Playlist
Show Playlist
Hide Playlist
Polycystic Ovarian Disease (PCOS)
-
Slides Ovary Female Repro.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
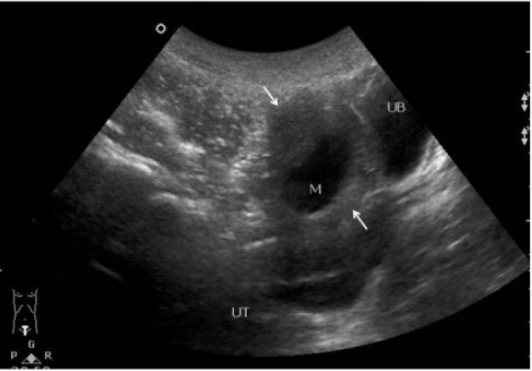
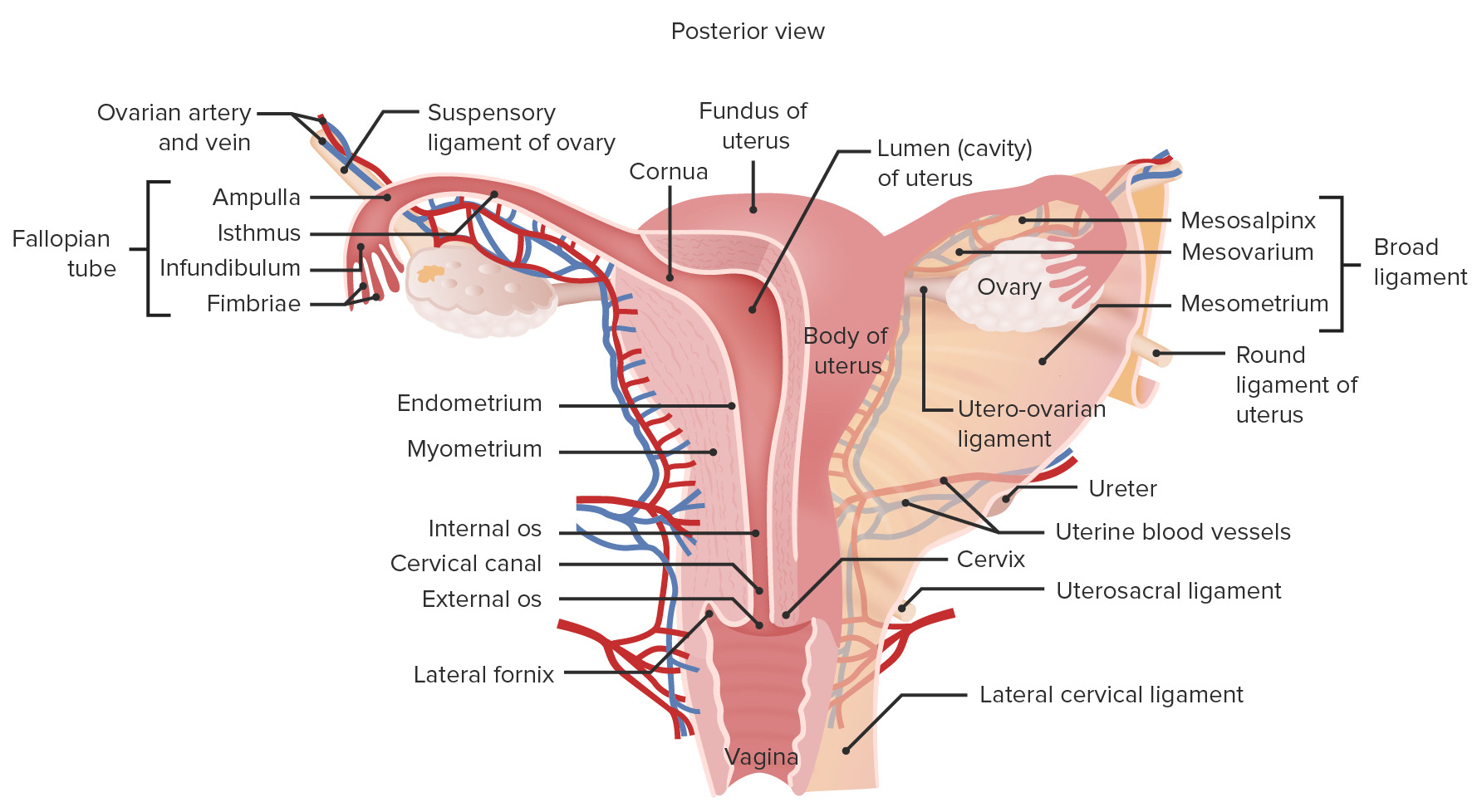
00:01 Our topic here is polycystic ovarian disease. 00:05 What then happens here is you may have cyst in the ovary. 00:08 Notice I said “may”. 00:10 It’s amazing that this condition is known as polycystic ovarian disease in current day practice but the criteria, you don’t even have to have a cyst in the ovary. 00:20 So what do you have to have in polycystic ovarian disease? Let’s take a look and more importantly, who’s your patient walking through that door? Oligomenorrhea with the multiple follicular cysts. 00:35 Multiple follicular cysts. 00:37 So there’s a possibility that the ovaries are going to contain this follicular cyst that we just talked about. 00:43 I’ll walk you through the pathogenesis of it. 00:45 But remember, I’m telling you now, current day practice, you don’t necessarily have to have follicular cysts. 00:52 That could be one of the criteria. 00:54 Another criteria might be oligomenorrhea. 00:57 You’ll have a thickened ovarian capsule. 01:01 Multiple small cysts are possible. 01:04 And you’ll have cortical stromal fibrosis. 01:07 All of this is then going to contribute to the oligomenorrhea. 01:12 What does that mean to you? That means that the time spent between the menses is much longer. 01:18 So if an average menses cycle, menstrual cycle was approximately 28 days, maybe now the female is having her menses once every 35 days. 01:28 Once every 40 days, right? Oligomenorrhea. 01:32 What’s your problem with polycystic ovarian syndrome? Let’s say a young woman with persistent anovulation, but yet she might actually have bleeding. 01:43 So what is exactly is taking place in polycystic ovarian disease and who’s your patient walking through the door? Well, since we’re doing female reproductive pathology that we have to then divide our gender into two variables. 01:58 Genotypic and phenotypic. 02:00 Genotypic and phenotypic. 02:01 From henceforth, whenever you do reproductive pathology, you pay attention to what the genotype of your patient is and what the phenotype of your patient is. 02:11 Trust me, that will come in quite handy. 02:14 Here, you’ll have a female, phenotypically, she is obese. 02:18 Genotypically, she is XX. 02:21 So no problems with the chromosome, but she is obese. 02:24 In addition, her walking through the door and she’s obese. 02:29 You see that she has a mustache. 02:31 In other words, she has man hair-like distribution. 02:35 What is this called when there is male-like hair distribution in a female? It’s called hirsutism. 02:41 Obese, hirsutism. 02:45 How is that hirsutism taking place? Well, there must be increased -- can we say male-like hormone in that patient? Yeah. 02:54 So keep all of that in mind as we go through this. 02:57 Here are the two major, major clinical manifestations that you’d find or presentation, with obesity and hirsutism. 03:08 Now we get into pathogenesis. 03:11 You want to begin polycystic ovarian syndrome with what exactly I’m telling you. 03:17 Here, we’re going to begin with excess LH from the anterior pituitary. 03:22 That’s where you’re going to begin. 03:23 You have to. 03:24 because laboratory-wise, to confirm polycystic ovarian syndrome, you’re going to look for an LH that is going to be elevated. 03:32 In fact, when you do an LH and FSH ratio, you’ll find an LH to FSH ratio being 2:1 or maybe perhaps 3:1. 03:42 The point is LH is considerably elevated. 03:47 I need your help to recall the physiology of the follicle. 03:53 You ready? Here comes out the LH in excess from the anterior pituitary. 03:59 It’s going to enter circulation. 04:02 Would you please follow me through to the ovary where it’s going to work upon the follicle? And the LH then works upon which follicular cell? Is it going to be the granulosa cell? Or is it going to be the theca cell? Good. 04:22 It will be the theca cell. 04:24 The theca cell is responsible for producing – take the T in theca and it’s going to produce T – testosterone. 04:34 Who’s your patient? Phenotypically an obese female who is “hirsitized”. 04:40 And, number two, genotypically, she’s a female. 04:44 She has a lot of testosterone. 04:46 Oh. 04:48 So that’s going to give you the androgen effect in that female. 04:51 What kind of effect? I told you about the hirsutism, maybe she has acne too. 04:56 So more masculinization, right? Keep going please. 05:01 So your patient has increased LH. 05:04 As you know, the theca cell produces testosterone. 05:07 Lots of that. 05:09 And she’s obese. 05:10 Hmm. 05:11 Do you know a method in biochemistry that converts your testosterone into estrogen? Sure you do. 05:19 What’s the name of that enzyme and what’s the name of the process? The enzyme’s called aromatase and the process is called aromatization. 05:26 Correct? So all of these excess LH, producing too much testosterone. 05:32 Well, a lot of conversion to estrogen. 05:36 We used this before. 05:38 All this estrogen is a risk factor for what kind of cancer? Endometrial cancer. 05:44 You’re taking a look at the labs and you want to answer the question quickly. 05:47 What are you going to look for? All labs are elevated, the LH will be elevated, testosterone will be elevated, estrogen will be elevated. 05:54 Move on. 05:56 Because of obesity, what is that going to do with the insulin receptors? It makes it resistant to the insulin. 06:03 And not only is she walking in and is she obese, not only will she have perhaps hirsutism, but maybe underneath the armpits and such, she has acanthosis nigricans. 06:14 You check out her lab for glucose and you find it to be elevated, diabetes mellitus. 06:19 You understand this? You’re in good shape for polycystic ovarian syndrome. 06:23 Here, we have an image of an ovary with multiple cysts. 06:26 Remember that with polycystic ovarian disease, that cysts are not even required as a criteria. 06:32 It could be of course. 06:33 Oligomenorrhea is something that you’re very much paying attention to and the clinical presentation that we talked about with obesity, hirsutism and diabetes mellitus. 06:42 Now real quick. With polycystic ovarian syndrome from pharmacology, because you’ve dealt with polycystic ovarian syndrome quite a bit with pharm, but really the next step of management is going to be – what do you think? Your patient walked in through the door and she is obese. 07:00 And you know that adipocytes have what enzyme in them? Aromatase. 07:05 And you know that she has lots of estrogen. 07:08 So don’t you think it would be a good idea for your first recommendation to lose weight, right? Lose weight. 07:15 Then you start thinking about using those drugs. 07:18 Low dose, maybe oral contraceptive pills. 07:20 Maybe leuprolide, spironolactone, so on and so forth. 07:24 Important.
About the Lecture
The lecture Polycystic Ovarian Disease (PCOS) by Carlo Raj, MD is from the course Ovarian Diseases.
Included Quiz Questions
Which of the following is a common presentation in women with polycystic ovarian syndrome?
- Oligomenorrhea, obesity, and hirsutism
- Amenorrhea, generalized hair loss, and weight gain
- Repeated ectopic pregnancies and chronic pelvic pain
- Fatigue, body aches, and menorrhagia
- Alopecia, dysmenorrhea, and weight loss
If an ovary from a woman with confirmed polycystic disease is examined microscopically, which of the following features is she MOST likely to have?
- Thickened ovarian capsule, multiple small cysts, and cortico-stromal thickening
- Multiloculated cysts filled with mucin
- Increased vascularization, thin capsule, and degenerated ovarian follicles
- Scarred ovarian capsule, increased stromal fibrosis, and absence of ovarian follicles
- Normal capsule and stroma, with multiple cysts containing ectodermal, mesodermal, and endodermal remnants
Which of the following hormone ratios is MOST likely to be increased in a patient with PCOS?
- LH to FSH
- FSH to LH
- Glucagon to insulin
- Growth hormone to insulin
- Progesterone to estrogen
A young woman diagnosed with PCOS asks her gynecologist about the risks associated with the disease. What should the doctor tell her?
- PCOS increases the risk of infertility, diabetes mellitus, and is associated with an increased risk of endometrial cancer.
- PCOS increases the risk of PID and endometrial hyperplasia.
- PCOS increases the risk of ectopic pregnancy, leiomyoma, and leiomyosarcoma.
- PCOS increases the risk of Sheehan syndrome, infertility, and hyperemesis gravidarum.
- PCOS increases the risk of ovarian and cervical cancers.
Customer reviews
3,5 of 5 stars
| 5 Stars |
|
3 |
| 4 Stars |
|
1 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
2 |
Bravo! Perspective is everything. Helped reinforce the information I have received before with greater clarity and understanding.
Very concise approach and explanation of PCOS. Thank you Dr Raj
Love it, short and totally relevant, Excelent to have a general review of such a complicated pathology
Bridges gaps, uses pharm, mentions PE and how metabolic syndrome predisposes.