Playlist
Show Playlist
Hide Playlist
Rheumatoid Arthritis: Diagnosis, Pathogenesis, and Treatment
-
Slides Rheumatoid Arthritis .pdf
-
Reference List Rheumatology.pdf
-
Download Lecture Overview
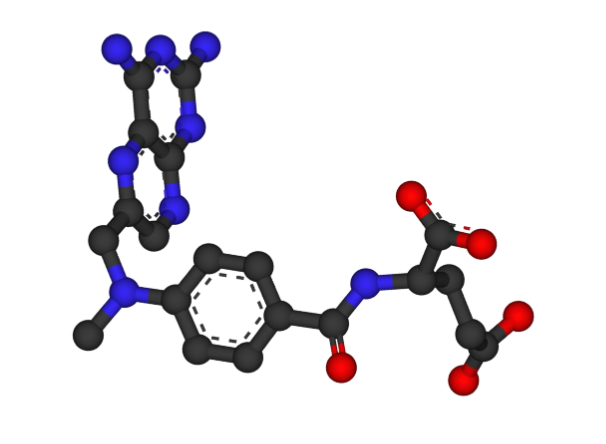
00:01 First off, his history of hypertension is important for a number of reasons. 00:05 Keep in mind that patients with rheumatoid arthritis have a chronic inflammatory state going on. 00:10 While we would always counsel a patient about cardiovascular risk if they have hypertension and he smokes a pack a day, rheumatoid arthritis is gonna raise the stakes even further. 00:20 All that chronic systemic inflammations and major cardiovascular risk factor, by virtue of progressive damage to your entire circulation and your endothelial cells on all your vessels. 00:30 So, something that he should be mindful of and hopefully would ammunition to help encourage him to quit smoking. 00:36 And lastly, on the topic of smoking, while I mentioned this before, rheumatoid arthritis is considered an idiopathic disease. 00:43 There is really strong evidence that smoking itself is an independent risk factor for rheumatoid arthritis. 00:49 So not only does it predict disease, but it also predicts disease progression. 00:53 It's gonna be a lot harder to treat his rheumatoid arthritis as long as he's smoking so he's got some really good reasons to quit smoking. 01:00 As further indication of the systemic inflammatory nature of rheumatoid arthritis, as many as 2/3 of patients with newly diagnosed RA will have antecedent systemic symptoms before arthritis even develops. 01:12 Now, this might include just general fatigue, malaise, etc., as in our patient or it might involve weight loss, generalized weakness or even subjective fevers. 01:22 Now, family history is crucial to taking a history in patients with joint inflammation. 01:27 Now, our professor did not end up having psoriatic arthritis but a family history of any kind of autoimmune disease nearly always increases your risk of your patient having some other sort of autoimmune disease. 01:38 Now the most common genetic association with RA is the HLA-DR4 allele which is also coincidentally one of many alleles associated with psoriasis. 01:49 So I suspect the uncle having psoriasis is still related to our patient's development of rheumatoid arthritis. 01:55 Next stop, I sort of mentioned this a little bit before but don't be led astray by the absence of joint deformity even though you're accustomed to seeing pictures of joint deformity if you're looking at any textbook on rheumatoid arthritis. 02:09 Oftentimes, we're thinking about really advanced changes like Boutonniere's deformities and Swan neck deformities, ulnar deviation, etc., but the findings in our gentleman with less than six months of symptoms are gonna be much more subtle and the radiographic findings are gonna be much more subtle. 02:24 and with advances in diagnoses in treatment, we're gonna just see a lot less of those advanced changes than might have been present historically. 02:32 So, just keep that in mind. The most common joints, speaking of joints, that you're gonna see in rheumatoid arthritis are circled in red on this plain film here and on this centuries-old drawing by Vesalius. 02:44 See how we're highlighting the MCPs in that radiographic picture as well as the PIPs, the proximal interphalangeal joints, and the wrist joints. 02:54 In contrast, DIPs should not be involved. You'd be more thinking about psoriatic arthritis or even hemochromatosis with DIP involvement. 03:02 In addition to those, most common presenting joints that we've mentioned on the x-ray on the left, there are a number of other joints which are commonly involved with patients with rheumatoid arthritis with advanced disease progression. 03:14 These would include the elbows, the shoulders, the knees, and rarely, we can oftentimes see Atlanto-axial subluxation which is where the C1 and C2 vertebrae are no longer articulating correctly and can even lead patients to have acute spinal stenosis issues, when they twist their head to the left or to the right, you can actually pinch the spinal cord. 03:34 So, that's a potentially devastating manifestation of late, uncontrolled rheumatoid arthritis. Thank you, Vesalius. 03:42 Lastly, this finding down here of an immobile nodule. 03:46 This is suggestive of a rheumatoid nodule, which is a painless subcutaneous growth which can be up to several centimeters in size, often found on extensor surfaces at pressure points like the olecranon process, the Achilles tendon, maybe the forearm and some other sites. 04:02 Now, they are in themselves completely benign though they may be associated with more severe rheumatoid arthritis disease. 04:09 and of note, they can also appear on viscera like in the lungs or even on the vocal cords so it's something to be mindful of if you find something on a deeper imaging. 04:19 Looking at the blood work as I mentioned, a normocytic anemia is the most common hematologic abnormality in RA but completely non-specific. 04:28 We should probably talk briefly about this rheumatoid factor thing so we make sure we understand what that actually means. 04:34 So, what is rheumatoid factor? Now, we know that rheumatoid arthritis is an idiopathic condition but we do know that it is a T-cell mediated autoimmune disease so whatever it is that got those T-cells revved up, they ultimately start to stimulate B-cells and once the B-cells get going, they are producing IgM. 04:55 Remember that IgM antibodies form these pentamers, shown here on the right, and rheumatoid factor which is an IgM antibody has a predilection for the FC portion of another IgG antibody. 05:09 Now, the detection of rheumatoid factor in the serum is about 80% sensitive for rheumatoid arthritis so it's gonna miss some cases of rheumatoid arthritis and those by the way are called seronegative rheumatoid arthritis but it's also a fairly reliable marker of disease activity. 05:26 So the higher the rheumatoid factor level, the more likely this person has active inflammatory disease. 05:32 Rheumatoid factor can also be positive in some other conditions. 05:36 Particularly cryoglobulinemia anemia, Sjogren's, mixed connective tissue disease amongst a variety of others. 05:44 Now, the aforementioned anti-citric citrullinated peptide antibody in contrast is highly specific for rheumatoid arthritis. 05:52 In fact, greater than 95% specific so it's a much better rule in test than rheumatoid factor. 05:59 Now that we made our diagnosis, and we've talked about a few of the pathophysiological principles, let's move on to talk about treatment. 06:06 NSAIDs are very good and very useful for the acute flare. Again, they are anti-inflammatory drugs so they're useful for the short-term. 06:14 You always have to be careful of a person's kidneys and their GI tract but otherwise if there's no other contraindications, getting started with ibuprofen or another NSAIDs is a good way to start. 06:24 Shown here is all of the non-biologic disease-modifying anti-rheumatic drugs and this includes methotrexate, leflunamide, sulfasalazine, hydrocychloroquine and one last one not shown here is azathioprine. The biologic disease modifying anti-rheumatic drugs include TNF-alpha antagonists like infliximab, etanercept, and adalimumab. Then we have our Interleukin-6 receptor antagonists, such as tocilizumab and sarilumab, and lastly , anti-B cell agents such as rituximab, among others. There's a variety of other medications out there as well and it seems like there's new medications coming out all the time. The most important point to highlight about DMARDS is that these agents should be used as soon as possible, once a diagnosis of RA has been confirmed, to prevent the irreversible joint injury that accompanies rheumatoid arthritis disease progression. 07:15 A key distinction of biologic DMARDs is their high cost and exclusively parenteral administration (either by injection or infusion), which sets them apart from conventional DMARDs. This cost and administration factor often influences treatment decisions and insurance coverage requirements. 07:32 Whereas our non-biological ones are very inexpensive for the most part they've been around a long time and many of them are oral. 07:39 A study shown back in 2013 found that the cheap drugs, a triple therapy with methotrexate, sulfasalazine, and hydrocychloroquine was actually more effective than an expensive drug like etanercept with methotrexate which really changed the game in terms of us thinking about how to best manage this disease.
About the Lecture
The lecture Rheumatoid Arthritis: Diagnosis, Pathogenesis, and Treatment by Stephen Holt, MD, MS is from the course Connective Tissue Diseases.
Included Quiz Questions
Which of the following sites is LEAST likely to be affected by rheumatoid arthritis?
- Distal interphalangeal joints
- Metacarpophalangeal joints
- Shoulder joints
- Proximal interphalangeal joints
- Knee joints
Which of the following radiologic signs is suggestive of rheumatoid arthritis?
- Atlantoaxial subluxation
- Subchondral sclerosis
- Chondrocalcinosis
- Pencil-in-cup deformity
- Bamboo spine
Which of the following hematologic conditions is commonly associated with rheumatoid arthritis?
- Normocytic anemia
- Acute intermittent porphyria
- Paroxysmal nocturnal hemoglobinuria
- Macroangiopathic hemolytic anemia
- Porphyria cutanea tarda
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Excelente class. I am from Brazil and help me a lot