Playlist
Show Playlist
Hide Playlist
Neuroinflammatory Disorders: Classification
-
Slides Multiple Sclerosis Inflammatory Disorders of the CNS .pdf
-
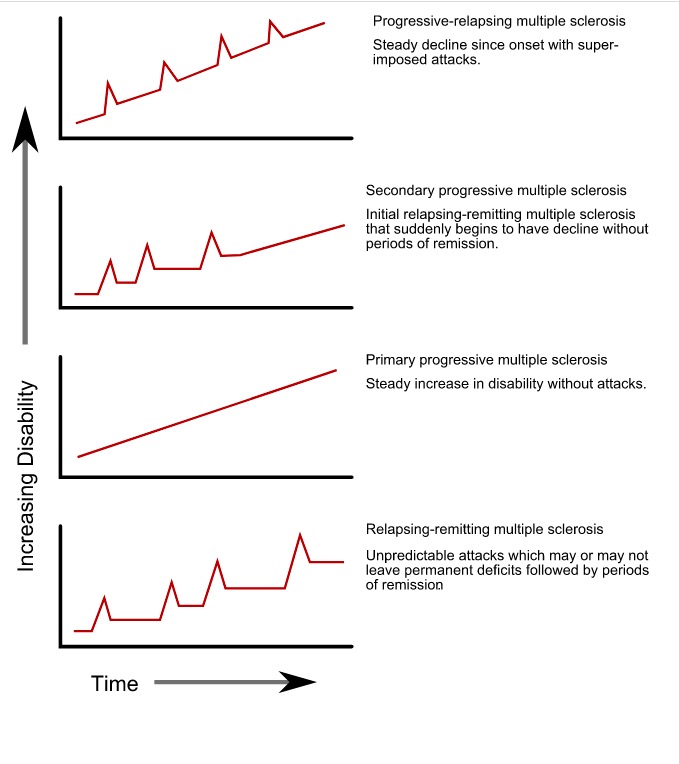
Download Lecture Overview
00:01 So how do we think about neuroinflammatory disorders? What is the classification? I like to think about classifying them in three ways. 00:09 The first is whether they're primary or secondary. 00:14 The second is by the type of the dominant immune population that's involved. 00:18 And we'll talk a little bit more about what that means. 00:20 And then last, I differentiate the isolated single events from recurrent or multiple events over time. 00:26 And this helps us to understand the types of neuroinflammatory disorders we can see, and the ones that we're going to diagnose in patients and on test questions. 00:37 First, let's start with step one. 00:38 Let's understand the difference between a primary CNS neuroinflammatory disorder and a secondary CNS neuroinflammatory disorder. 00:48 Primary neuroinflammatory disorders are ones that were the autoimmune attack is only in the CNS. 00:54 There's not a systemic immune disorder, there's not systemic autoimmunity, this is autoimmunity to the brain and to the brain only. 01:02 Examples of this include multiple sclerosis, neuromyelitis optica, and MOG antibody disorder, which we'll talk a little bit more about. 01:10 Here, we need to evaluate inflammation within the Central Nervous System. 01:15 We're looking for activation of the immune response in the CNS. 01:18 We can do a lumbar puncture to look for elevated protein and possibly mildly elevated cells. 01:24 We're looking for that immune infiltration into the CNS, or neuroimaging showing an immune attack on the brain or spinal cord, which is evidenced by increased T2, signal, swelling in the central nervous system and often with the presence of enhancement. 01:39 That enhancement is indicating breakdown of the blood-brain barrier, which is how the immune system is infiltrating into the central nervous system. 01:48 There's often not evidence of systemic inflammation. 01:51 We don't see elevation on ESR or CRP, or ANA's, or rheumatoid factors, or other evidence of an underlying autoimmune condition. 01:59 The primary process is in the brain or CNS. 02:04 That differs from secondary CNS neuroinflammatory disorders, where the immune attack occurs in the systemic system, and then it flows into the brain or central nervous system as a result of the underlying systemic autoimmunity. 02:18 Examples of this include systemic lupus erythematosus, Sjogren's syndrome, rheumatoid arthritis, and others. 02:26 And here the patient has an underlying systemic autoimmune condition that can involve the brain. 02:32 Our evaluation here involves a twofold evaluation, both looking for evidence of CNS immune attack, as well as the underlying systemic activation of the immune system. 02:43 And we can do that by investigating the CNS with a lumbar puncture. 02:46 We're looking for increase in CSF protein, and potentially mild elevation in cell counter pleocytosis. 02:53 The neuroimaging showing an immune attack on the brain or spinal cord. 02:58 In addition, these patients require systemic evaluation for an underlying autoimmune condition. 03:03 My typical screen includes an ESR, CRP, ANA, and rheumatoid factor, but we may need to dig deeper based on the history and the examination of the patient, if we're concerned about one of these conditions. 03:15 We may look for double stranded DNA testing in patients who may have systemic lupus or sjogrens antibody, SSA, SSB, or RO or LA antibodies in patients with sjogrens syndrome, or rheumatoid factor and patients with rheumatoid arthritis, digging for that underlying evidence of a systemic autoimmune condition. 03:39 Step two in evaluating these patients is to determine whether this is a monophasic illness or recurrent illnesses. 03:45 because there were recurrent attacks, immune attacks that could occur in the nervous system, or is this a single one time event. 03:52 So, monophasic illnesses and recurrent illnesses. 03:57 The classic monophasic course you're seeing here in this schematic graph. 04:02 And we see evolution over time and patients with a monophasic illness have a single attack. 04:06 They begin normal. 04:08 There's onset of disability, which typically occurs sub acutely. 04:12 So over the course of a couple of weeks, patients will develop weakness in the arm or leg, they'll develop a paraparesis. they'll develop vision loss, and that sub acute onset is common in patients who have inflammatory disorders. 04:24 This peaks often over the course of a couple of weeks and then gradually improves. 04:30 With patients typically returning to normal, as you see in this graph with no long term disability. 04:35 Now patients can be left with long term disability as a result of this monophasic illness. 04:41 And certain conditions will result in a monophasic course. 04:46 And that's different from the recurrent course. 04:48 And here we see a good example of the depiction of what a recurrent autoimmune condition will look like. 04:54 These patients have periods of relapse where there's a new disability and remission, which often returns to normal. 05:01 Here we have sub-acute onset of symptoms in each one of these relapses. 05:05 So patients develop new symptoms over the course of days, to weeks. 05:09 And again, this may be hemi body symptoms or paraparesis, or new vision changes, as a result of wherever the lesion is occurring. 05:16 The immune attack is occurring in the brain. 05:18 This peaks over the course of a couple of weeks, and then there's spontaneous improvement or improvement more quickly with treatment. 05:25 Patients often returned to normal without disability, but we can see persistent disability after each one of these episodes. 05:32 And again with recurrent conditions patients are at risk for relapses for new episodes or recurrence of symptoms. 05:40 with each one of these episodes. 05:43 And this relapsing remitting course is highly suggestive of a CNS autoimmune condition. 05:49 We think about autoimmune conditions, paraneoplastic conditions, sometimes infections can have this relapsing remitting course and occasionally toxic exposures. 05:59 Those four pathophysiologic processes are the ones we should consider with this type of a course.
About the Lecture
The lecture Neuroinflammatory Disorders: Classification by Roy Strowd, MD is from the course Multiple Sclerosis (MS) and Inflammatory Disorders of the CNS.
Included Quiz Questions
Classifications of neuroinflammatory disorders include which types? (Select all that apply.)
- Primary versus secondary
- Disorders classified by the dominant immune population
- Isolated versus recurrent
- Disorders classified by how many joints are affected
A neuroinflammatory disorder with an elevated ESR and CRP is most likely to be classified as which type of disorder?
- Secondary neuroinflammatory disorder
- Primary neuroinflammatory disorder
- Recurrent neuroinflammatory disorder
- Remitting neuroinflammatory disorder
An individual presents to you with a six-episode history of neurologic symptoms that come on over days to weeks, and typically resolve after a few weeks. How might the time course of this disorder be classified?
- Recurrent
- Monophasic
- Continuous
- Singular
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |