here’s my knee and you’re gonna have the synovial cells undergoing inflammation. 07:51 You’re gonna have this pannus formation. 07:54 Pannus formation would be the granulation tissue which has then proliferating causing destruction, erosion of the bone and the cartilage. 08:03 And once that happens, remember, and if the patient is not found out early enough, then this then becomes a permanent disability. 08:11 In fact, a person who has severe untreated rheumatoid arthritis. 08:16 might cut short their life by ten years because of rheumatoid arthritis if not managed properly. 08:23 So we’re talking about significant repercussions. 08:26 In addition, inflamed joint capsule and inflamed synovium and in that synovium, you’re going to find quite a bit of inflammation.
About the Lecture
The lecture Rheumatoid Arthritis (RA): Pathogenesis by Carlo Raj, MD is from the course Connective Tissue Diseases. It contains the following chapters:
- Introduction to Rheumatoid Arthritis
- Pathogenesis of Rheumatoid Arthritis
Included Quiz Questions
Which of the following statements is NOT true regarding rheumatoid arthritis?
- It is not an inflammatory disease.
- There is symmetric joint involvement.
- It is a chronic disease.
- The disease affects the synovium of the joints.
- It is an autoimmune disease.
Which of the following joints is LEAST likely to be affected in rheumatoid arthritis?
- Carpometacarpal joint of the thumb
- Proximal interphalangeal joint
- Wrist joints
- Metacarpophalangeal joint
- Knee joint
What is Felty syndrome?
- Neutropenia and LUQ fullness due to splenomegaly, seen in patients with rheumatoid arthritis
- Neutropenia and hemolytic anemia seen in patients with rheumatoid arthritis
- Pericarditis and neutrophilia seen in patients with rheumatoid arthritis
- Episcleritis and anemia seen in patients with rheumatoid arthritis
- Vasculitis and interstitial fibrosis seen in patients with osteoarthritis
What extraarticular manifestations are seen in patients with rheumatoid arthritis?
- Lung nodules, interstitial fibrosis, and vasculitis
- Liver nodules and splenomegaly
- Erythrocytosis and liver fibrosis
- Vasculitis, sinusitis, and polychondritis
- Glomerulonephritis and episcleritis
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
this lecture helped to do my research and explain this disease