Playlist
Show Playlist
Hide Playlist
Invasive Ductal Carcinoma (IDC)
-
Slides MalignantBreastDiseases Surgery.pdf
-
Download Lecture Overview
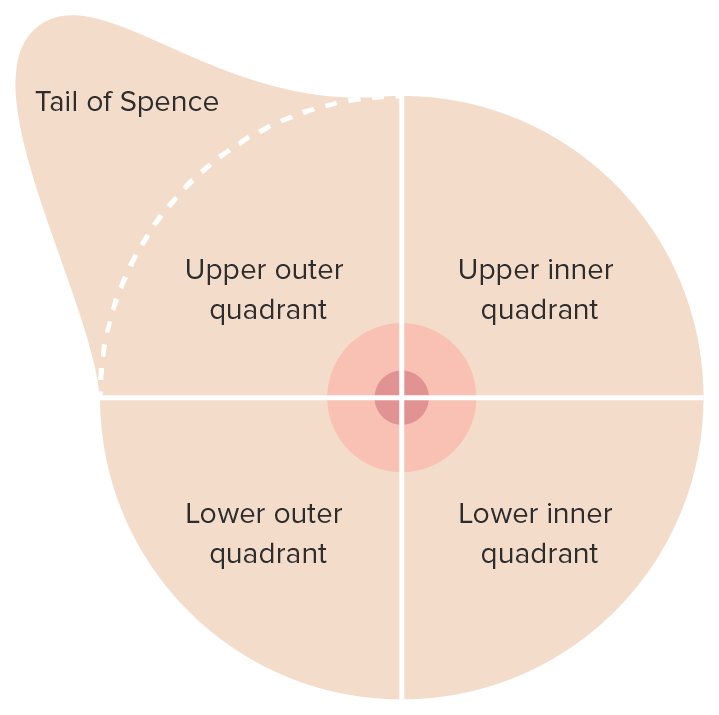
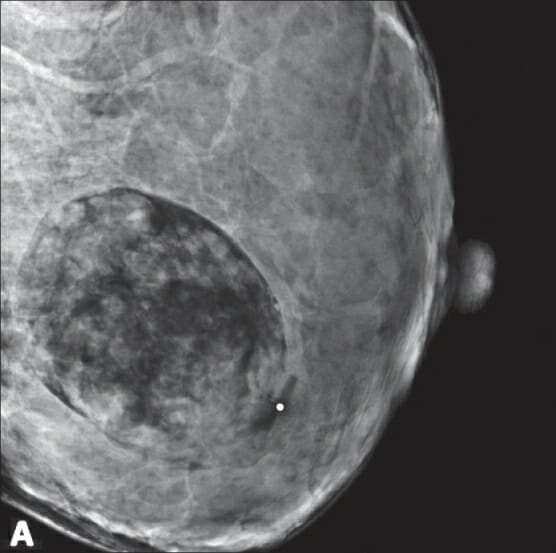
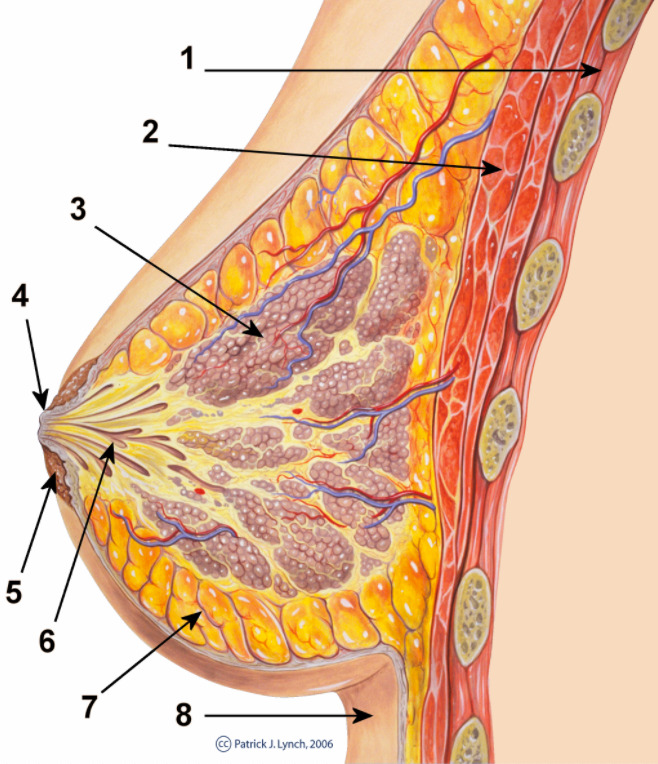
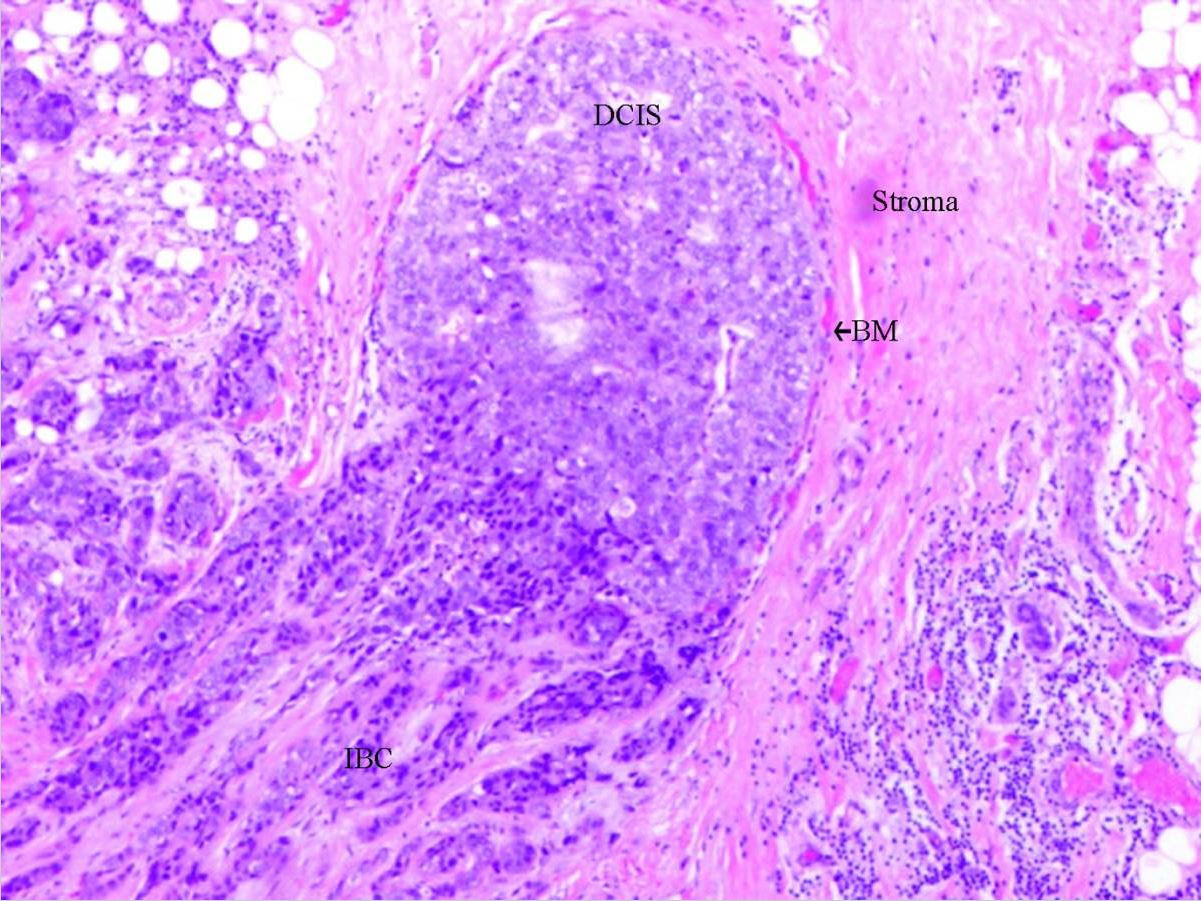
00:01 Now, let’s move on to a discussion of infiltrating ductal carcinoma. These patients unfortunately have cancer that have evaded beyond the ducts. What are some of the risk factors? Women clearly, now remember, men can also get breast cancer; older women; genetic mutations such as BRCA or BRCA 1 and 2; early menstrual period, late or never pregnant; and patients who have had estrogen replacement therapy. Overaching theme of the last three risk factors increases one's duration of estrogen receptor stimulation. Here’s the imaging of infiltrating ductal carcinoma. 00:44 You might recall this image looks very similar to our ductal carcinoma in-situ. Again to reiterate, it is often very difficult to distinguish based on mammogram alone. So, if it’s palpable, we can do a needle core biopsy. Again, if not palpable, we can do a 3D image-guided stereotactic biopsy. 01:04 But tissue diagnosis is absolutely necessary. If your tissue diagnosis comes back negative or doesn’t show any cancer, we may actually have to proceed to a surgical excisional biopsy because of the suspicious lesion on mammogram. One should not settle for the first set of biopsies if they're not congruent with your clinical suspicions. For infiltrating ductal carcinoma, cancer operation is offered. 01:34 Again, patients are often eligible for breast conservation therapy including the local excision, postoperative radiation, and again the results are similar to a mastectomy. Some patients, once again choose a mastectomy and that’s a personal decision between the patient and the surgeon. 01:54 Now, let’s go on to a discussion of sentinel lymph node biopsies. Recall when I said the importance of assessing the lymph node draining basins. Lymph node status is of utmost importance in prognostic value for breast cancer. Female breast and adjacent lymph nodes and lymph vessels drain on a very predictable manner, generally into the supraclavicular, behind the pectoralis, and into the axilla. Sentinel lymph node biopsy allows us to detect the first several draining lymph nodes. The chances are if the first several lymph nodes do not contain cancer, it’s unlikely that the rest of the basin contains breast cancer. The idea behind sentinel lymph node biopsy is that traditionally, removing the entire armpit axilla of lymph node tissue has been a very, very morbid procedure. Let’s move on to a different entity. Allow me to pose a question to you. 02:51 What if the pathology is lobular carcinoma in-situ? What would you do at that point? I’ll give you a second to think about this. Lobular carcinoma in-situ is a noninvasive lesion in lobules and terminal ducts. It is almost always an incidental finding. And excisional biopsy is recommended to exclude malignancy. Some opt for double mastectomy because lobular carcinoma in-situ infers increased risk of cancer. We can offer chemopreventative therapy using selective estrogen receptor modulators or aromatase inhibitors. Here are some very important take-home messages, clinical pearls, and high-yield information. Remember, if breast conservation therapy is offered to a patient, radiation must follow. If the patient is not candidate for radiation or chooses not to have radiation, you as the clinician should not offer breast conservation therapy. For patients with the diagnosis of lobular carcinoma in-situ, remember it confers increased risk of invasive ductal carcinoma even in the contralateral breast. Remember, patients sometimes choose double mastectomies to decrease the risk of breast cancer or can have estrogen modulators. 04:14 Thank you very much for joining me on this discussion of malignant breast diseases.
About the Lecture
The lecture Invasive Ductal Carcinoma (IDC) by Kevin Pei, MD is from the course General Surgery.
Included Quiz Questions
Which of the following patients has the highest risk for invasive ductal carcinoma?
- A post-menopausal 61-year-old woman with menarche at age 11 and has never been pregnant.
- A post-menopausal 58-year-old woman with menarche at age 15 and has never been pregnant.
- A pre-menopausal 58-year-old woman with menarche at age 15 and has never been pregnant
- A post-menopausal 60-year-old woman with menarche at age 12 and a history of 3 term pregnancies.
- A pre-menopausal 45-year-old woman with menarche at age 16 who has a history of 2 term pregnancies.
Which of the following is NOT a risk factor for invasive ductal carcinoma?
- Late menarche
- Genetic mutations BRCA 1 and 2
- History of post-menopausal estrogen replacement therapy
- Age greater than 50
- No pregnancies
A 63-year-old woman who has a sister with a history of breast cancer presents to the clinic with a concern over a palpable lump in her breast. A mammogram confirms the suspicion of an abnormal lesion in the left breast. What is the next most appropriate step in management?
- Core needle biopsy
- Stereotactic biopsy
- Surgical excision
- Local excision of the lesion followed by post-operative radiation
- Sentinel lymph node biopsy
A 58-year-old woman is confirmed to have invasive ductal carcinoma on biopsy of her right breast. In consultation with her physicians, she makes it clear that she is opposed to getting radiation therapy due to her fear of side effects. What is the most appropriate treatment option for this patient?
- Right mastectomy and sentinel lymph node biopsy
- Bilateral mastectomy
- Breast conservation therapy
- Wide excision of the lesion and sentinel lymph node biopsy
- Wide excision of the lesion followed by chemotherapy
Which of the following statements is true about a patient found to have a non-invasive lesion in the lobules and terminal ducts of the right breast?
- She has an increased risk of invasive ductal carcinoma in either breast.
- She has an increased risk of invasive ductal carcinoma in the right breast only.
- It is recommended to monitor the lesion for growth by imaging every 6 months for the next 3 years.
- She should have a right-sided mastectomy and axillary lymph node dissection to reduce her risk of invasive malignancy in the future.
- Chemopreventative treatment with a selective estrogen receptor modulator is not sufficient risk reduction without a bilateral mastectomy first.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |