Playlist
Show Playlist
Hide Playlist
Labor Stage 2: Operative Delivery
-
Slides OperativeDelivery Obstetrics.pdf
-
Download Lecture Overview
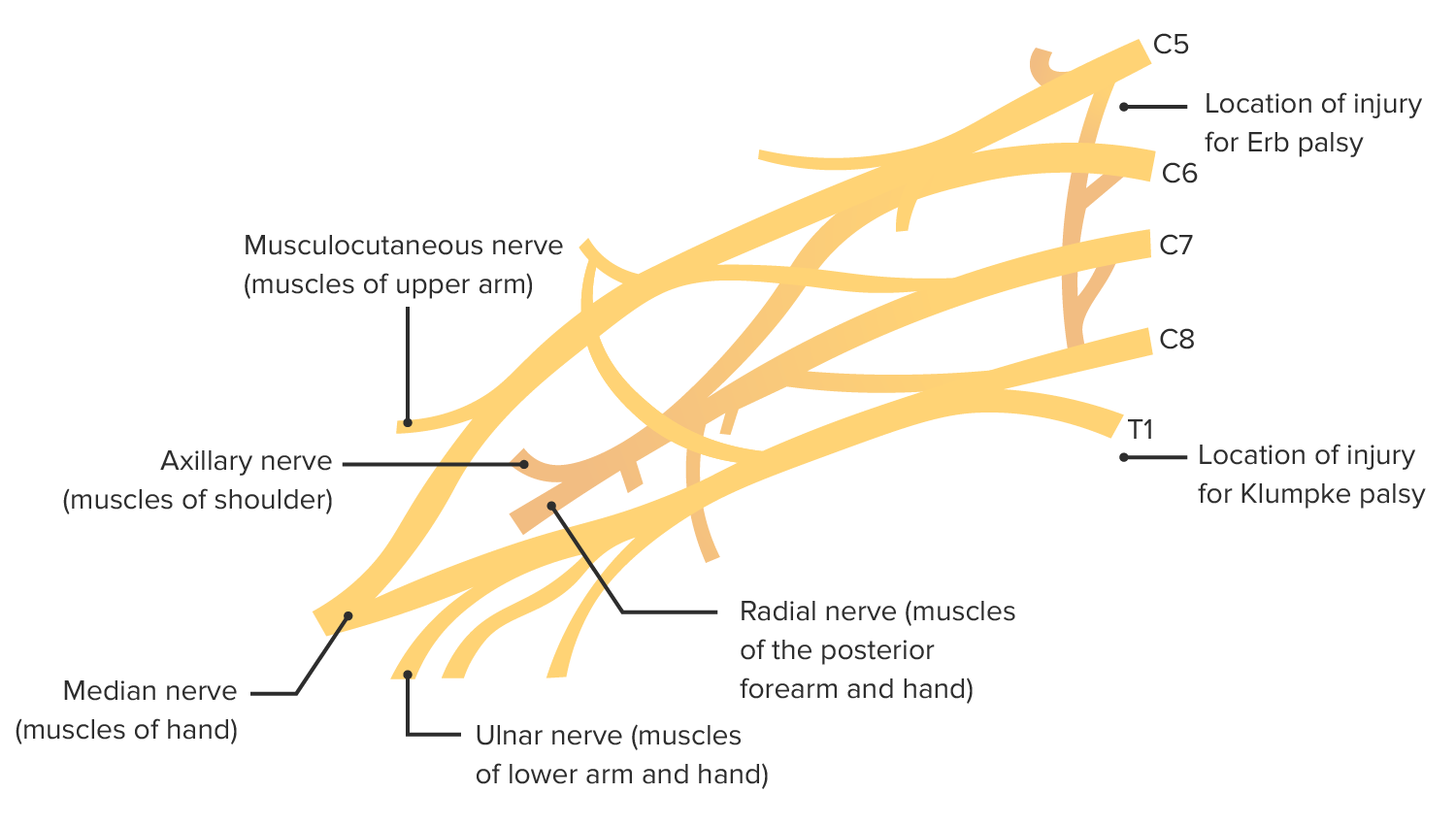
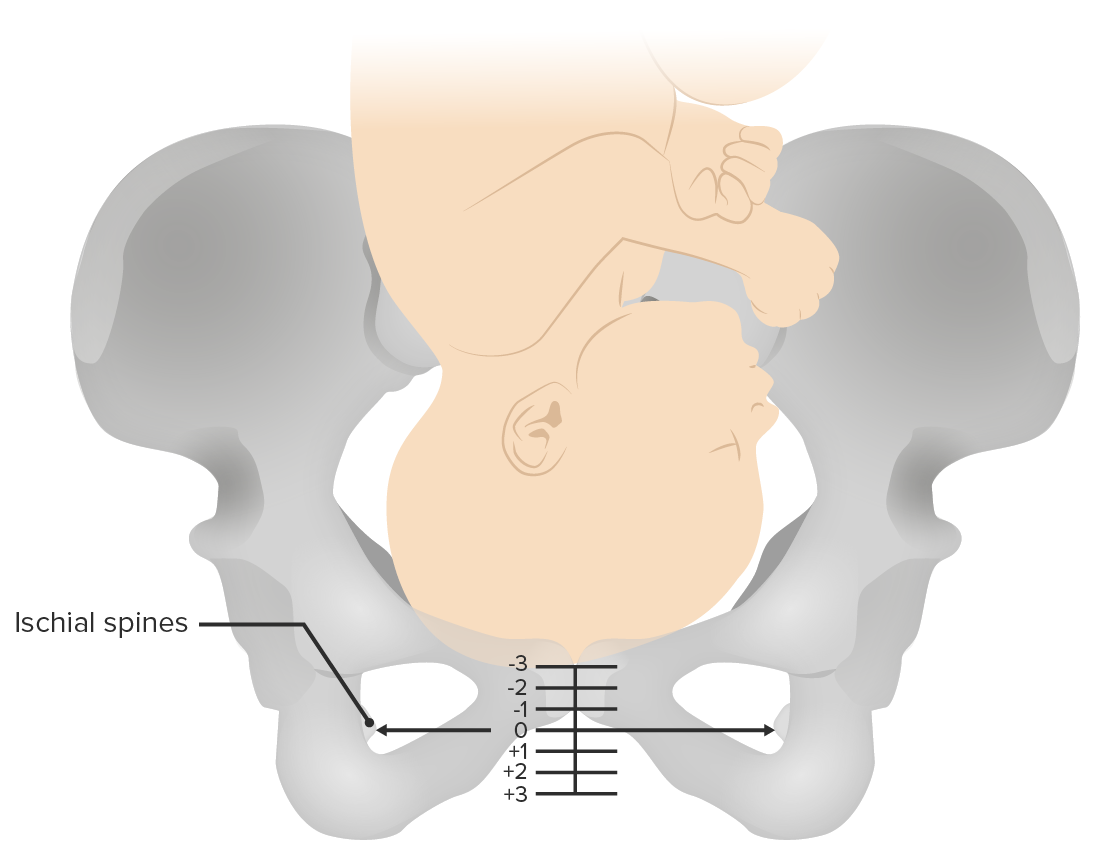
00:01 Now let's discuss Operative Delivery. 00:03 We'll start with the case presentation. 00:07 A 25 year old gravida 1 para 0 female at 38 weeks gestation and 2 days presents to labor and delivery in active labor. 00:16 She is not at stage 2 of labor. 00:19 She has an epidural in place and has been pushing for 3 and a half hours. 00:23 How would you manage her delivery at this point? Let's go through the lecture to find the answer. 00:29 So operative deliveries have 3 types that we can do operatively. 00:34 A vacuum assisted vaginal delivery. 00:37 Forcep delivery and cesarean section. 00:40 Let's take the time to talk about each of these in a bit of detail. 00:45 So the indications for any operative vaginal delivery, fetal tolerance of labor. 00:49 So we're talking about a category 3 tracing. 00:52 Arrest of the 2nd stage of labor. 00:54 And if you remember the 2nd stage of labor is when mom is pushing the baby out. 00:58 And if we had no descent over 2 hours then we now have an arrest for second stage. 01:04 And then shortening of second stage of labor. 01:06 So there's some maternal conditions where we do not want mom to exert. 01:10 The force that it takes to push such as cardiac anomalies, intercranial issues. 01:15 In those cases we will perform an operative vaginal delivery so that mom doesn't have to exert that force. 01:23 Now, there is a criteria to perform the operative delivery as well as those indications. 01:28 First is knowledge of the fetal position. 01:30 And when we speak of fetal position, we're talking about the fetal occiput in relationship to the maternal spine. 01:37 So you can see from our examples here. 01:40 Occipit anterior is what we most commonly see and that's what we have here at the top. 01:44 But you can also have occiput rotate in different positions. 01:48 You have to know that position of the head to know where to apply the vacuum or the forceps when you're performing an operative vaginal delivery. 01:57 Now the patient must be at least +2 station. 02:00 If you remember from our previous lecture, the station refers to the leading edge at the level of the ischial spine or in relationship to the ischial spine. 02:09 So we want that fetal head to be at +2 station or at least 2 centimeters below the ischial spine. 02:17 Now the cervix must also be fully dilated so 10 centimeters. 02:21 And the patient has to have adequate anesthesia. 02:26 Now what are the indications for cesarean section. 02:28 They are a little bit different than operative vaginal delivery. 02:32 Fetal intolerance of labor. 02:33 So again our Category 3 tracing. 02:36 Arrest of dilation or descent in labor. 02:38 So the cervix when it's stop dilating or if the baby stops coming down through the pelvis. 02:43 Malpresentation such a breech presentation or a mentum posterior presentation. 02:49 Placental abnormalities such as placenta percreta, increta. 02:55 Or if we have a placenta previa or the patient has previous uterine surgery. 03:01 Now this would be for example for our patients who have had a cesarean section and decline at trial of labor at the cesarean. 03:07 Or if they had 2 or more C-sections. 03:10 In those situations a vaginal delivery is contraindicated. 03:16 So, let's talk about those complications of our operative vaginal deliveries. 03:21 First with the vacuum assisted delivery. 03:23 You can have fetal scalp lacerations, Cephalohematoma. 03:27 As you can see here in this picture where we have the swelling or above the head. 03:31 And we can also have intracranial hemorrhage. 03:34 Now there is some debate specially with intracranial hemorrhage as to how much of this is caused by the operative delivery and how much of it happens intrapartum. 03:43 With forceps delivery there are also complications. 03:46 Facial laceration, injury to the facial nerve, skull fracture. 03:52 And you can also have intracranial hemorrhage. 03:57 So back to our patient. 03:59 This 25 year old gravida 1 para 0 female at 38 weeks and 2 days that presented to labor and delivery in active labor. 04:06 She is now in stage 2 with an epidural in place and she has been pushing for 3 and a half hours. 04:11 We know from our normal stages of labor and our normal parameters that as a G1, having epidural in place, she should have completed stage 2 in 3 hours. 04:21 So she's beyond that time. 04:23 Now within this, if this is a situation where the head is at + 2 station, we can consider doing an operative delivery. 04:30 That would either be operative vacuum delivery or an operative forcep delivery. 04:35 Whether you choose to do a vacuum or choose to do a forcep, is really left up to the clinician and the clinician's experience. 04:42 If that head is at less than +2 station, however, or if it's malpositioned, we would need to perform a cesarean delivery.
About the Lecture
The lecture Labor Stage 2: Operative Delivery by Veronica Gillispie, MD, MAS, FACOG is from the course Intrapartum Care. It contains the following chapters:
- Operative Delivery
- Complications of Vacuum of Operative Deliveries
Included Quiz Questions
Which of the following is an indication for operative (vacuum or forceps assisted) vaginal delivery?
- Arrest of the second stage of labor with the fetal head at least 2 cm past the ischial spines
- Arrest of the first stage of labor due to fetal intolerance of labor
- Arrest of the second stage of labor with fetal head at least at the level of the ischial spines
- Arrest of the second stage of labor due to fetal malpresentation
- Arrest of the first stage of labor due to uteroplacental insufficiency
Which of the following is a complication of vacuum-assisted vaginal delivery?
- Cephalohematoma
- Facial laceration
- Skull fracture
- Facial nerve injury
- Fetal clavicular fracture
A 21-year-old G1P0 presented to the labor ward in active labor and progressed to complete dilation and stage 2 of labor without complication. She has an epidural in place. After 3 hours of pushing, her last cervical exam demonstrated occiput anterior fetal position at 2+ station, which is unchanged from her exam 6 hours prior. She is tiring out and does not know if she can push anymore. Fetal heart tracing is Category 2 with early decelerations with contractions and several irregularly spaced variable decelerations. What should be the next step in management?
- She is in arrest of labor and operative vaginal delivery should be considered
- She should be encouraged to continue to push for spontaneous vaginal delivery since the fetus is tolerating labor
- She is in arrest of labor and cesarean section should be the next step
- She is in protracted labor and cesarean section should be the next step
- Although she is progressing well in labor, she should have an operational vaginal delivery due to fetal intolerance
Which of the following is NOT an indication for a vacuum-assisted vaginal delivery?
- Fetal macrosomia
- Fetal intolerance of labor
- Arrest of the 2ⁿᵈ stage of labor
- Need to shorten or decrease maternal exertion due to pre-existing conditions such as heart failure or intracranial berry aneurysms
- Category 3 fetal heart tracing
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |