Playlist
Show Playlist
Hide Playlist
Mycobacterium Tuberculosis
-
01-07 Mycobacteria.pdf
-
Download Lecture Overview
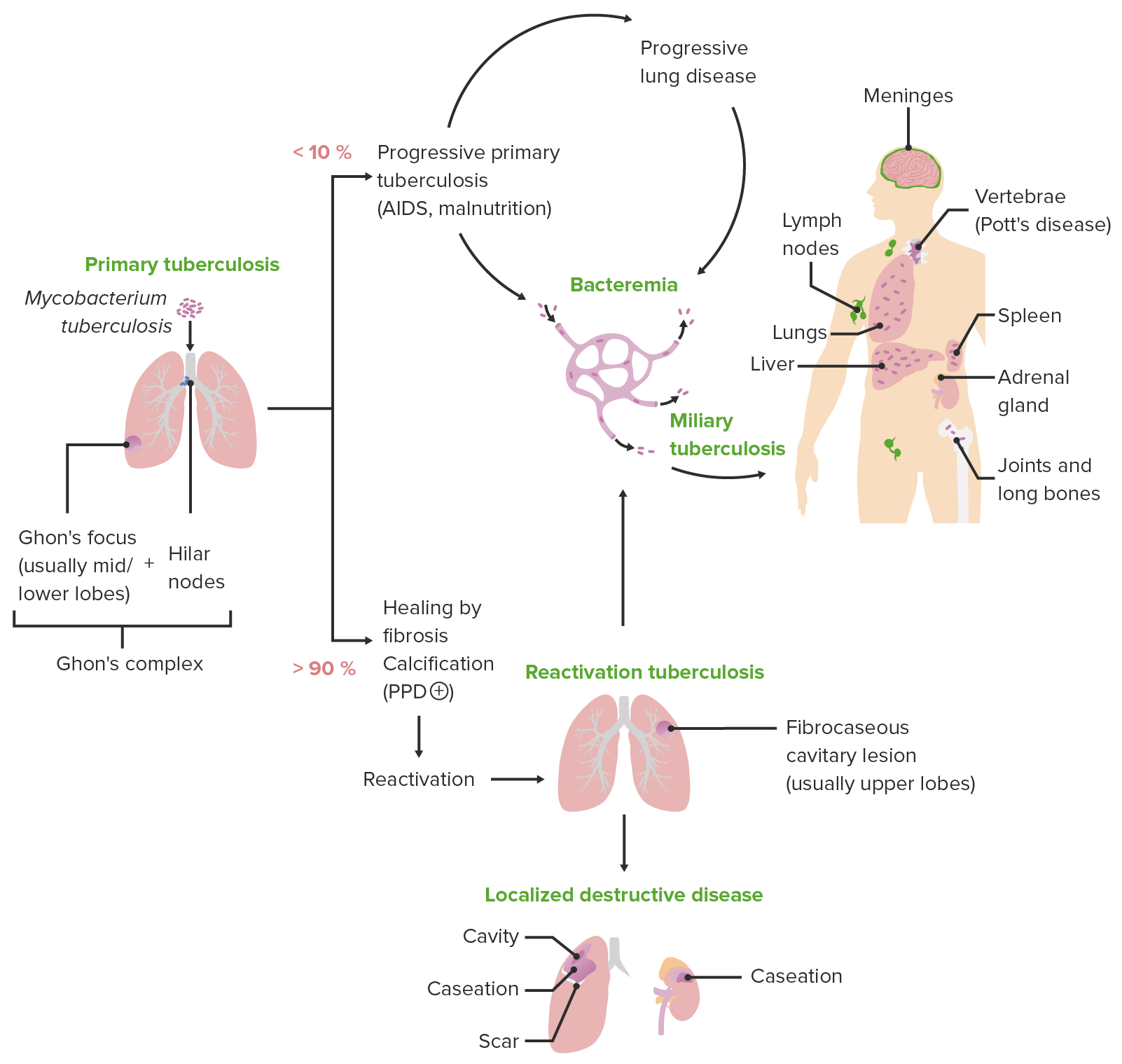
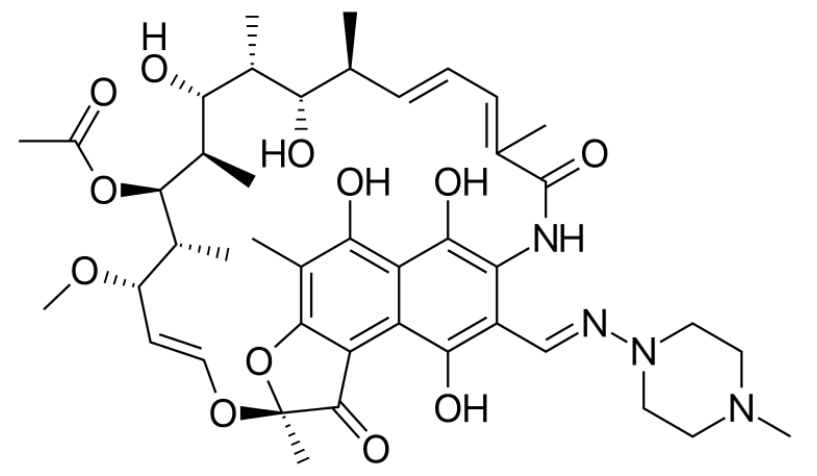
00:01 Let's look first at Mycobacterium tuberculosis as the most recognizable cause of disease. Humans are the only lucky natural reservoir for disease for this organism. 00:13 Typically, the organism is transmitted through respiratory droplets and not your typical small droplets, such as you would get with sneezing but large, heavy droplets. In fact, the contagious area related to a respiratory droplet from somebody with tuberculosis is within three to at most six feet, unless they have cavitary disease, which we'll examine shortly, in which case their droplets are large and are coughed or expressed with high velocity. 00:43 Who then is at risk for tuberculosis? Unfortunately, anybody, especially if they live in an endemic area. 00:50 However, there are classic risks and those are the elderly or the young, i.e. those with immature or waning immunity and patients who are immunocompromised. For whatever reason. 01:02 The x ray that you see on this slide shows a Cavitary tuberculosis lesion. 01:07 A patient with a lesion such as that outlined by the arrows would be highly contagious if they're coughing. 01:14 And again, those with cavitary lung disease, regardless of the age, are highly contagious but still within a somewhat limited spatial distance. 01:24 So let's look a bit more closely at the pathogenesis of Mycobacterium tuberculosis. Or as I might abbreviate in this lecture MTB. 01:34 First is the inhalation aspect. 01:36 You might be a happy, innocent casual bystander standing next to somebody with cavitary TB. 01:43 They might cough, you might inhale. 01:45 And in go the acid fast bacilli the MTB. 01:50 Next, as you are lowering the organism into your airways the bacteria. The MTB will be phagocytosed typically by alveolar macrophages. 02:01 They are part of the innate immunity present in your respiratory tissue, which are very good at at eating or phagocytosing for material such as in this case, our MTB bacteria as that alveolar macrophage ingests or phagocytosis the MTB, it has on its own a triggering of pro-inflammatory cytokines such as you see listed on the slide, especially the Interleukins one, 12 and 18, which will stimulate by cytokine pathways a local inflammatory reaction. 02:38 Next will be induction of interferon gamma VI triggered T lymphocytes, especially those that are CD8 positive and CD4 positive. And you can see that mechanism on the slide as well. 02:51 One gets an interaction between the alveolar macrophage, which has been stimulated by ingestion of the MTB, and then further release of pro-inflammatory cytokines, including the interferon gamma, which are supposed to induce bacterial killing. 03:07 In addition to that, TNF alpha tumor necrosis factor alpha is another pro-inflammatory cytokine which is precipitated in its release by the presence of MTB within the alveolar macrophage. 03:21 All of these steps occur sort of in a sequential but also simultaneous fashion, creating to the growth of a granuloma or a localized site of infection with the MTB, and the entire process is meant to control growth of the MTB, to limit it from infecting additional cells and proliferating in a typical fashion that also means to control the further growth or further proliferation of MTB, that continuous cytokine stimulation and continuous immune surveillance must occur. 03:57 That means that granuloma, which is forming, is an entire cluster of activated, actively secreting immune cells, all which are tasked to limit this further spread of MTB. 04:10 That is fantastic. 04:11 That's great. The macrophages contribute to that and they continue to be part of the activated process. 04:17 The problem occurs when the process breaks down. 04:20 And this is what's referred to as post primary tuberculosis. 04:24 The first step that we just described is the initial infection. 04:28 Most often there are no symptoms associated with it unless the patient is immunocompromised. Most often then the patient has what is called latent tuberculosis infection TB. 04:41 That's the first stage in which the organism is ingested into the lungs, walled off within the granuloma, and sits there, hopefully in a quiet fashion forever. 04:51 However, sometimes things break down and when they do, it's due to a failure in that ongoing immunosurveillance such as we see here. 05:01 When that happens, the MTB is able to proliferate, evade its macrophage ingestre, and cause further proliferative disease, and that then allows for disease to reactivate disease is the presence of actual symptom signs and clinical symptomatology associated with the infective presence of an organism within the cell. 05:25 When that happens, then damage of nearby bronchi occur, damage of alveoli occur, and one gets to the spread of MTB to other areas of the lung. 05:34 This is post primary tuberculosis. 05:38 What can happen further is in patients who have a specific immunodeficiency. And here we turn our minds to those patients with HIV Aids in which their CD4 T lymphocyte cell function is either compromised or absent. When that occurs, there is no hold, no no limit to associate with, and the and the granulomas develop even further into pulmonary disease. 06:06 If the CD4 function is absent and the macrophages are unable to proliferate and release pro-inflammatory cytokines in response, then granulomas don't even occur and one has free ranging or completely overwhelming MTB infection in the lung. 06:23 This is the state in patients with HIV Aids. 06:28 So let's look a little bit more closely then at what happens in the stages in tuberculosis infection. 06:34 And we start again with primary TB. 06:37 The initial infection occurs with the first aspiration of the MTB into the airways. And then hopefully it's walled off into the granuloma. 06:47 However, within several years of infection, if immunosurveillance decreases, up to 10% of patients may develop active disease. 06:57 When that occurs, the disease occurs in the mid and lower lobes. 07:00 There's higher oxygen tension there. 07:03 And so those organisms can grow a little bit more expediently. 07:07 What may develop then in the specific and focal setting of an infection would be something called the Ghon focus, in which the MTB is proliferated in the subpleural area, causing necrosis or a gone complex, which also involves the higher lymph nodes. 07:25 The entire process creates a focal infection which has not yet spread throughout the lung. Patients at this stage of infection may have a very nonspecific presentation. 07:36 They may appear simply flu like, so malaise, low grade fevers, they may have some night sweats, they may have a cough. 07:45 They may have weight loss. 07:46 At some point, the cough may progress to become productive of bloody sputum or hemoptysis in patients with active tuberculosis, meaning that the disease is now evaded its immune mediated controls and is progressing. Those patients will develop further cough, further malaise, further night sweats. Everything is amplified to a power of ten or so. 08:10 And these are patients that, on plain radiography on the x rays, will show evidence of pneumonitis and hiler lymphadenopathy, progressing then into secondary tuberculosis. 08:21 This is the reinfection step. 08:23 So after the initial aspiration and with now lack of immune suppression patients will develop progressive disease going from that focal area. 08:34 Perhaps that go and focus into cavitary lesions throughout the lung fields themselves. And here, with increasing oxygen tension in the upper lobes, the disease will progress into cavitary lesions. 08:47 Miliary spread is a reference to millet seeds, which are the way that these illnesses look on x ray. 08:55 Tiny little dots of focus of disease spread throughout the lung fields. 09:01 This also can be associated with recurrence of new clinical manifestations and further hemoptysis. 09:08 Now, a patient may go between primary TB infection and the secondary TB infection for months, years or even decades, or potentially until they become older and have a waning of their immunity. 09:20 Those patients who are overtly immunocompromised, whether they are immunosuppressed due to medications or have acquired HIV infection, progressing to Aids, or have undergone treatment of cancer with chemotherapy, any compromising of the immune system can allow for extrapulmonary disease to occur. 09:41 Now this also has in parentheses miliary TB. 09:44 Because tuberculosis preferentially occupies and creates infection in only a few small foci throughout the lungs. 09:53 However, when that immune control evaporates, those small foci can then disseminate throughout the lung fields, causing that miliary or millet seed appearance, but the bacteria can also spread throughout the blood and the lymph system to go throughout the entire body. 10:10 And as you can see listed on the slide, many patients will develop disease throughout the genital urinary system, central nervous system, the kidneys, and in fact, the kidneys are the most common extrapulmonary site. 10:23 The symptoms and signs of clinical disease in this case are nonspecific, except that patients may have ongoing weight loss, they may develop skin lesions, and they may develop clinical evidence of multiple organ dysfunction. 10:38 Diagnosis. As mentioned before, the mycolic acid present in the cell wall of MTB is acid fast, and so one can perform an acid fast stain on induced sputum or on a biopsy specimen and look for the organisms such as you see here on the slide. 10:58 Isolation also can occur through culturing the organism on lowenstein-jensen culture media, but it requires 3 to 6 weeks for MTB to grow. 11:07 It's quite a slow grower, which again goes along with the onset of disease. It's a slow process. 11:15 We, however, can look for immune recognition of infection with MTB by placing a tuberculin skin test, which is known as PPD or purified protein derivative. If the patient has been exposed to or infected with MTB and developed an immunologic reaction, they will then mount a type four hypersensitivity reaction or a delayed type hypersensitivity, also known as, and create an erythematous or a red raised nodular reaction to placement of the PPD in the intradermal intradermal excuse me space. 11:54 Now, importantly, one has to read the amount of the induration to accurately describe the result of a PPD. 12:02 Unfortunately, a common clinical mistake is to simply measure the diameter of the redness surrounding the reaction. 12:10 That, however, is not the true indurated reaction by Deloitte. 12:14 Excuse me, delayed type hypersensitivity. 12:17 Instead, one should measure the thick indurated raised component, and one can do that by taking a simple ballpoint pen, and on the arm of the site is drawing a line until you reach the edge of that indurated raised spot. 12:31 Do so in all four directions, and then measure the diameter between the ends of the pen line. That's the true induration, not the full amount of the redness or the erythema. Now, there are several reasons that some may have a false positive or a false negative. 12:48 Ppd a common reason to have an exaggerated PPD reaction is if the patient had previously had a PPD placed certainly within the last 48 to 72 hours, or even in the last 2 to 4 weeks, because one would have precipitated a reaction by delayed type hypersensitivity to replace and rechallenge. 13:10 The immune system that way would create an even more exaggerated response, because those innate immune cells are already and still activated. 13:19 In fact, in hospital infection control practices, we call the whole process a two step PPD, placing an initial PPD, measuring the result, then placing a second PPD two weeks after the first, measuring the result. 13:35 Again, it's a good way to bring out a very slow or early reaction to somebody who might just have been exposed to tuberculosis infection. 13:45 A common cause of false negative results will be medications and recent infections, especially recent infections that in part suppress the immune system. Infections with some of the herpes viruses, such as Epstein-Barr virus infection or cytomegalovirus, can absolutely suppress the immune reaction. 14:04 An infection like HIV, which specifically targets CD4 cells, can absolutely cause a false negative, as can granulomatous diseases such as sarcoidosis. 14:15 And again, those who are very old or very young. 14:18 Use of steroids has an unpredictable interaction with the development of a delayed type hypersensitivity, and so a false negative could occur in a patient who recently has received either systemic or oral steroids. A classic reason for a positive PPD is receipt of the BCG vaccine, which is given in many parts of the world, and it's difficult to interpret. 14:43 Then a PPD in a patient who received such a vaccine. 14:47 Is it a true positive meaning they actually do have MTB, or is it simply a low reaction which is precipitated by having received the BCG vaccine in the past treatment? Assuming that one has now confirmed presence of MTB infection, the treatment is ripe. No, not what you probably smell like after studying for a very long time, but ripe. The four initials of the four anti-tuberculosis drugs that typically are used rifampin, isoniazid, pyrazinamide and ethambutol. 15:20 Easy to remember if you can just remember ripe. 15:23 All four drugs are started together for the first part of treatment for a tuberculosis infection, and those are used for the first two months of treatment. 15:33 Then just the rifampin and isoniazid are used together for. 15:38 For another four months total of six months treatment, but only the first two months of which have all four drugs. 15:44 The right treatment prevention well prevention in part depends on recognition, and thus all health care workers undergo annual screening by PPD looking for prior infection with or exposure to the MTB organism. 16:01 Prevention. Well prevention in part depends on recognition, and thus all health care workers undergo annual screening by PPD looking for a prior infection with or exposure to the MTB organism. 16:16 Additionally, the US Preventive Services Task Force recommends screening all patients at risk of TB infection. 16:24 This may include individuals who were born or lived in regions with a high prevalence, or individuals who have lived in certain congregate settings, such as homeless shelters or correctional facilities. 16:35 Those who are positive will likely undergo some treatment to help minimize the reaction likelihood and development of secondary tuberculosis. 16:45 Similarly, the BCG vaccine can be administered to those who are very young and living in an endemic part of the world. 16:53 And then for those who are exposed, some cases deserve prophylactic isoniazid or in if they are in high risk.
About the Lecture
The lecture Mycobacterium Tuberculosis by Sean Elliott, MD is from the course Bacteria.
Included Quiz Questions
Which of the following refers to the typical mode of transmission of Mycobacterium tuberculosis?
- Through respiratory droplets
- Through sexual contact
- By a fecal-oral route
- Through blood
- Via vectors
The release of which of the following proinflammatory cytokines primarily induces bacterial killing in response to the phagocytosis of Mycobacterium tuberculosis by alveolar macrophages?
- Interferon-gamma
- Tumor necrosis factor-alpha
- Interleukin-11
- Interleukin-6
- Interleukin-18
Which of the following terms best describes the involvement of the hilar lymph nodes during infection by Mycobacterium tuberculosis?
- Ghon complex
- Ghon focus
- Cavitary lesion
- Consolidation
- Miliary spread
Which of the following is a characteristic pulmonary finding in cases of secondary tuberculosis?
- Cavitary lesions in the upper lobes
- Consolidation in the upper lobes
- Ghon complex in the upper lobes
- Ghon focus in the upper lobes
- Consolidation in the lower lobes
Previous administration of which of the following vaccines may result in a false-positive result on a tuberculin skin test?
- BCG vaccine
- DPT vaccine
- MMR vaccine
- Hib vaccine
- HPV vaccine
Which of the following stains will best detect Mycobacterium tuberculosis in the sputum of an infected individual?
- Acid-fast stain
- Gram stain
- Auramine–rhodamine stain
- Hematoxylin and eosin stain
- Periodic acid–Schiff stain
Which of the following culture media is most commonly used to grow Mycobacterium tuberculosis?
- Löwenstein-Jensen medium
- Blood agar
- Chocolate agar
- MacConkey agar
- Baird-Parker agar
Which of the following types of hypersensitivity reactions is expected in response to injection of purified protein derivative (PPD) in an individual exposed to Mycobacterium tuberculosis?
- Type IV hypersensitivity reaction
- Type I hypersensitivity reaction
- Type II hypersensitivity reaction
- Type III hypersensitivity reaction
- Type V hypersensitivity reaction
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
It's explained in a very understandable way and slow for non native speackers