Playlist
Show Playlist
Hide Playlist
Large Intestines: Colon Cancer
-
Slides Colon cancer General Surgery.pdf
-
Download Lecture Overview
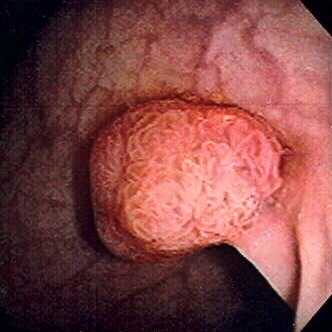
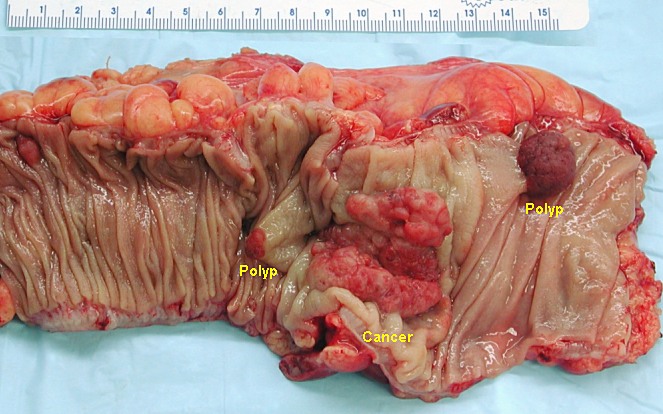
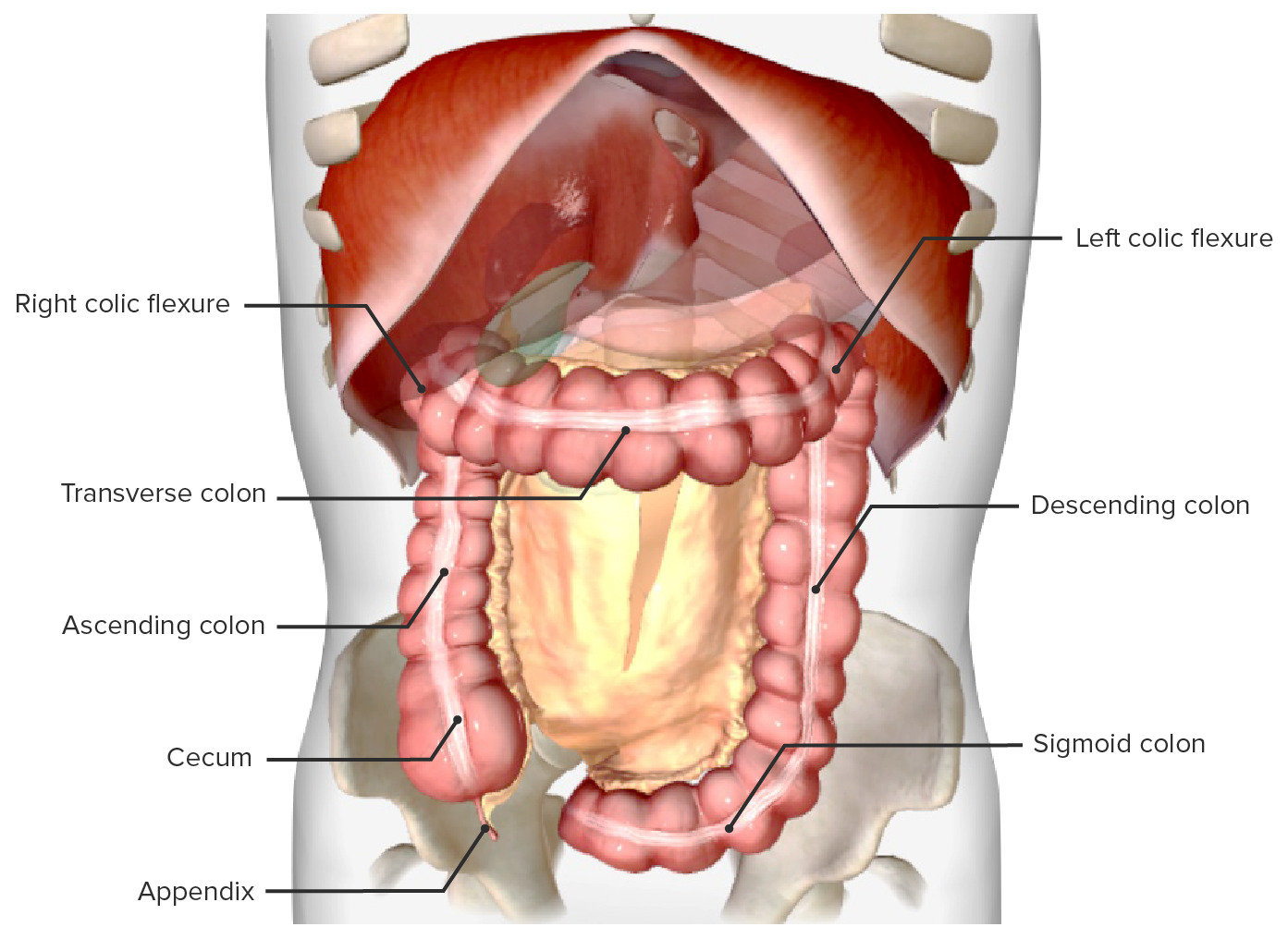
00:00 Welcome back, thanks for joining me on this discussion of colon cancer under the section of large intestines. 00:09 What are the causes of colon cancer? I'll give you a second to think about this. 00:16 Here's some very important colon cancer risk factors. 00:20 Low fiber, high fat diet, we call this the Western diet, there are very important hereditary syndromes to be aware of gene mutations from a polyp all the way to cancer in a predictable fashion. 00:35 And inflammatory bowel disease, including ulcerative colitis and Crohn's disease, ulcerative colitis and Crohn's disease will be covered in your medicine lectures. 00:47 Let's start with one of the very important syndromes hereditary nonpolyposis, colorectal cancer, HNPCC. 00:57 HNPCC are typically described as either Lynch Syndrome one or Lynch Syndrome two. 01:05 Lynch Syndrome one is an autosomal dominant phenotype and classically associated with a DNA mismatch repair gene MLH or MSH on your examination when presented with a particular DNA mismatch repair gene. 01:22 Look for these as the answers in Lynch syndrome two, it's similar to an autosomal dominant Lynch syndrome one, except that now you have extracolonic cancers, particularly endometrial or ovarian. 01:39 Petz-Jeghers, another important syndrome, autosomal dominant phenotype. 01:46 These are classically associated with hematomas which are benign in the GI tract, also associated with Mukulcutaneous pigmentation. 01:56 However, although the hematomas are benign, there is an increased risk of associated GI cancers, not derivatives of the hematomas. 02:09 How about familial adenomatous polyposis? These are multiple colon polyps and usually in the thousands. 02:18 There is a APC or adenomatous polyposis coli gene, which is a tumor suppressor gene mutation. 02:25 And as a reminder, in general, when a tumor suppressor gene mutation occurs, there's no tumor suppression. 02:33 Just like many of the other polyposis syndromes, this is also autosomal dominant in nature. 02:39 Typically, you'll find hundreds or thousands of polyps and there's almost 100% guarante of risk of colon cancer due to the pure volume of polyps. 02:48 Shortly we'll discuss the very predictable line of polyp to colon cancer and why often FAP patients will require surgery. 02:59 Gardner syndrome under high yield syndrome again associated with colon polyposis, this is considered a subset of familiar adenomatous polyposis that we just talked about, and the difference here is that it's a multiple polyposis syndrome that's associated with extra colonic manifestations such as Desmoid tumors, sebaceous cysts, lipomas and osteomas. 03:25 When you're presented with the clinical scenario that show extra colonic manifestations as well as polyposis, remember Gardner syndrome.
About the Lecture
The lecture Large Intestines: Colon Cancer by Kevin Pei, MD is from the course General Surgery.
Included Quiz Questions
All of the following are risk factors for colon cancer EXCEPT for?
- A Mediterranean diet
- A low fiber, high fat diet
- Ulcerative colitis
- Crohn's disease
- Familial adenomatous polyposis
Which of the following is TRUE about hereditary non-polyposis colon cancer?
- Lynch Syndrome 1 is associated with DNA mismatch repair gene mutations (MLH, MSH).
- Lynch Syndrome 1 is an autosomal recessive disease.
- Lynch Syndrome 2 causes colon cancer only.
- Lynch Syndrome 1 causes colon and ovarian cancers.
- Lynch Syndrome 2 is an X-linked dominant genetic disease.
Which statement is FALSE?
- Malignant gastrointestinal cancers in Peutz-Jeghers syndrome are mostly derived from benign hamartomas.
- There is an increased risk of gastrointestinal cancers in Peutz-Jeghers syndrome.
- There is an increased risk of gastrointestinal hamartomas in Peutz-Jeghers syndrome.
- Abnormal mucocutaneous pigmentation is a clinical sign often seen in Peutz-Jeghers syndrome.
- Peutz-Jeghers syndrome is an autosomal dominant disease.
A patient was diagnosed with Gardner Syndrome. Which of the following is not a classic extracolonic manifestation of this syndrome?
- Melanomas
- Sebaceous cysts
- Desmoid tumors
- Osteomas
- Lipomas
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Great Teacher Much Appreciated honestly, I have a surgery exam very soon so just recapping!