Playlist
Show Playlist
Hide Playlist
Pheochromocytoma – Adrenal Medulla
-
Slides AdrenalMedulla EndocrinePathology.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
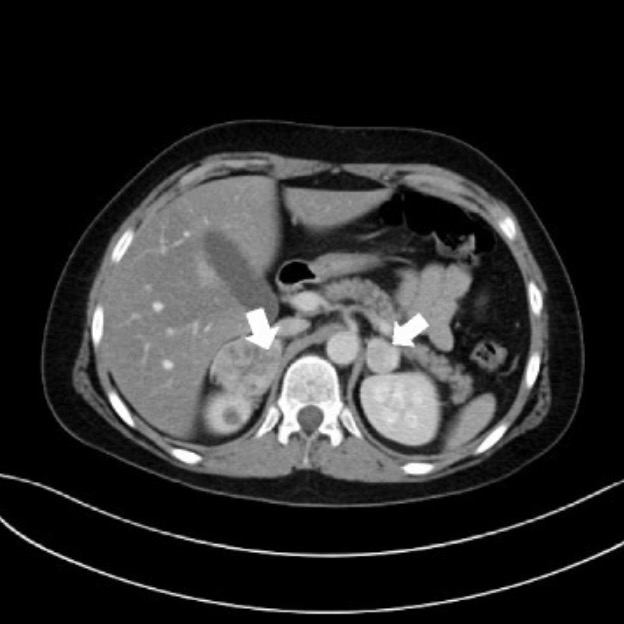
00:01 Let’s get into pathology. 00:04 Inside the medulla, you have a benign tumour. 00:08 This benign tumour episodically might then be releasing epinephrine. 00:13 When you increase your epinephrine, what happens? You’re going to have increased blood pressure for reasons we’ve talked about. 00:19 Beta-1 receptor activity increasing your heart contractions, increases systolic blood pressure. 00:26 Uncommon neoplasm, but my goodness, do you want to know this for your boards. 00:30 These are your medulla chromaffin cells. 00:33 Whenever you have... now, for board purposes know this… clinically speaking, in medicine, the term or the concept of paraganglioma is actually quite complicated. 00:43 I will give you the-the absolute minimum or what’s necessary for you to get the questions right here, but if you find a-a epinephrine producing tumour outside the adrenal medulla, then you call this a paraganglioma. 01:00 When from extra adrenal chromaffin cells, the operative word extra, this is then referred to as being paraganglioma. 01:10 So, where would this be located if it’s not in the adrenal medulla? Bifurcations, of what? Bifurcations of blood vessels such as the carotids up here, internal/external bifurcation of the carotid artery and then the iliacs. 01:27 Pheochromocytoma, reaction with dichromate fixation helps you… you want to know about a particular staining mechanism. 01:35 Tumours of the adrenal medulla generally may be sporadic associated with inherited… we’ll talk about this in great detail. 01:43 Including neurofibromatosis type I, we’ll talk more about neurofibromatosis type I in neuropathology in which then gives rise to a particular type of brain issue called neurofibroma all associated with and you must know of von Hippel-Lindau disease. 01:59 Von Hippel-Lindau disease is extremely important for you and I in pathology because of its molecular mechanisms including something called hypoxia-inducible factor 1-alpha and the fact that it works on your VEGF. 02:12 If you’re not familiar with any of that, this would probably be a good time to go back and take a look at the chapter neoplasia that we are… that we have covered and in which I’ll walk you through in great detail about increasing-increasing your effect and influence of VEGF in a cancer with Von Hippel-Lindau in which you have bilateral renal sarco… or cancer. 02:32 Succinate dehydrogenase submit gene mutation and MEN 2 syndromes. 02:37 Why did I emphasise “es”? Because it’s part of both MEN2A and 2B. 02:44 What is pheochromocytoma? So, earlier when we began this section, I told you the medulla and the pathology of it is not to be underestimated because of its incredible links to other subjects - biochemistry, physiology, pathology and other pathologies and its associations that we’ve already had discussions, but you must bring all of it together now. 03:06 Epinephrine/metanephrine predominates suggests MEN2A and 2B; bilateral tumours, familial history, young age or paragangliomas such as genetic syndromes. 03:20 What’s paraganglioma? Think about it as being a pheochromocytoma… extra adrenal. 03:26 Where is it located? Bifurcations maybe the iliacs and maybe the carotids. 03:31 Correctable, meaning to say that the hypertension here is not constitutive, what that means is that the hypertension is not going to be continuous. 03:42 This is pheochromocytoma, your focus here episodic hypertension. 03:51 Presentation and Diagnosis: triad… headaches, sweating, palpitations during the episodes. 04:00 Anxiety, nervousness to the point where feels like impending death by the patient; severe tremors, pain in the lower chest, upper abdomen all due to increased sympathetic activity. 04:14 Nausea, weight loss, heat intolerance, incredibly high levels of epi, epi, epi, epi… increasing everything. 04:24 About half will have what’s known as paroxysmal hypertension, meaning to say that it’s refractory, it will not pay attention, or should I say, it will not respond to conventional medication. 04:34 Hence, you get into interesting drugs such as phenoxybenzamine. 04:40 Most others appear to have essential hypertension. 04:43 Presentation and diagnosis is important for you to pay attention to. 04:47 There is no sign that is a best test, do not look for buzz words; most common however will be the fact that you’re going to look for your metanephrines 24 hours. 04:57 You’ve heard of vanillylmandelic acid… plasma free metanephrines. 05:04 The metabolites are more sensitive than parent catecholamines… the metabolites of epi. 05:12 Always confirm a biochemical test. 05:14 However, before doing any imaging study, and I have emphasized that throughout this entire lecture series, always look for biochemical test before doing imaging. 05:25 Next step of management with imaging MRI’s preferred. 05:27 Once you do an MRI of the abdominal region, you will then notice that there is a tumour in the adrenal gland specifically in the medulla, but you correlate this please first with diagnosis. 05:40 Meaning to say that your labs that were showing the metanephrines and the vanillylmandelic acid in the urine. 05:48 If the MRI is unrevealing then you might be thinking about using radioactive diagnosis and this brings us to MIBG scintigraphy which is meta… M, iodo… I, benzo… B, guanidine. 06:09 There is something called the rule of 10’s or the rule of 10 percent of pheochromocytoma, it is important that you know these. 06:17 Majority of your pheochromocytomas are benign, non-malignant… 10 percent are. 06:25 Majority of your pheochormocytomas are unilateral, 10 percent are bilateral. 06:31 Majority of your pheochormocytomas are in your adrenal medulla, 10 percent might be extra adrenal… welcome to paraganglioma. 06:40 Majority of your pheochormocytomas are in adults, 10 percent might be in children. 06:45 Majority of them are sporadic, 10 percent might be familial… put familial and paraganglioma together. 06:52 10 percent are associated with MEN2A and or 2B; 10 percent may recur… 10 percent rules of pheochromocytoma. 07:05 Treatment consists of surgically excision of the tumour, remove the darn tumour. 07:11 Since surgery can precipitate catecholamine release from the tumour, patients are prepared with your phenoxybenzamine so that you would do what? Control, control, control your blood pressure. 07:23 That is what’s most important. 07:24 I don’t care what kind of surgery that you’re doing, you want to make sure that your patient is not in a state of bleeding and definitely controlling his or her blood pressure, right? Absolutely. 07:36 Prior to operation, beta blocker prior to alpha blocker should be avoided as it may lead to severe hypertension due to unopposed alpha adrenergic activity. 07:49 Patients with large pheochromocytoma increase risk of malignancy, remember 10 percent could be malignant or paraganglioma… once again malignancy. 07:59 These individuals should then undergo the MIBG scintigraphy… metaiodobenzylguanidine. 08:08 The sporadic is the majority of our type, that is where our focus here is, 90 percent, ages 40-60; 10 percent will… 10 percent bilateral, 10 percent malignant. 08:20 Hereditary form important, important associations. 08:24 Childhood, males, bilateral, von Hippel-Lindau, what does that mean to you? Renal carcinoma… automatically renal carcinoma. 08:36 What if your patient is ataxic as a gait? Good, hemangioblastoma in the cerebellum. 08:42 What if there’s visual issues? Hemangioblastoma in the retina. 08:47 Sturge-Weber… child… half the face is red, right? Called as port wine stain, could have… that child might have neo onset seizures because of space occupying lesions due to what’s known as leptomeningeal arteries. 09:03 You can have neuroblastomas that are associated and we will get into 2A and 2B in just a little bit.
About the Lecture
The lecture Pheochromocytoma – Adrenal Medulla by Carlo Raj, MD is from the course Adrenal Gland Disorders.
Included Quiz Questions
A patient presents with a tumor consisting of chromaffin cells at the bifurcation of the carotid artery. What is the most likely diagnosis?
- Paraganglioma
- Wilms' tumor
- Metastatic tumor with lung origin
- Adrenal carcinoma
- Adrenal adenoma
Which disorder is NOT associated with pheochromocytoma?
- Tuberous sclerosis
- Neurofibromatosis type 1
- Von Hippel-Lindau disease
- Succinate dehydrogenase subunit gene mutation
- MEN2 syndrome
What is NOT a common symptom of pheochromocytoma?
- Lethargy
- Palpitations
- Headache
- Tremors
- Sweating
What are the characteristics of hypertension produced by pheochromocytomas?
- Paroxysmal/episodic
- Higher in arms than legs
- Consistently above 160/110 mm Hg
- Responds rapidly to diuretics
- Accompanied by a drastic increase in renin
What is NOT a part of the "Rule of 10s"?
- 10% unilateral
- 10% malignant
- 10% familial
- 10% extra-adrenal
- 10% of cases in children
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |