Playlist
Show Playlist
Hide Playlist
Pathogenesis of Diabetes Mellitus – Hyperglycemia
-
Slides HyperglycemiaDiabetesMellitus EndocrinePathology.pdf
-
Reference List Pathology.pdf
-
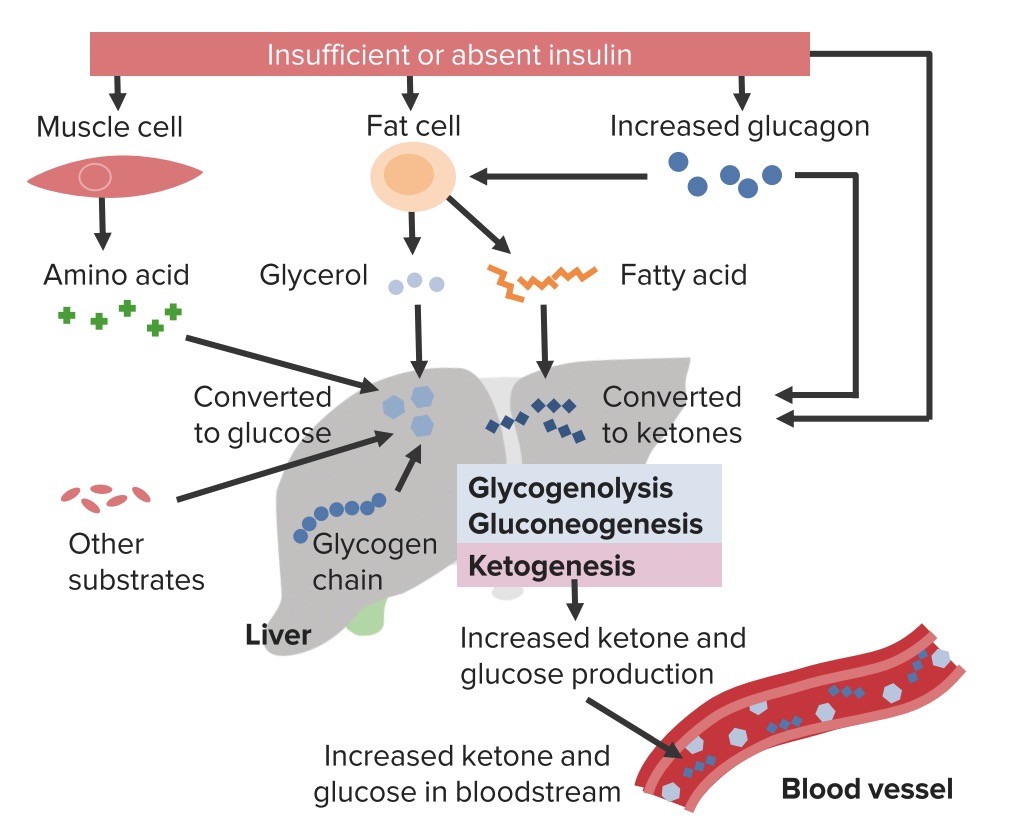
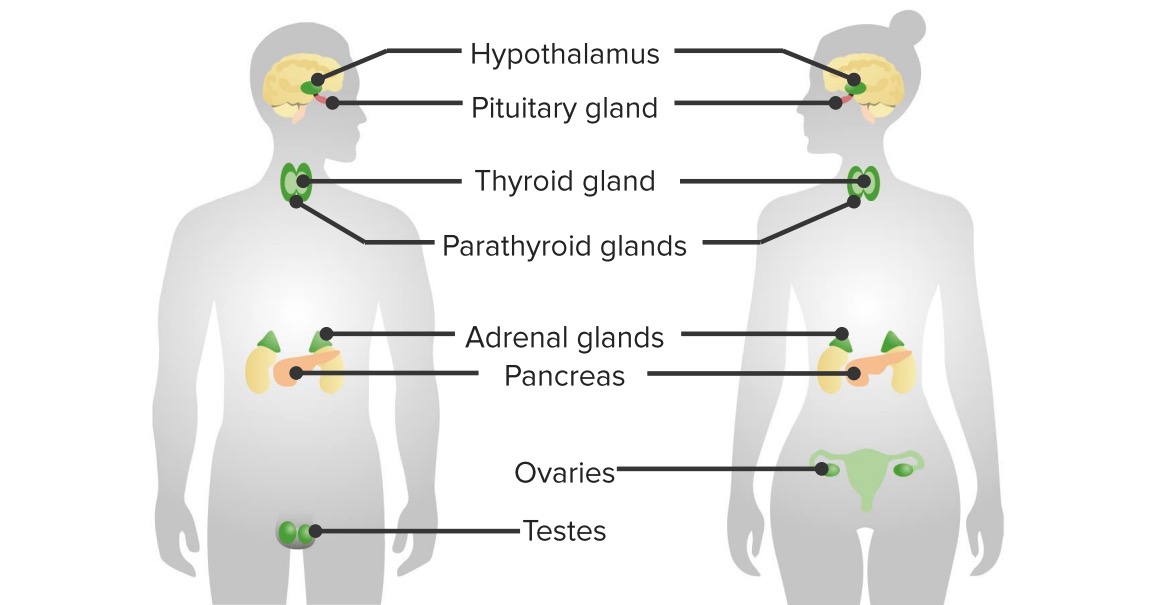
Download Lecture Overview
00:00 Let’s start with a brief overview of the different types of diabetes. 00:06 Type 1 Diabetes Mellitus (DM) accounts for 5-10% of all diabetes cases. 00:14 It is primarily immune-mediated, which means that the body's immune system mistakenly attacks and destroys the insulin-producing beta cells located in the islets of Langerhans of the pancreas. 00:27 Although Type 1 DM most commonly becomes apparent in childhood or young adulthood, it's important to recognize that it can occur at any age. 00:36 Latent autoimmune diabetes in adults is a slowly progressive variant of type 1 DM. 00:43 Patients with Type 1 DM typically have detectable autoantibodies, which include: Insulin Autoantibodies Glutamic Acid Decarboxylase Antibodies Insulinoma-Associated-2 Autoantibodies Zinc Transporter 8 Autoantibodies Beyond these autoantibodies, cellular immunity is also believed to play a significant role in the pathogenesis of this condition. 01:10 A small subset of Type 1 DM is categorized as idiopathic, meaning that it has no known cause. 01:16 Type 2 Diabetes Mellitus represents about 90% of diabetes cases. 01:22 It typically develops in adulthood but is increasingly seen in younger individuals, largely due to the rising rates of obesity. 01:31 Type 2 DM develops over many years and often begins with insulin resistance, where the body's cells do not respond effectively to insulin. 01:40 Management of Type 2 DM generally involves: Lifestyle changes such as diet and exercise Oral medications to improve insulin sensitivity or increase insulin secretion In some cases, insulin therapy may be necessary if other treatments do not adequately control blood sugar levels. 02:02 Other types of Diabetes Mellitus make up less than 5% of cases: Genetic forms of diabetes, such as MODY, are caused by mutations in single genes and often run in families. 02:16 Diseases of the exocrine pancreas, such as pancreatitis, and endocrinopathies, like Cushing's syndrome, can lead to secondary diabetes. 02:27 Drug or chemical-induced diabetes can result from treatments such as steroids or after organ transplantation. 02:34 Infections and uncommon forms of immune-mediated diabetes, although rare, can also lead to diabetes. 02:42 Other genetic syndromes such as Down Syndrome, may be associated with an increased risk of diabetes. 02:49 Gestational Diabetes Mellitus, which occurs during pregnancy. 02:54 While it usually resolves after giving birth, it does increase the risk of Type 2 DM later in life for both the mother and the child. 03:04 Now, we’ll talk about the pathogenesis, this is the most important. 03:08 It's called non-enzymatic glycosylation. What does that mean? With all that glucose that’s circulating it will then bind to protein, it will cause and wreak havoc up and down the body through depositing in the capillary membrane. 03:23 When it does so, it will cause arteriosclerosis. 03:27 If it's in the capillary, it will then cause non-enzymatic glycosylation and therefore compromise proper exchange of nutrients. 03:37 Altered carbohydrate metabolism and a second pathogenesis here is that you wanna know about sorbitol and that’s because with all that glucose, instead of going to the glycolytic pathway, it might end up going through what's known as aldose reductase. 03:53 With that aldose reductase in sorbitol specifically in the lens, remember what I told you if you started with a patient with diabetes over a long period of time, what color could their lens be? In Greek, cataract means waterfall. 04:06 When you take a look at the waterfall, what color is that water when it's falling over the cliff? Opaque and white. 04:13 That’s what cataract means in Greek, you find whiteness over the lens that’s because sorbitol accumulating in the lens is going to cause waterfall into the lens, in other words, increase osmotic pressure. 04:29 Unregulated glucose intake by this tissues partially explains why these are the main diabetes mellitus targets. 04:39 The increase glucose metabolized by the enzyme aldose reductase to sorbitol, that’s an important point, make sure that you pay attention to that enzyme. 04:50 Two major pathogeneses that I just walked you through, the most important will be non-enzymatic glycosilation, neg, or you might have heard of AGE, advanced glycosilated end-product - one and the same. 05:04 Capillary membrane destruction, remember the arteriosclerosis that you found with diabetes that’s called hyaline atherosclerosis and do not forget about the sorbitol pathogenesis. 05:16 Quickly type 1 versus type 2, a brief beautiful summary of the things that you would look at in your head now, you should have a firm understanding as to why these things are taking place. 05:28 Type 1, weight please - normal or thin, type 2, overweight. 05:34 First step of management, type 2 diabetic lose the weight. 05:39 Age: Type 1, young - by young we mean still less than 20 or 30, about 22-23 but usually, younger but you never know. 05:50 Remember the other differential that you wanna keep in mind called unconventional or MODY in which it’s called Maturity onset of Diabetes in the young, in which I told you to focus upon a deficiency in glucokinase gene. 06:04 If its type 2, a little bit older, 30, obese, insulin resistance. 06:11 Type 1, with glycemic pattern all over the place because of insulin pump, type 2, less variable. 06:15 Type 1, with glycemic pattern all over the place because of insulin pump, type 2, less variable. 06:17 Insulin sensitivity in type 1, perfectly normal hence the insulin pump. 06:23 In type 2, if the receptors aren't working how in the world is insulin even being properly responded to? Insulin sensitivity reduced in type 2. 06:35 What about oral agents? Only effective in type 2. 06:40 Antibiotic status. In type 1 remember the topic insulitis? I told you about your glutamic acid decarboxylase, a type 2 hypersensitivity that’s auto immunity. 06:56 So antibiotic status positive in type 1, negative in type 2. 07:01 Remember the autoimmune disease within the thyroid, the pancreas, and the adrenal, polyglandular endocrinopathy. 07:07 C-peptide level, undetectable in type 1. 07:12 High in type 2. 07:13 What does C-peptide mean to you? Endogenous production of insulin. 07:17 Family history - strong family history in type 2. 07:22 Other autoimmune disorders for sure in type 1 and I’ll walk you through all of these, your patients here tend to be more of females.
About the Lecture
The lecture Pathogenesis of Diabetes Mellitus – Hyperglycemia by Carlo Raj, MD is from the course Pancreatic Disease and Diabetes.
Included Quiz Questions
What is a difference between type 1 and type 2 diabetes mellitus?
- There is a stronger first-degree relative family history of disease in type 2 diabetes.
- The C-peptide level is low in type 2 diabetes and normal in type 1 diabetes.
- Autoimmune conditions are common for patients with type 2 diabetes but not in type 1 diabetes.
- Patients with type 1 diabetes are more often overweight than patients with type 2 diabetes.
- Insulin sensitivity is reduced in type 1 diabetes and increased in type 2 diabetes.
What is the pathogenesis of diabetic neuropathy?
- Unregulated glucose uptake leads to increased sorbitol and glycosylation of proteins.
- Capillary basement membrane thickening
- Arteriosclerosis
- Decreased level of aldose reductase
- Apoptosis in neurons
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |