Playlist
Show Playlist
Hide Playlist
Polyenes – Antifungals
-
Slides Polyenes Antifungals.pdf
-
Reference List Pharmacology.pdf
-
Download Lecture Overview
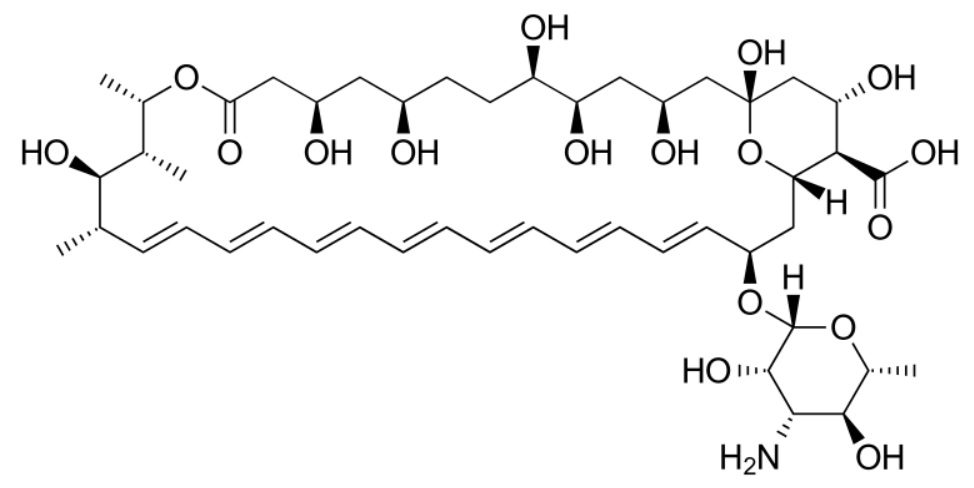
00:00 Let's take a look at some other classes of drugs that are used to treat fungal infections. 00:06 The polyenes, nystatin being the prototypical drug is used for superficial infections. 00:11 You can see where it acts on the cell wall down here. 00:14 It's used topically to suppress candida infections. 00:18 And it's used as "swish and swallow" for oral candidiasis. 00:22 The mechanism of action, remember that these polyene antifungal agents bind to ergosterol and caused artificial pores in the cell membrane. 00:34 This causes leakage of hydrogen ion, potassium ion, chloride ion and even sodium ion through that pore. 00:41 It also increases free radical formations within the cell itself which causes toxic intermediates inside the cell. 00:50 And causes fungal cell death. 00:54 The next polyene I want to talk about is amphotericin B. 00:57 And you'll notice that the slide is almost is exactly the same as nystatin. 01:02 Now these polyenes binds to ergosterol and caused artificial pores. 01:07 And once again as with the nystatin, it leaks hydrogen, potassium, chloride and sodium ions through this pore. 01:14 And you also have free radical formation within the cell that causes toxicity inside the fungal cell and cell death. 01:22 Now amphotericin B is a polyene and it is related to nystatin. 01:27 But it's usually intravenously administered. 01:30 Nystatin is usually what we call topical. 01:33 And so it's gargling kind of an agent that we use in oral candidiasis. 01:39 Amphotericin B is an intravenous drug and it's used for much more serious infections. 01:44 It's eliminated through the slow hepatic metabolism of it. 01:48 And it's half life is therefore quite long, 2 weeks. 01:52 It has minimal renal excretion. 01:54 But we do make small adjustments to this medication in class 4 or stage 4 renal failure. 01:59 Clinically we use it for systemic mycoses. 02:03 And usually ones that are fairly serious. 02:05 It's the widest antifungal spectra of any antifungal agent on the market. 02:11 It works against aspergillosis. 02:12 It works against blastomycosis. 02:15 It works against candida, cryptococcosis, histoplasmosis and mucor. 02:22 It also used intravenous or rarely intrathecally. 02:27 I have seen it used intrathecally once in my career. 02:30 Now mycotic corneal ulcers and keratitis are one of the potential treatments of that we can use amphotericin B for. 02:39 Now in terms of the toxicity of this medication, the most interesting thing that I've seen with this agent is, infusion related chills. 02:49 So patients suddenly start feeling very cold and -- I don't really have an explanation as to why that's occurring. 02:56 Patients will also have nausea, muscle spasms and vomiting. 02:59 And sometimes patients will have this shock like fall in blood pressure. 03:05 So a lot of time we will premedicate these patients with antihistamines or even glucocorticoids. 03:11 You have to be very aware that ampho B can cause renal tubular acidosis. 03:16 And can cause magnesium wasting and potassium wasting. 03:19 Now the magnesium and potassium wasting are kind of coming hand in hand. 03:23 Most of the time when you have magnesium wasting, you're also going to have potassium wasting. 03:28 The other toxic effects include anemia. 03:32 That's usually due to decreased erythropoietin production from the kidney. 03:37 You can have those nephrotoxic effects. 03:40 These are usually dose limited however. 03:42 Now we have a liposomal version of amphotericin B. 03:47 These amphotericin B liposomes package the amphotericin B on the inner surface or on the inside of these liposomes or I should say endozomes. 03:59 And the reduce renal toxicity, we call that lysosomal amphotericin B or liposomal amphotericin B. 04:08 The correct term is actually liposomal. 04:10 We do give intrathecally this medication but it is associated with seizures in neurologic damage. 04:18 So that is a treatment that we try to avoid unless we're really in trouble.
About the Lecture
The lecture Polyenes – Antifungals by Pravin Shukle, MD is from the course Antimicrobial Pharmacology.
Included Quiz Questions
What is NOT a similarity between nystatin and amphotericin B?
- They are both administered intravenously.
- They both bind ergosterol.
- They are both polyenes.
- They both increase free radicals in the cell.
- They both cause artificial pores in the fungal cell wall.
What is a primary indication for nystatin administration?
- Swish and swallow for oral candidiasis
- Intrathecal administration for mycotic meningitis
- Combined with a steroid for topical tina cruris infections
- Topical application for dermal fungal infections
- Intravenous administration for systemic mycoses
What is an amphotericin B toxicity?
- Anemia
- Keratitis
- Lymphedema
- Salt wasting
- Cartilage damage
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |