Playlist
Show Playlist
Hide Playlist
Paget's Disease of Bone
-
Slides PagetsDisease EndocrinePathology.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
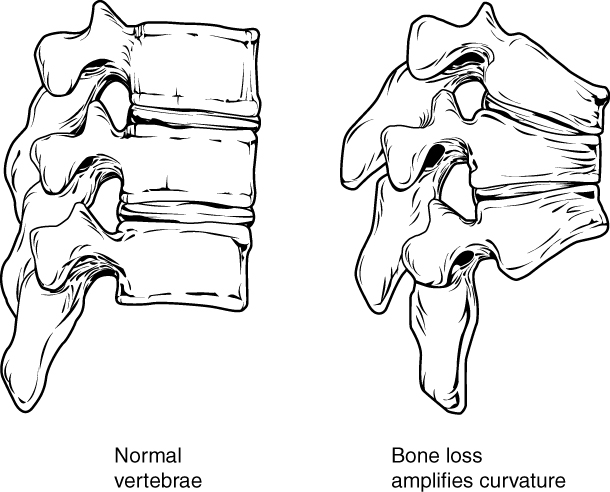
00:00 Paget's disease of bone is our topic. Prevalence of the bone disease, United Kingdom, Australia, South Africa, US and with Paget's disease of the bone fundamentally this picture pretty much tells you the story of Paget's disease, the story. The story began with healthy osteoclasts and as the day wore on and as the weeks wore on, years wore on, osteoclasts, mister osteoclasts kept getting tired and tired, tired until he'd pretty much die. Huh, so osteoclasts initially there might be too much chaotic osteoclastic activity and functioning, therefore initially you'd expect there to be increased bone resorption if you take a look at the x-ray here and on your left you'll notice that the bone appears quite lucent. That's because of increased bone resorption. Keep that in mind. So, therefore, the patient initially might have hypercalcemia. The story of osteoclastic activity continues and he starts or she starts, whatever, the cells start dying. It starts burning out. So, if osteoclastic activity starts dying out, then please understand that there's going to be increased bone activity and with that increased bone activity you are then going to have thickening of the bone as seen in the x-ray in the picture. So, therefore the picture on the right shows you increased thickened white, opaque bone representing osteosclerosis. Now what I haven't shown you here is that there is a stage in between whereas I've told you there was declining functioning of the osteoclasts. So initially there was osteolytic lesion, then there'd be as the osteoclasts are burning out a mosaic pattern. Ultimately, when you have thickening of the bone, it's called osteosclerosis to the point where you might then cause compression of certain cranial nerves for example the vestibulocochlear and with such nerves being compressed you might have problems with hearing and maybe even ringing in the ears. Etiology to this day really unclear. 02:24 There're a few theories out there and usually the patient that comes in to you or when you read about this patient, you'll hear that the patient is expressing that his or her hat size might be increasing. The pattern of bone involvement may involve one or many bones asymmetrically. Common sites include the pelvis; move a little bit higher, lumbar; even higher, skull; and then in the pelvis because you're thinking about the femur; the major common sites. 02:59 Most patients are asymptomatic where the 90%. Others have bone pain, skeletal deformity. 03:06 This was what I was talking to you about earlier, particularly the frontal and the occiput, so the front and the back, either extremes of the skull especially during the osteosclerotic phase, there might be enlargement of the skull but then that means to you that the patient is expressing that his hat size is increasing. There might be bowed lower extremity, increased fracture risk. The more bone that you have doesn't necessarily mean that what, it would be stronger. Remember you have to have remodeling, the balance between osteoclasts and osteoblasts. That balance in Paget's disease has been forever lost, so therefore femur, tibia, radius extremely susceptible to pathologic fracture. Impingement syndrome, what does that mean? The last phase of Paget's in which its osteosclerosis may then cause, as I was explaining earlier, compression of your cranial nerves. So, therefore the vestibulocochlear might be affected in your ear, hearing loss, and perhaps even vertigo. The uncommon manifestation, something that you want to keep in mind. So, let me give you some differentials or better yet why don't you give me some differentials in which the bone is becoming thicker. What's it called when you hear about marble bone disease that we talk about in ortho? That's osteopetrosis. What if you had a patient that was older and you find an adenoma in the anterior pituitary and the patient is presenting as large hands, large tongue, hat size is increasing? You find on laboratory studies that IGF1 is elevated. That's acromegaly. 04:53 Acromegaly, osteopetrosis, Paget's disease, you can then expect there to be increased thickening of the bone, but each one would be a little bit different. How can you distinguish Paget's disease from, let's say, osteopetrosis? It's easy with the acromegaly, right? An acromegaly whether that I give you for laboratory tests, increased IGF1, hyperglycemia, right, completely different presentation. Here however, with Paget's disease of the bone, we have high output, congestive high output heart failure from vascular shunts, in other words this is AV malformations that you might find with Paget's disease of the bone. Small percentage of your patient's Paget's disease of bone may result in and develop osteosarcoma and immobilization results in hypercalcemia especially in Paget's disease of the bone patients. 05:48 Paget's hip, if you take a look at the right side of this patient, then you'll notice that it's actually quite normal. The left aspect with all these arrows, these arrowheads that you're seeing, the left side of this patient's hip, you find there to be increased thickening. Thickened cortex, prominent trabeculae and could have lytic features. Remember, just because you've thickened bone doesn't mean that's stronger bone. In fact, it's increased prone or there is increased tendency of fracture to take place. It may cause substantial pain, deformity and disabilities especially in the elderly. It does not spread to other bones after those that are affected. So, do not think about adjacent bones being affected but the major bones that are affected, the pelvis, the femur, the spine, lumbar spine, and maybe perhaps the skull; in the skull, the frontal and the occiput. Let's take a look at the clinical presentation of Paget's disease of the bone, in other words von Recklinghausen disease of the bone. Take a look at that skull lit up and opaque. So would you call that an osteolytic type of appearance? Would you call that a mosaic or do you think it would be more of an osteoblastic type of appearance? Osteoblastic, correct? Because the osteoclasts have died and at this point you're in the state of sclerosis, hence extreme, extreme opacity. So in the Paget's skull, oftentimes the patient is going to present with "doc, my hat size is increasing because my head is getting bigger not due to ego but due to Paget's disease of the bone," enlargement of the skull associated with cotton wool appearance, and the osteoporosis circumscripta refers to the fact that, well, you could have regions of the bone that may be a little bit osteolytic. 07:56 If you take a look at the frontal region of the skull here, you'll notice that it is a little lucent. So what osteoporosis circumscripta refers to is the osteolytic changes you expect in the bone early on in Paget's disease. Evaluation, lab studies, isolated ____. The alk phos here is going to be incredibly elevated. That is one of the hallmark findings of Paget's disease of the bone. You'll never expect such an increase with acromegaly and with osteopetrosis once again I've given you enough clues here that without a doubt you know that your patient has Paget's disease of bone such as your AV malformation that suggest the tendency of developing osteosarcoma and the fact that the alk phos or alkaline phosphatase is elevated. Look at this, greater than 500 units per liter. The plain film can reveal the 3 phases of the disease. Early on it looks like osteoporosis. Keep that as a differential whenever you deal with bone disease especially with Paget's disease and osteoporosis. Osteoporosis completely different, different presentation, may be a female postmenopausal. Later on you get mixing. Who's dying in the meantime? In other words which osteo cell is burning out? The osteoclasts. Initially there was too much activity. Next as it starts declining, there might be a mix between osteoclasts, osteoblasts and you call that a mosaic pattern and finally 3rd phase will be your sclerosis with cortical thickening that I've talked about earlier. The bone scan most sensitive test can reveal areas of increased uptake and migratory lesions should call diagnosis of Paget's in to question, evaluate for alternative such as metastasis to the bone. Paget's disease of the bone management, symptomatic patient involving the axial skeleton weightbearing bones analgesics for the pain. Remember the Paget's disease of bone can be treated, not cured, managed may be perhaps with bisphosphonates. Bisphosphonate therapy, 1st line of severe disease. Oral agent, these include your risedronate and alendronate. Remember that alendronate could also be used for osteoporosis. The IV agents include pamidronate and zoledronate. Oral agents such as alendronate are important and we have IV agents such as pamidronate that is important. 10:35 Remember once again that with Paget's disease of the bone the major significant increase would be alk phos, 500 is the magic number.
About the Lecture
The lecture Paget's Disease of Bone by Carlo Raj, MD is from the course Bone Disease.
Included Quiz Questions
What is the pathogenesis of Paget's disease of bone?
- Dysfunctional osteoclast activity
- Excessive RANKL signaling
- Osteosarcoma
- Hypercalcemia
- Disordered alkaline phosphatase secretion
What is NOT associated with Paget's disease of bone?
- Increasing height
- Enlarged frontal bone
- Bowed legs
- Pathologic fracture
- Cranial nerve impingement
Which characteristic feature of Paget's disease of bone is caused by the disruption of normal bone formation in the skull?
- Cotton wool appearance
- Spread from skull to other bones
- Osteosarcoma
- Crew cut sign
- Decreasing hat size
What are the three phases of Paget's disease of bone?
- Osteolytic, mixed sclerosis and osteolytic, sclerosis
- Osteolytic, sclerosis, mixed sclerosis and osteolytic
- Osteolytic, sclerosis, osteolytic
- Sclerosis, mixed sclerosis and osteolytic, osteolytic
- Sclerosis, osteolytic, sclerosis
What is a hallmark lab finding in Paget's disease of bone?
- Isolated alkaline phosphatase elevation
- Increased GH accompanied by elevated alkaline phosphatase
- Hypercalcemia and hypophosphatemia
- Decreased PTH, increased alkaline phosphatase
- Hypocalcemia and decreased alkaline phosphatase
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |