Playlist
Show Playlist
Hide Playlist
Primary and Secondary Amenorrhea
-
Slides Reproductive Endocrine Disorders.pdf
-
Reference List Endocrinology.pdf
-
Reference List Reproductive Endocrine Disorders.pdf
-
Download Lecture Overview
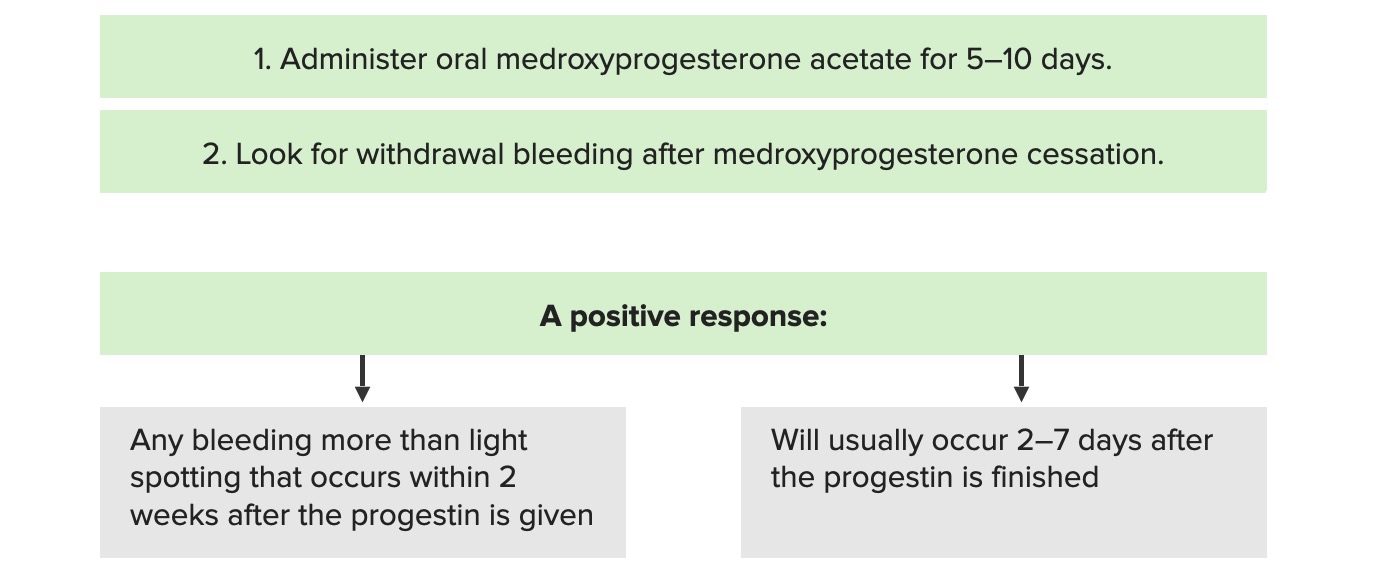
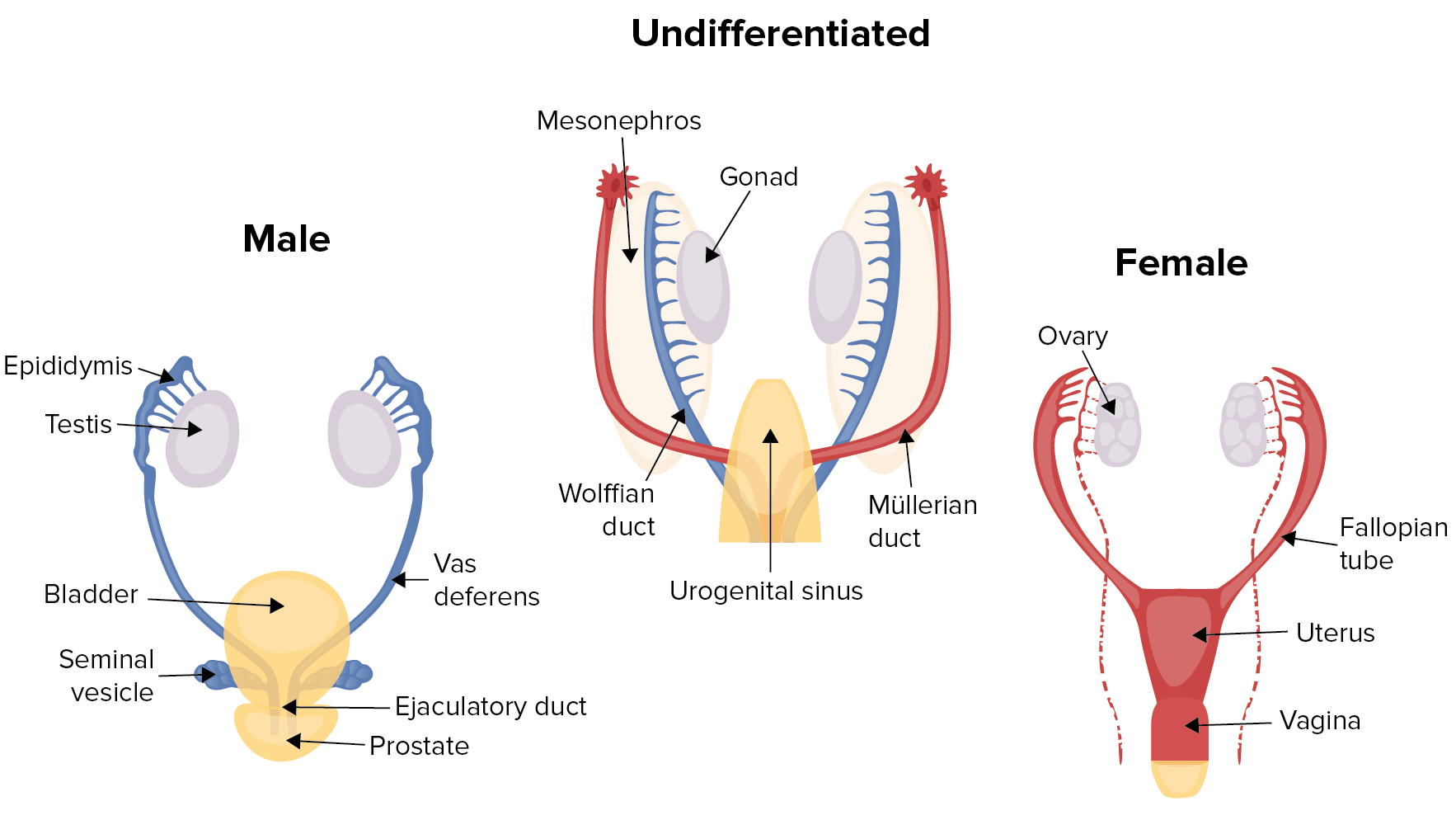
00:01 Primary amenorrhea is the absence of menses at age 15 in the presence of normal growth and secondary sexual characteristics as occured in this case. 00:11 Primary amenorrhea is most commonly caused by genetic or anatomic abnormality. 00:17 A genetic abnormality in 50% of cases and an anatomic abnormality in 15%. 00:23 The most common cause is gonadal dysgenesis, most commonly with Turner syndrome as seen in our case. 00:30 This occurs in 1 in 2500 live female births. 00:36 Treat these patients with exogenous estrogen therapy with cyclic progestin to prevent endometrial hyperplasia and continue this until age 51, the average age of menopause. 00:48 The anatomic abnormalities are much less common, occuring in 15 percent of cases. 00:53 And this will include an intact hymen, a transverse vaginal septum or vaginal agenesis otherwise known as Mullerian agenesis or Mayer-Rokitansky-Kuster-Hauser syndrome. 01:06 This happens to be the second most common cause of primary amenorrhea but it's far less common than Turner syndrome. 01:13 The incidents here is 1 in 5,000 live female births. 01:17 Normal female karyotype in ovarian function and thus normal external genitalia and secondary sexual characteristics. 01:28 Secondary amenorrhea is the absence of menses for more than 3 months in women who previously had regular menstrual cycles or 6 months in women who have irregular menses. 01:40 Disruption of the hypothalamic pituitary ovarian axis is the most common cause of secondary amenorrhea after pregnancy. 01:48 Hyperprolactinemia accounts for 10-20% of non pregnancy mediated amenorrhea. 01:55 Polycystic ovary syndrome is by far, the most common hyperandrogenetic cause of secondary amenorrhea. 02:03 Asherman syndrome or intrauterine adhesions are the only uterine cause of secondary amenorrhea. 02:10 Asherman syndrome should be suspected in those patients who had prior dilatation and curettage of the uteruses with a maybe some form of injury where fibrous adhesions have formed and obliterated the central core of the uterus preventing adequate menses. 02:29 There is an algorithm for the evaluation of amenorrhea. 02:33 When amenorrhea is present, particularly secondary amenorrhea, obtain a serum HCG level to exclude the presence of pregnancy. 02:41 If it is positive and the patient is pregnant, you have your diagnosis. 02:46 On the other hand, if it is negative, a more substantial endocrine work-up is warranted. 02:51 One would start by obtaining a follicle stimulating hormone, a TSH, a free T4 and a prolactin. 02:59 Starting with prolactin, if prolactin is elevated, always repeat it to confirm it's positivity and review the list of medications that the patient is on. 03:08 Also, if those are negative, consider obtaining a pituitary MRI to rule out the presence of a prolactinoma. 03:18 When the TSH is abnormal, it implies underlying thyroid disease and one then should go on and evaluate further for thyroid dysfunction. 03:26 With regards to FSH, if the FSH is elevated, one should then go on and obtain a karyotype and consider primary ovarian insufficiency as was the case with our patient with Turner syndrome. 03:40 On the other hand, if the FSH is low or normal, one should then proceed with progesterone withdrawal testing. 03:48 Under these circumstances, the patient is given a dose of progesterone for a certain number of days. 03:53 When the progesterone is stopped, when the patient stops taking the progesterone, they essentially withdraw from it and one hopes to invoke a withdrawal bleed. 04:04 However, if no bleeding is present with progesterone withdrawal and the patient has headaches or temporal vision loss, obtain a head MRI again to rule out pituitary course for the amenorrhea. 04:18 Also consider a eating disorder or excessive exercise or stress in the case of patients who do not undergo progesterone withdrawal bleeding. 04:28 If there is a history of gynecologic procedures, also consider hysteroscopy to evaluate for uterine adhesions or Asherman syndrome. 04:39 If the patient bleeds with progesterone withdrawal, then consider hyperandrogenism. 04:44 Obtain a testosterone level, a dehydorepiandosterone level and a 17-hydroxypregesterone test. 04:51 These patients tend to have polycystic ovary syndrome and this is probably the most common cause of hyperandrogenism leading to secondary amenorrhea.
About the Lecture
The lecture Primary and Secondary Amenorrhea by Michael Lazarus, MD is from the course Reproductive Endocrine Disorders. It contains the following chapters:
- Primary Amenorrhea
- Secondary Amenorrhea
- Evaluating Amenorrhea – Algorithm
Included Quiz Questions
What is the most common cause of primary amenorrhea?
- Turner syndrome
- Down syndrome
- Asherman syndrome
- Fragile X syndrome
- Marfan syndrome
What is the most common hyperandrogenic cause of secondary amenorrhea?
- Polycystic ovary syndrome
- Primary ovarian insufficiency
- Uterine fibroids
- Endometriosis
- Asherman syndrome
What is the first step in the evaluation of amenorrhea?
- Serum hCG
- FSH
- TSH & free T4
- Prolactin
- Brain MRI
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |