Playlist
Show Playlist
Hide Playlist
Pathogenesis, Diagnostics and Clinical Manifestations – Infective Endocarditis
-
Slides Valvular Hypertensive Heart Disease.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
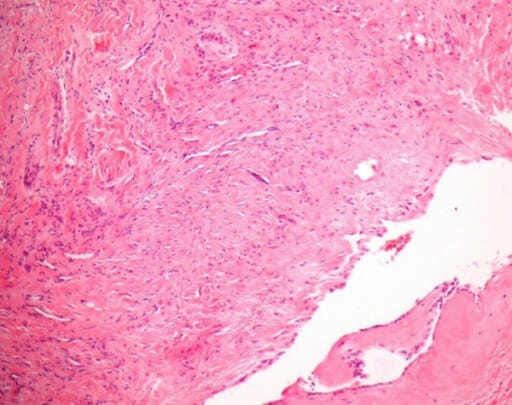
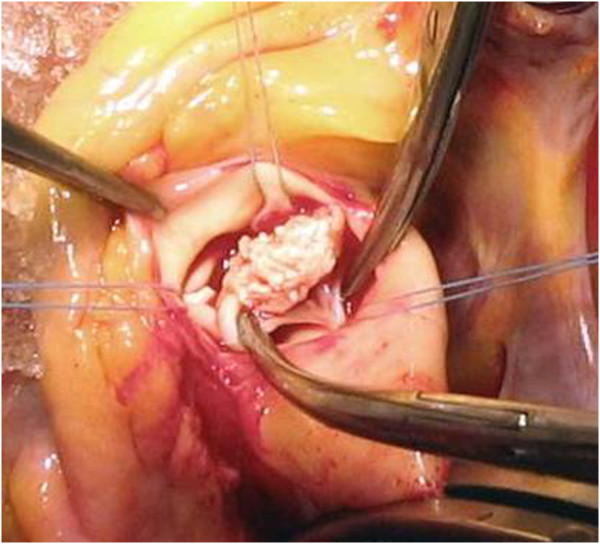
00:01 So, pathogenesis. The infection can occur for a variety of reasons and depends on the nature of the valve, and whether it has some previous deforming or deformation because of the, say, rheumatic valvular disease. 00:18 A way that you can seed bacteria into the bloodstream is with dental or surgical procedures. 00:23 So, even simple flossing actually causes a remarkable amount of bacteremia. 00:29 In most cases, in most of us, we clear that bacteria very effectively in going through the liver and the spleen. 00:36 But if you have an abnormal valve and you have a dental procedure where you now have a large shower of oral flora into the bloodstream and you don't prophylax that patient with antibiotics, that dental procedure or a surgical procedure such as a colonoscopy, can give a significant burden of bacteria into the bloodstream. 00:59 You can also have just trivial breaks in the epithelial barriers. 01:03 So, again, Staph. aureus, gee, that's probably coming from a minor cutaneous lesion overall. 01:10 And then, there's another way that you can get in bacteria and that's through intravenous drug use. 01:15 And in particular, that will tend to introduce things like Staph. aureus. 01:20 In all cases, you have microorganisms that seed into the bloodstream, and it can be bacteria, it can be fungus. So, you can have bacteremia or fungemia. 01:33 Notably, just because you have bacteria or fungus in your bloodstream does not mean that you're septic. 01:38 Again, probably daily for most of us when we floss our teeth, we are transiently bacteremic, but that doesn't mean that we're septic. 01:46 On a susceptible valve and depending on the microorganism, then it can set up shop, these bacteria that are floating around in the bloodstream. 01:56 And then, you can get an endocarditis. 01:58 So, vegetations on the heart valves and valvular destruction are classic hallmarks of infective endocarditis. 02:08 Notably, they will occur also in subacute infective endocarditis as well to some extent. 02:16 So, what do I mean by vegetation? Sounds like you've got a little bit of broccoli growing there. 02:21 Not so. Here we have, we're showing the mitral valve, and we're showing the mitral valve with this accumulation of platelets and bacteria and fibrin and inflammatory cells, predominantly neutrophils. 02:32 That is a response, an appropriate response, to bacteria that have set up shop on the surface of that valve. 02:39 That vegetation can be rather large. 02:41 It can be up to a centimeter or more, or it can be little, tiny ones. 02:45 So, those vegetations are a classic hallmark. 02:48 And then, you can also have underlying valvular destruction. 02:52 What's noted there is the aortic and mitral valves are the most common sites. 02:55 Mitral winning out much more commonly than the aortic valve. 02:59 Interestingly, if we're talking about intravenous drug use, the right-sided valves are much more commonly affected. 03:06 So, the tricuspid valve is going to be a very commonly infected valve in someone who is not using good hygiene and using intravenous drugs. 03:18 So, the inflammatory infiltrate is mostly neutrophils. 03:22 There can be some monocytes within there as well. 03:25 And because of the combined activity of the bacteria or fungus and the neutrophils elaborating proteases, reactive oxygen species, and other mediators, you can get some degree of underlying damage to the valve. 03:41 And in fact, it can also track backwards into the annulus and can give you a ring abscess. 03:48 So, these are all kind of consequences of the infective endocarditis. 03:51 Another important consequence is embolization. 03:55 These vegetations are not really well assembled. 03:58 They will flake off right and left. And think about the valve. 04:01 It's flopping in the breeze 60 to 70, 80 times a minute. 04:05 So, there's going to be prone to detachment and embolization. 04:07 That embolization can be a significant manifestation, and sometimes is the first clue that a patient has endocarditis. 04:16 You can get septic infarcts because in the fragments that embolize, there are bugs, and they go to some other place in the body, and they set up an infection there. 04:24 If they get into the vessel, we can get mycotic aneurysm. 04:27 Mycotic aneurysm just means an infected vessel with destruction of the vessel wall. 04:33 Usually, either rupture or aneurysm results. 04:35 In subacute endocarditis, it tends to be more slow growing. 04:43 There tends to be less valvular destruction. There tends to be more healing. 04:47 So, we will see granulation tissue that's indicative of that healing. 04:50 We will see less in terms of the size of the vegetations. 04:55 We may see more valvular scarring as a result of the healing. 04:59 We may see some degree of calcification in many cases because we have necrotic cells and/or bacteria that are - become a little nucleus for calcification. 05:10 You can get a chronic inflammatory infiltrate as part of that granulation tissue indicative of healing. 05:15 And that overall appearance would be much more like a subacute infective endocarditis. 05:24 So, there is a Duke Criteria for making the diagnosis of infective endocarditis. 05:28 It may not be a trivial exercise to actually say someone has got that. 05:33 So, a number of important criteria, major and minor, are included to help make the diagnosis. 05:39 One is that we would like to see microorganisms in culture or on histologic examination of the valve. 05:45 I've already told you that some organisms are rather fastidious and it's hard to culture, so we may not always get them out in culture. 05:52 And then, histologic confirmation of active endocarditis, and that's where me, the cardiac pathologist, comes in handy. 05:59 So, the clinical criteria include the major criteria, which are blood culture(s) positive, echocardiographic identification of a valve-related mass or abscess, and new valvular regurgitation. 06:12 Those are the major criteria. Minor criteria include predisposing heart lesions, intravenous drug use, fever, other vascular lesions, peripheral manifestations of embolization, immunologic phenomena probably related to cytokine production, and microbiologic evidence such as in cute - elevated acute phase reactants. 06:36 So, the pathologic criteria, if we find endocarditis, that kind of confirms it. 06:43 Otherwise, we want two of the major criteria or one major and three minor criteria or five minor criteria. 06:50 And this gives you a sense if we just have clinical information to act on, it can be relatively difficult using the pure Duke Criteria to make the diagnosis of endocarditis. 07:02 Okay, so complications of can, in most cases, be eliminated if we make a timely diagnosis and effective treatment. 07:10 Peripheral manifestations. 07:12 So the septic emboli will cause some characteristic classic lesions and you should be looking for these in patients you suspect of endocarditis in their periphery. 07:22 They can be somewhat subtle. 07:23 So, Janeway lesions are erythematous or hemorrhagic lesions due to septic emboli in various parts of the skin, typically on the palms or soles. 07:32 Osler nodes are subcutaneous nodules due to bacterial immune complexes and bacterial vegetations that are setting down within the joints or in subcutaneous tissues. 07:47 You can have splinter hemorrhages. 07:51 So, you can have septic emboli typically at the base of the nail bed, in the lunula of a nail bed, and those splinter hemorrhages are indicative or can be indicative of a septic emboli from the endocarditis vegetations. 08:07 And finally, looking in the eye grounds, you can see Roth spots. 08:11 These are flame-shaped retinal hemorrhages that again, are due to septic emboli in the eye. 08:18 You can also have non-cardiovascular complications. 08:21 So, immune complex deposition due to an ongoing bacterial infection with antibodies elaborated in bacteria can lead to the deposition of antigen antibody complexes within the glomeruli. 08:37 So, you can get a glomerulonephritis, a nodular glomerulonephritis. 08:43 And so, sometimes, the only or the initial manifestation is some degree of proteinuria and renal failure.
About the Lecture
The lecture Pathogenesis, Diagnostics and Clinical Manifestations – Infective Endocarditis by Richard Mitchell, MD, PhD is from the course Valvular and Hypertensive Heart Disease.
Included Quiz Questions
Which of the following is the LEAST likely cause of infective endocarditis (IE)?
- Intranasal drug abuse
- Dental/surgical procedure
- Epithelial barrier damage
- Intravenous drug abuse
- Active infection
Which valve or valves are most commonly involved in IE due to IV drug abuse?
- Right-sided valves (tricuspid, pulmonic)
- Left-sided valves (mitral, aortic)
- Pulmonic valve only
- Aortic valve only
- All valves, equally
Which of the following features is more commonly seen in subacute infectious endocarditis (vs. acute infectious endocarditis)?
- Increased granulation tissue
- Neutrophil-predominant infiltrate
- Large vegetations
- Ring abscesses
- Mycotic aneurysms
Which of the following is considered a major clinical criterion for IE by the Duke criteria?
- New valvular regurgitation
- IV drug use
- Preexisting valve damage
- Fever
- Evidence of a septic infarct
Which of the following situations is NOT sufficient for diagnosis of IE?
- 1 major + 2 minor modified Duke criteria
- Pathologic valve vegetation
- 2 major modified Duke criteria
- 1 major + 3 minor modified Duke criteria
- 5 minor modified Duke criteria
Which of the following is NOT a peripheral manifestation of infective endocarditis?
- Papilledema
- Roth spot
- Janeway lesion
- Osler lesion
- Splinter hemorrhage
What might you suspect as the cause of hematuria and proteinuria in a patient with a history of IV drug use and a new heart murmur?
- Glomerulonephritis due to IE
- Focal segmental glomerulosclerosis
- Renal infarction due to left atrial thrombi
- Lupus glomerulonephritis
- Renal artery stenosis
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |