Playlist
Show Playlist
Hide Playlist
Ischemic Stroke: Treatment
-
Slides 01 Stroke Neuropathology I.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
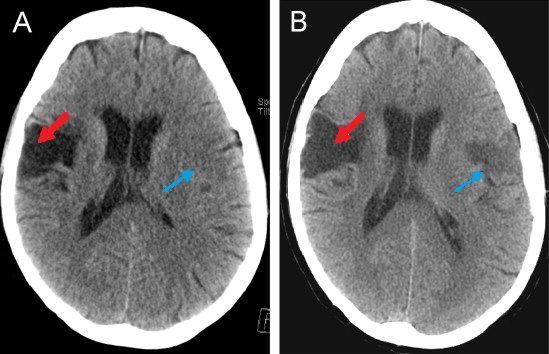
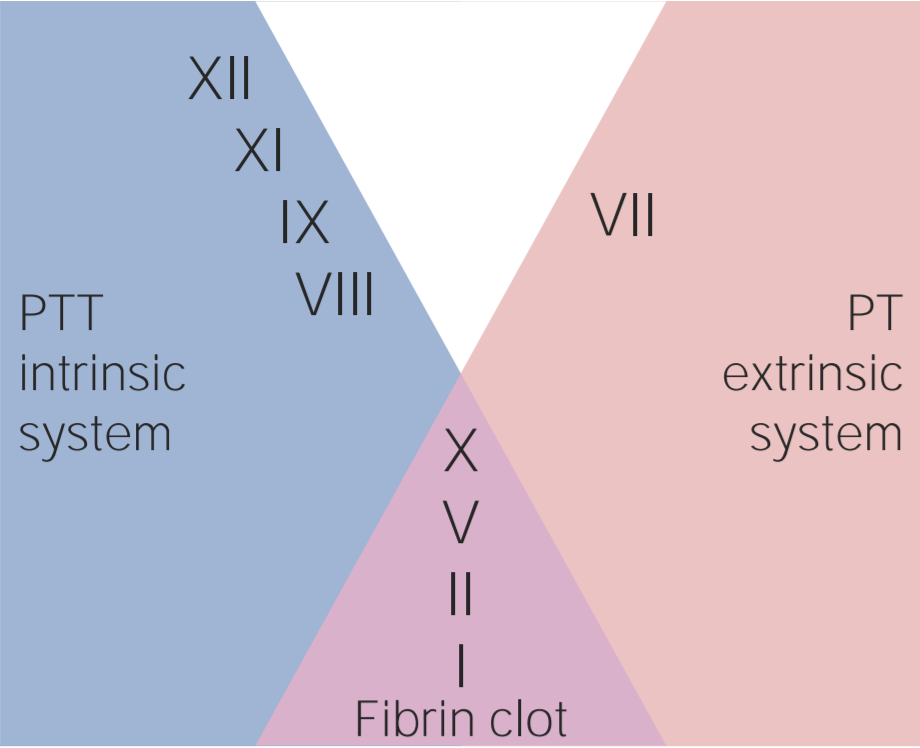
00:01 Now, what about the treatment for ischemic stroke? Well, in ABCs, you always want to make sure that you’re able to take care of the airway, the breathing, and circulation. 00:10 That’s always going to be the issue with stroke. 00:13 Now, with your blood pressure control, you want to keep in mind with systolic blood pressure between, let’s say, 180 and 220. 00:21 And then if it’s a diastolic blood pressure, you may be approximately 140 to about 120. 00:27 You want to be less than that so that you’re able to manage your patient who has suffered a stroke. 00:34 Antiplatelet therapy, aspirin. 00:36 Anticoagulation. If, if, the patient luckily is the hospital, heparin has to be instituted and helps and hurts, only used in atrial fib and dissection. 00:48 So be careful. 00:49 If your patient is already in a state of vulnerability, is already in the state of maybe bleeding, and if your patient is not suffering from atrial fibrillation or dissection, then be really careful with heparin. 01:04 It’s rapidly acting, works through antithrombin III. 01:07 And it might actually hurt the patient, may result in a hemorrhagic stroke, so be careful with heparin, please. 01:12 Also, thrombolytics. 01:14 I’m going to walk you through tPA, very, very important. 01:18 And I want to walk you through this. 01:19 I’m going to walk you through a great detail as to the contraindications for TPA that you must know for your boards. 01:28 And then rehab. 01:30 I promised you that we’d come back to the indications for tissue plasminogen activator. 01:38 Remember that the physiology behind your tPA is the fact that plasmin is an “enzyme” that breaks down your fibrin clot very, very quickly. 01:51 In other words, it’s a thrombolytic agent physiologically or homeostatically. 01:57 And of course, we used this to our advantage in which we can then try to break down our clot very quickly. 02:03 And we have discussed this earlier with myocardial infarction. 02:07 And earlier, we talked about streptokinase, alteplase, your -ase drugs. 02:14 You’re worried about reperfusion injury. 02:16 Now, here with tPA, remember now we’re trying to break down a clot that may then be resulting in ischemic stroke. 02:23 So the indications kind of seem similar, don’t they? But, a huge but, are going to be the list of contraindications that I’m about to give you. 02:31 The criteria is pretty straightforward. 02:33 Clinical diagnosis of ischemic stroke for all the different reasons we’ve talked about. 02:38 Your patient has to be older, greater than 18. 02:42 Now, here, this is important. 02:47 Time to tPA administration, less than 4.5 hours from the onset of the symptoms. 02:54 So this is where your imaging studies are going to become incredibly crucial. 02:59 Granted in current day practice, there are many, many advancements in imaging and such. 03:05 But at this point, something that I walked you through is the noncontrast CT and where, for example, I gave you middle cerebral artery type of stroke and what it means from one hour. 03:17 So really pay attention to 4.5 hours, please, with tPA. 03:23 Now, the head CT, without contrast, things that you want to make sure that you identify is has there been a hemorrhage? What about the size of the stroke? And if that size of the stroke is rather large and there’s a lot of hyperdense area on that head CT, then you want to start maybe questioning whether or not you want to use your tPA. 03:48 Or if there’s hemorrhage taking place. 03:50 Remember, tPA is already going to break down the clots. 03:53 So you’re already increasing the risk of hemorrhage taking place. 03:57 And if you indentify evidence for a hemorrhage, then you really want to be careful by using tPA. 04:03 Now, let’s walk into the all important contraindications. 04:07 There’s a large list here and I’d recommend that you spend some time making sure that you know these. 04:12 Now, clinical judgement of using tPA is different from doctor to doctor, neurosurgeons, so on and so forth. 04:20 But what I can speak to you about is going to be the facts of when it’s contraindicated to use tPA and these you want to make sure that you commit to memory. 04:32 Stroke or serious head trauma in the last three months. 04:36 Once again, you want to worry about hematomas that are taking place. 04:39 Remember, whenever there is a trauma that’s taking place with the head, they could be multiple causes as we shall see. 04:46 History of intracranial hemorrhage or AV malformations. 04:49 If there’s already a history of bleeding taking place in your patient, then you want to make sure that you avoid tissue plasminogen activator. 04:58 This is a list of contraindications. The list prior was a list of criteria Myocardial infarction in the past six weeks. 05:06 Be careful. Contraindicated to use tPA. 05:10 Major surgery or trauma in the last two weeks. 05:12 GI or urinary tract hemorrhage in the last three weeks. 05:16 So you want to make sure that you evaluate your patient for hemorrhage up and down the body because you’re never quite sure as to how vulnerable your patient is to hemorrhage because you’re worried about the potency of tPA because it is extremely effective. 05:34 Lumbar puncture or your arterial puncture at non-compressible site in the last week, tPA will be contraindicated. 05:43 And aggressive blood pressure therapy is absolutely required prior to using tPA. 05:49 And if that blood pressure, we talked about indications for systolic and diastolic blood pressure, and if that is not controlled, then please make sure that tPA is carefully, if at all, administered. 06:03 Other contraindications. 06:05 Continuing our discussion, if there’s elevated PT, let’s say above 15 seconds or above 40 seconds for PTT, contraindicated. 06:14 Platelet count. if there isn’t enough platelets, you start dropping down below 100,000s, specifically 50,000, contraindicated. 06:24 And glucose, either hypo or hyperglycemic, less than 40, greater than 400, give yourself a range. 06:32 Pregnancy, tPA contraindicated. 06:34 There is something called the NIH scale and remember that scale that I walked you through just a little bit and I told you, "Get an idea." If it’s less than 4 or greater than 22, then tPA will be contraindicated. 06:49 Improving symptoms. 06:50 If your patient is recovering from the stroke, then you probably don’t want to give tPA at this point. 06:56 You monitor your patient very closely. 07:00 And then seizure at onset. 07:03 Oftentimes and we’ll talk about this later on when we talk about seizures and epilepsy and when we do, whenever there is seizure type of symptoms, then you try to avoid tPA, please. 07:15 Secondary preventions, so at this point, we’ve closed our discussion of tPA. 07:22 We’ve talked about the criteria and more importantly, we’ve walked through some very important contraindications. 07:27 Let’s do secondary prevention. 07:29 Antiplatelet agent, aspirin or you’ve heard of clopidogrel. 07:34 It’s your ADP inhibitor from your platelet so that you do not express your glycoprotein IIb/IIIa. 07:40 And you probably know this as a generic – Your trade name is Plavix or there’s another one called Aggrenox, and that is your dipyridamole. 07:50 These are antiplatelet agents. 07:52 Anticoagulation. 07:54 Once again, remember, atrial fibrillation. 07:55 We’ve discussed this plenty. 07:58 And here, to make sure that you prevent an embolization type of ischemic stroke, you’ll be using anticoagulation. 08:06 Remember the carotid artery, a common site for maybe atherosclerosis. 08:10 And so therefore, whatever that might be taking place within the coronary artery could also be taking place within the carotid. 08:17 And so therefore, whatever that you would be conducting in the coronary is something that you want to take care of here in the carotid. 08:24 Endarterectomy in appropriate patients and greater than 70% stenosis. 08:29 Remember, kind of behaves like the discussion that we had with angina, right? When you start getting into – In the carotid artery though, a little bit more dangerous. 08:40 In the coronary artery, remember 70% or so stable angina, 90% you get into unstable angina. 08:46 But in the carotid though, 70% is something that you very much want to keep in mind and consider with the amount of stenosis taking place. 08:55 Endarterectomy. 08:56 Smoking cessation. 08:58 Control the diabetes. 08:59 Hypertension control. 09:00 Cholesterol control. 09:01 The rest of these make perfect sense. 09:03 These are preventive measures. 09:05 Please make sure that you’re well-versed with prevention. 09:09 What’s the best type of medicine? Prevention. 09:12 Treatment? Unfortunately is where we stand today. 09:16 But as you know, the medical world is moving towards prevention, which is nice to know. 09:21 So in summary with ischemic stroke, remember the risk factors we’ve talked about. 09:25 We’ve talked about age, gender. 09:26 We’ve talked about hypertension being a very important, very important risk factor. 09:31 Diabetes. 09:32 Genetically, we talked about the autosomal dominant condition called CADASIL. 09:36 Also, hypercoagulable states. 09:38 Preventive medicine, important. 09:40 Here, if you know that your patient is at risk for stroke, then try to treat the underlying issue. 09:48 Once again, look at those antiplatelet agents. 09:51 Remember the carotid artery, if you find that the blood flow through the carotid artery is decreased, then perhaps endarterectomy is warranted. 10:01 Secondary, treat the underlying condition. 10:03 Once again, what we talked about earlier. 10:06 Signs and symptoms. 10:07 Well, here, focal weakness, sensory changes, ataxia, vertigo, language difficulty. 10:13 Well, all the symptoms that you can expect for an ischemic type of stroke. 10:17 So now, before we absolutely close the chapter on ischemic stroke, remember, under stroke, you can have it as being focal or global and this point, we’ve focused primarily on focal. 10:29 Under focal, approximately 80-85% will be of ischemic type . 10:34 and then you have a smaller percentage of hemorrhagic type. 10:38 We’re summarizing ischemic. 10:40 Differential diagnosis could be hemorrhagic. 10:43 Then you have something called Todd’s paralysis, seizures-associated, metabolic disorders, complicated migraines, all differentials. 10:53 Acute and post acute diagnostic workup, we talked about that head CT. 10:57 We talked about echo, MRI, carotid type of ultrasound to make sure how much stenosis is taking place in the carotids. 11:06 Treatment, we’ve talked about the antiplatelet therapies. 11:08 We’ve talked about the great extent of tPA and keep in mind, in general, anticoagulation.
About the Lecture
The lecture Ischemic Stroke: Treatment by Carlo Raj, MD is from the course Stroke (Cerebrovascular Accident). It contains the following chapters:
- Treatment of Ischemic Stroke
- Tissue Plasminogen Activator - tPA
- Secondary Prevention
- Ischemic Stroke: Summary
Included Quiz Questions
What is TRUE regarding the administration of tPA in the treatment of ischemic stroke?
- Elevated PT/PTT is a contraindication for tPA administration.
- With seizure-type symptoms, it is safe to give tPA.
- It inhibits the extrinsic pathway.
- It can be administered in pregnancy.
- It is available in oral and IV forms.
A patient presents with right arm weakness and aphasia that started eight hours ago, and a head CT reveals no evidence of hemorrhage. A clinical diagnosis of ischemic stroke is made, but tPA administration is withheld. What is the reason for withholding tPA treatment in this patient?
- The elapse of time from the onset of symptoms
- Inadequate blood pressure control
- History of IV drug abuse
- Head CT finding
- Clinical diagnosis
What is one of the contraindications to tPA administration in stroke?
- History of stroke in the last 12 weeks
- History of myocardial infarction 8 weeks ago
- History of motor vehicle accident 2 months ago
- History of lumbar puncture 12 weeks ago
- History of urinary tract infection in the last 3 weeks
What is one of the drugs used in the prevention of stroke?
- Aspirin
- Tissue plasminogen activator (tPA)
- Heparin
- Beta-blockers
- Insulin
What is one of the criteria for tPa for a patient presenting with an acute stroke?
- Onset of symptoms less than 4.5 hours
- Age > 50
- Blood pressure < 140/90
- BMI < 35
- No prior history of stroke
Customer reviews
4,0 of 5 stars
| 5 Stars |
|
0 |
| 4 Stars |
|
1 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
I enjoyed the series on ischaemic stroke but it would have been great to discuss in more depth the secondary management of stroke in particular blood pressure targets and agents with the most supportive evidence for use (e.g ACE-I). I also note that there was an omission about the best way to manage BP in the acutely hypertensive patient post stroke. Despite theses as always good taster of the topic. I appreciate the challenge of work that goes into producing these contents