Playlist
Show Playlist
Hide Playlist
Pulmonary Vasculitis
-
Slides 08 VascularDiseases RespiratoryAdvanced.pdf
-
Download Lecture Overview
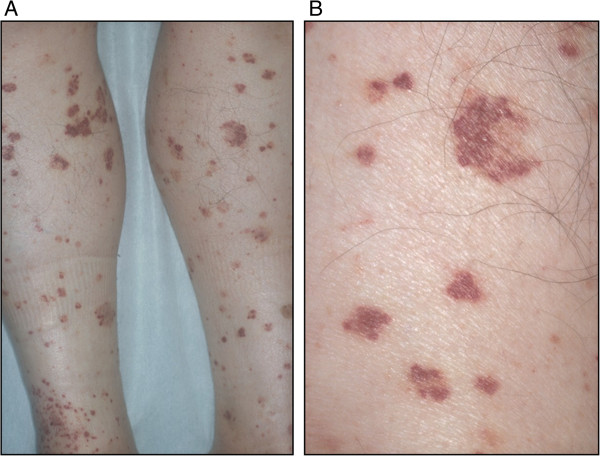
00:00 So the next section of this talk, I'm going to discuss pulmonary vasculitis. Now these are rare diseases, which are autoimmune inflammation affecting lung blood vessels. They are very rare and therefore most people will not see many cases of this but they are important because they do mimic much commoner lung conditions such as cancer and various types of infection, pneumonia, TB, etc. And also, if they are misdiagnosed, the patient is quite likely to die because without intense immunosuppression, these diseases progress rapidly. They can be diagnosed, usually by blood tests, showing positive autoantibodies, the anti-neutrophil cytoplasmic antibody being the most important test, or biopsy of the affected lung tissue showing the vasculitic inflammation of the arteries and arterioles. 00:52 If a patient has one of these diseases then they need to be treated with systemic steroids cyclophosphamide, and potentially other immunosuppressors such as rituximab which removes your B cells and the autoantibodies that are causing the disease in the first place. 01:07 There are different patterns of vasculitis, the three main ones that affect lung is granulomatosis disease with polyangitis, used to be called Wegener's disease. This presents with focal lung nodules that may cavitate, can also cause strictures of the large airways and also, along with the other valculus disease they characteristically have extra thoracic involvement. 01:28 So the vasculitis is affecting the lungs frequently have other organs affected as well, that is a clue to the diagnosis. So for example in granulomatosis with polyangitis, you will get air, nose, and sinus inflammation, kidney involvement, nerve involvement. These patients usually are cANCA positive, which makes the diagnosis much easier than it used to be, because all it requires is a blood test. This could confirm the diagnosis by biopsy. 02:00 Because they present with lumps which may cavitate these patients, look like they may have infection such as tuberculosis or a cancer but it's the vasculitis that is their problem. 02:13 Another relatively common vasculitis is eosinophillic granulomatosis with polyangitis, which used to be called Churg Strauss syndrome. This is a different pattern disease to Wegener's disease, it's asthma associated with peripheral eosinophilia, and perhaps nerve, skin, and cardiac involvement. And it's a rare cause of patients with difficulty to control asthma. 02:38 Occasionally there'll to be lung infiltrations as well which is the one way where you can recognize a patient may have this disease rather than just plain asthma because the X ray does not share infiltration in asthma by itself. 02:52 And the last disease is anti-glomerular basement membrane antibody disease, used to be called Goodpasture's syndrome. This is very, very rare indeed, presents with pulmonary hemorrhage and kidney involvement, it’s a characteristic kidney and lung problem with acute issues affecting both. So to summarize the main learning points of this lecture on vascular disease; PEs are common, they affect all ages and they need to be considered the differential diagnosis of patients presenting with many different lung diseases whether it is acute or chronic. Massive PEs cause cardiac arrest and shock and are significant cause of sudden death. Medium-sized PEs are more readily recognizable, they present acutely with haemoptysis, pleuritic chest pain, and breathlessness. The most difficult one to diagnose is probably multiple small pulmonary emboli because this presents similarly to pulmonary hypertension with chronic progressive dyspnea, and can be confused as other causes of chronic progressive dyspnea, and it does require specific tests to be identified, the echocardiogram for example. If you want to identify a PE, the best method nowadays is this CT pulmonary angiography. This can rapidly identify the presence of large and medium clots, and also can identify the small clots that cause chronic PEs in many patients as well. If somebody has pulmonary emboli, they need to be treated by anticoagulation, acutely with low molecular weight heparin, and then long-term with oral anticoagulants such as warfarin, either for a short period of time if there is a known cause for the PE, or forever if they have no repeated pulmonary emboli or a cause that isn't known to recur. 04:31 Pulmonary hypertension is usually a secondary problem to chronic lung disease or chronic cardiac disease. So chronic hypoxic lung disease causing pulmonary hypertension is called cor pulmonale, and the main treatment for that is long-term oxygen therapy, and diuretics for any oedema that develops as a consequence of the right heart strain. In contrast, primary pulmonary hypertension is relatively rare, but it is very difficult to recognize and has a poor prognosis and it can affect young people and is therefore, very important to identify as soon as it can be and you need a high index of suspicion to identify these patients and make sure they get the specialist investigations, and care that is required. 05:11 Thank you for listening.
About the Lecture
The lecture Pulmonary Vasculitis by Jeremy Brown, PhD, MRCP(UK), MBBS is from the course Pulmonary Vascular Disease.
Included Quiz Questions
A patient with severe COPD presents to the hospital with marked peripheral edema to the upper thigh and a raised jugular venous pressure. Management should NOT include which of the following options?
- Diuresis to achieve a fluid imbalance (output - input) of > 1 L/day
- Diuresis to achieve a fluid imbalance (output - input) of ≤ 500 mL/day
- Correction of hypoxia
- Restriction of dietary salt intake
A 60-year-old man presents with hemoptysis and a cavitary mass on chest X-ray. Which of the following diseases would NOT be considered in the differential diagnosis?
- Mesothelioma
- Granulomatosis with polyangiitis
- Tuberculosis
- Lung cancer
Which antigen is associated with granulomatosis with polyangiitis?
- Anti-neutrophilic cytoplasmic antibodies (cANCA)
- Myeloperoxidase or pANCA
- HMG1
- Alpha-enolase
- Catalase
Which vasculitis typically involves the heart as well as the lungs?
- Eosinophilic granulomatosis with polyangiitis
- Granulomatosis with polyangiitis
- Goodpasture syndrome
- Anti-glomerular basement membrane antibody disease
- Wegener granulomatosis
Patients with multiple small pulmonary embolisms often present with which of the following signs and symptoms?
- Chronic progressive dyspnea
- Hemoptysis
- Shock
- Sudden death
- Cardiac arrest
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Clearly presented, without redundant details. It helps a practising physician refresh their knowledge and organize it.