Playlist
Show Playlist
Hide Playlist
Meningitis and Encephalitis (Emergency Medicine)
-
Emergency Medicine Bord Meningitis and Encephalitis.pdf
-
Download Lecture Overview
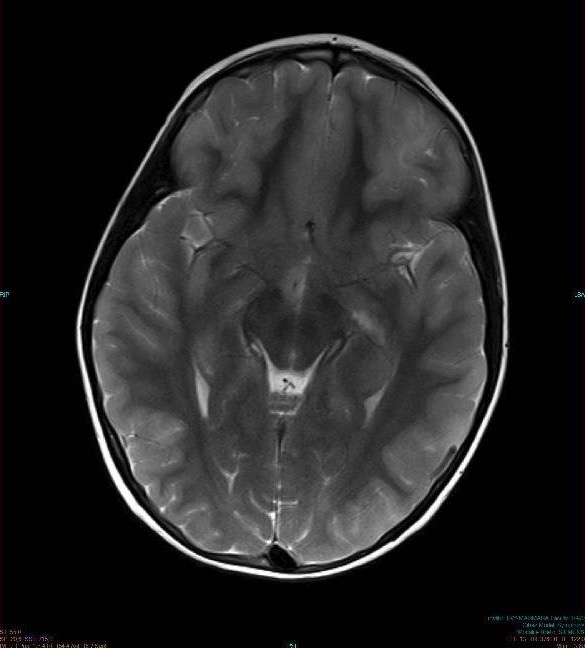
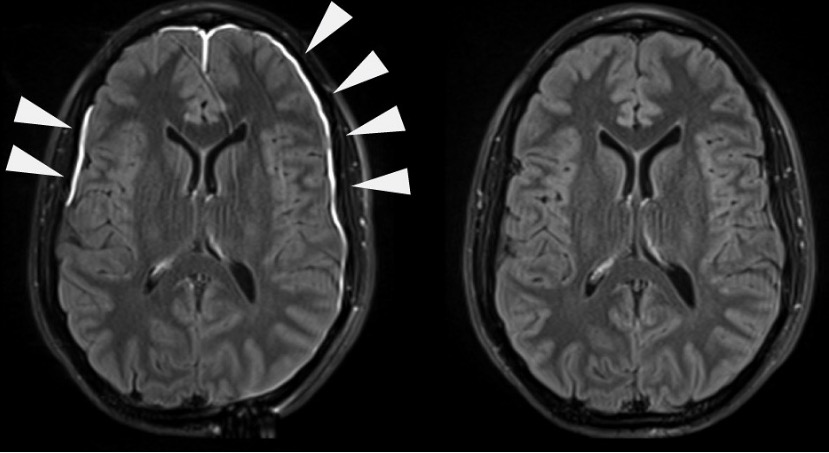
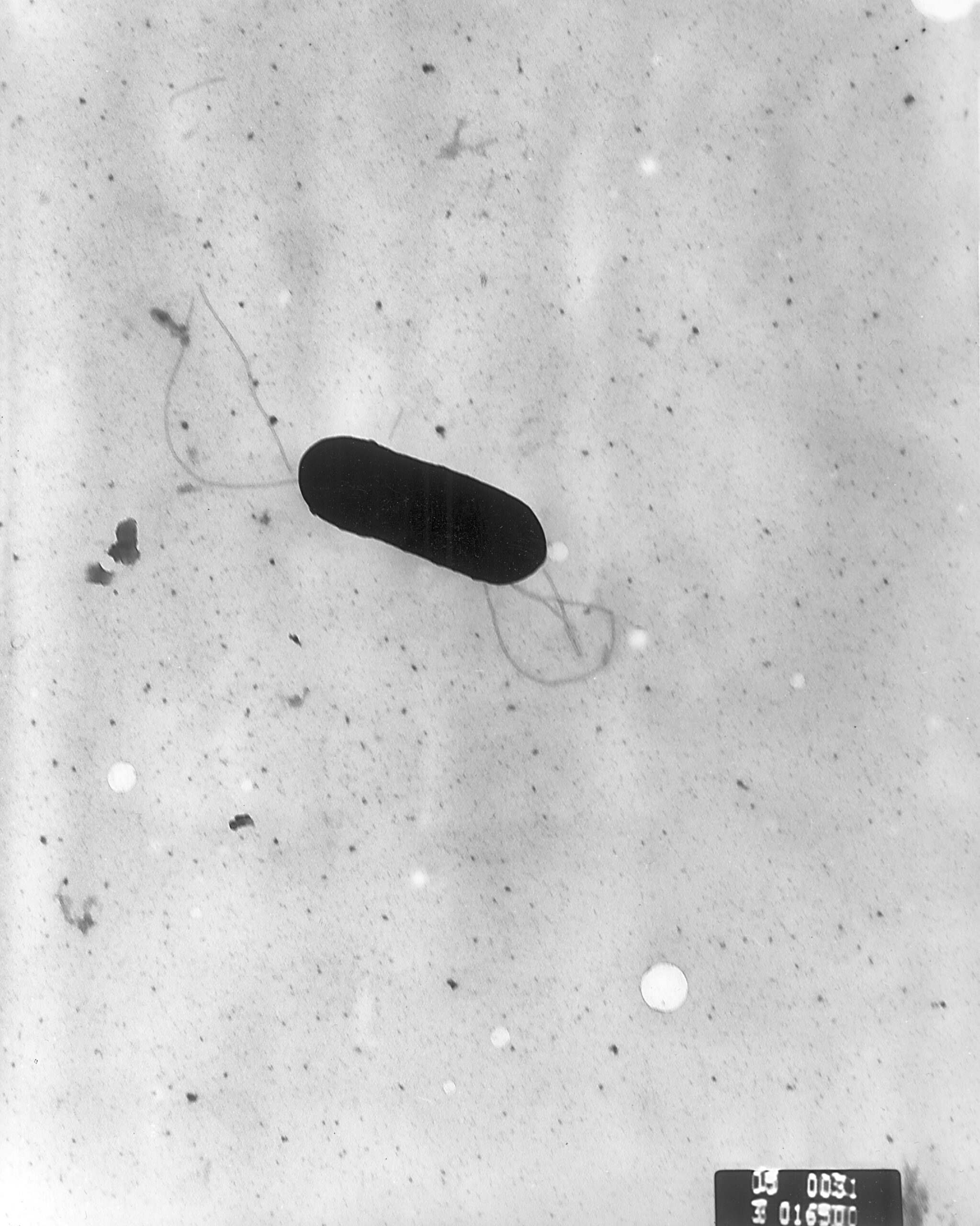
00:02 Hi. 00:02 We’re gonna be talking about meningitis and encephalitis. 00:07 Let’s get started by talking about some definitions. 00:10 So what does meningitis mean? Meningitis is essentially inflammation of the membranes surrounding the brain and spinal cord. 00:16 Here, we’re gonna be talking about primarily infectious related meningitis. 00:20 Encephalitis is a little bit different in a sense that it’s inflammation of the brain itself. 00:25 So meningitis is the inflammation of the membranes, the meninges that surround the brain and the spinal cord. And encephalitis is inflammation of the brain matter itself. 00:34 Now what causes meningitis? The most common things we’re gonna talk about here. 00:40 So bacterial meningitis is one of them. 00:42 And the most common bacteria that cause meningitis are streptococcus pneumoniae, Neisseria meningitidis, listeria monocytogenes and haemophilus influenza. 00:52 Important things about each of these, these different bacteria. 00:57 So strep pneumo is a very common cause of bacterial meningitis. 01:02 Neisseria meningitidis is a very — is less common but is unfortunately, has a very high, high mortality rate associated with it. 01:11 An interesting thing about Neisseria is that it’s related to patients living in closed quarters or the people living in closed quarters. 01:17 So historically, like dorms and military barracks are the classic patients who we worry about this in. 01:25 Now for this reason is why patients or teenagers rather, get a vaccination or it's recommended they get a vaccination against Neisseria meningitidis before they go off to college or potentially to the military to help prevent Neisseria. 01:42 Listeria monocytogenes is a cause of meningitis that’s primarily in the very young and the very old. 01:48 So in that new born, infant time period as well as in elderly people, you wanna think about listeria. 01:55 And then haemophilus influenza used to be a very common cause of meningitis but in the last number of years, the use of haemophilus vaccination has increased quite a bit. 02:08 So haemophilus has decreased its rate of causing meningitis significantly. 02:16 Tuberculous meningitis is a rare but potential cause for meningitis, that’s meningitis caused by tuberculosis. 02:24 Viral meningitis is actually a relatively common cause of meningitis. 02:31 The most common viruses that cause meningitis are enterovirus as well as HSV. 02:38 So those are the most common ones that we do see but there are a whole bunch of other viruses that can also cause viral meningitis. 02:46 Now for the most part, when we’re thinking about viral meningitis, it’s important to note that while bacterial meningitis can have a significant morbidity associated with that mortality, viral meningitis, especially those cause by enterovirus and variety of other viruses is actually relatively benign. 03:05 HSV is the one portion of viral meningitis that requires more aggressive treatment with an anti-viral medication. 03:14 And then fungal meningitis is the last big category here. 03:18 The most common fungal meningitis that occurs is cryptococcal meningitis and here you could see it on a special stain. 03:27 Viral meningitis is more common in the summer months. 03:30 And it’s more common in the summer months due to increased prevalence of the enterovirus during that time period. 03:35 So June, July, August is gonna be the time period that it's most common. 03:41 Patients who have meningitis, the classic symptoms that you think about are fever, headache and altered mental status. 03:51 Now it’s important to note that these symptoms are not all present in all people with meningitis. 03:57 So you wanna make sure you’re maintaining a high level of suspicion for this condition. 04:01 Now some people do so say that fever, headache, or altered mental status, one of those needs to be present in order to make the diagnosis of meningitis and that’s likely true, but just make sure that you’re thinking about this and considering it for patients you present. 04:16 Photophobia is another classic symptom. 04:18 What that means is that the light will bother the patient’s eyes, vomiting, chills. 04:24 Classically, we think of shaking chills. 04:26 So a patient comes in and they say they were shaking, their whole body were shaking all over, they were having chills is a classic thing, especially with especially with strep pneumo that can be a classic thing that’s also associated with pneumonia. 04:37 And then neck stiffness, we call that one of the big signs of meningismus. 04:42 So when you’re trying to talk with the patient about what kind of symptoms they are experiencing, asking them if their neck has been bothering them or causing them pain is an important piece of the history. 04:54 And like I mentioned, you wanna make sure you maintain a high suspicion for this diagnosis, especially in a patient who is immunocompromised. 05:01 Are they immunocompromised due to an underlying medical condition or they’re immunocompromised due to medication that can make them immunocompromised, especially in transplant patients or other people who have medications that make them immunocompromised. 05:16 Older patients can always be tricky and may not necessarily present with those classic symptoms. 05:21 And then patients who you're concerned with fungal meningitis can be very tricky as well. 05:26 So these patients may all present with subtle symptoms. 05:29 Fungal meningitis can actually develop over a much longer time period and patients can have much vaguer symptoms. 05:35 So making sure that you’re thinking about that and keeping it on your differential diagnosis is key. 05:41 The other important thing to keep in mind and a good clinical pearl here is that there's a higher incidence of seizures in patients who have HSV related encephalitis. 05:50 So for patients who present with seizures, and fever, and headache, definitely, you wanna be thinking about HSV. 05:57 You also wanna make sure you’re thinking about other risk factors for these conditions. 06:01 So what are the other key risk factors? So again, the young and the old. 06:06 So little babies, older adults. 06:09 Patients who have had a splenectomy. 06:11 This is something that sometimes I actually forget to ask about. 06:14 So making it you know, a common thing that you ask about in patients who have had abdominal surgery. 06:19 Now some patients believe it or not, might not actually know if they've had their spleen taken out. 06:24 So for those patients, you wanna look at their belly and see if they have a scar. 06:29 The other thing to remember about the splenectomy is that, in patients who have sickle cell, they might have a splenectomy where their spleen isn’t functioning effectively due to the fact that that organ doesn’t work effectively in patients with sickle cell after a period of time so keeping that in mind as well. 06:45 The immunosuppressed patients. 06:47 Patients who are on immunosuppressive medication or have underlying medical problems that make them immunosuppressed. 06:53 Any kind of recent neurosurgical procedure or a VP shunt. 06:57 A ventriculoperitoneal shunt, so a shunt that goes from the brain into the peritoneal cavity. 07:02 Those are generally used if a patient has an excess CSF or too much cerebrospinal fluid. 07:09 Now definitely in those patients, as you can imagine, if they've had their CSF or brain manipulated in anyway or if they have a foreign body in their brain system. 07:19 That make sense if that would pre-disposed you to meningitis. 07:24 Intravenous drug use, another thing that can predispose people to infections. 07:28 Definitely, if patients are using dirty needles to inject the drugs into their veins, that can predispose someone to getting a brain abscess or an infection around their brain that came from their blood stream. 07:42 And then closed quarters. 07:44 This is one of those things that can predispose to Neisseria, 'cause Neisseria can spread very rapidly and very quickly. 07:51 So anyone from a dorm or military barracks is key.
About the Lecture
The lecture Meningitis and Encephalitis (Emergency Medicine) by Sharon Bord, MD is from the course Neurologic and Psychiatric Emergencies.
Included Quiz Questions
Teenage students are recommended to get vaccinated for which of the following pathogens before living in dormitories?
- Neisseria meningitidis
- Listeria monocytogenes
- Haemophilus influenza
- Streptococcus pneumoniae
- Staphylococcus aureus
Which of the following statements regarding meningitis is FALSE?
- Meningococcal meningitis is most often seen in pregnant women.
- There has been a drastic decrease in the incidence of meningitis due to Haemophilus influenza after the introduction of the vaccine.
- Tuberculous is a rare cause of meningitis.
- Non-polio enterovirus is a very common cause of viral meningitis.
- Listeria causes meningitis in the very young and older population.
Which of the following is the most common cause of bacterial meningitis in children and adults in the United States?
- Streptococcus pneumoniae
- Staphylococcus aureus
- Haemophilus influenza
- Listeria monocytogenes
- Neisseria meningitidis
When is the most common time of year for viral meningitis?
- Late spring to fall
- Late fall to early winter
- Late winter to early spring
- Throughout the cold season
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |